Play all audios:
ABSTRACT _PURPOSE_ To ascertain the therapeutic effect of periocular corticosteroids in diabetic papillopathy. _METHODS_ Prospectively, five consecutive adult-onset diabetic patients with
symptomatic diabetic papillopathy underwent visual fields and fluorescein angiography before and after superonasal subtenon injection of corticosteroids. _RESULTS_ The median duration of
papillopathy was 2.5 weeks by ophthalmoscopy and 3 weeks by fluorescein angiography. The median recovery time of best-spectacle-corrected visual acuity was 2 weeks. Two patients developed
sequential diabetic papillopathy, and both reported faster visual recovery and better subjective vision in treated eyes. In these two patients, the final best-spectacle-corrected visual
acuity and visual evoked responses were comparable between the two eyes, while automated visual fields were less constricted in treated eyes. Complications included ocular hypertension, mild
progression of cataract, and mild ptosis in one patient each. _CONCLUSIONS_ Periocular corticosteroids shortened the duration of diabetic papillopathy from a reported median of 5 months to
3 weeks in the present uncontrolled observational study, partly by their angiostatic and antioedema effects at the level of the anterior optic nerve. Intraocular pressure needs to be
monitored in eyes receiving periocular corticosteroids. SIMILAR CONTENT BEING VIEWED BY OTHERS WHAT HAVE WE LEARNED FROM A DECADE TREATING PATIENTS WITH DIABETIC MACULAR OEDEMA WITH 0.19 MG
FLUOCINOLONE ACETONIDE INTRAVITREAL IMPLANT? Article Open access 19 February 2025 CLINICAL EFFICACY AND SAFETY OF INTRAVITREAL FLUOCINOLONE ACETONIDE IMPLANT FOR THE TREATMENT OF CHRONIC
DIABETIC MACULAR OEDEMA: FIVE-YEAR REAL-WORLD RESULTS Article 13 December 2022 INTRAVITREAL RANIBIZUMAB REDUCED OCULAR BLOOD FLOW AND AQUEOUS CYTOKINE LEVELS AND IMPROVED RETINAL MORPHOLOGY
IN PATIENTS WITH DIABETIC MACULAR EDEMA Article Open access 10 December 2020 INTRODUCTION Acute disc swelling with superficial, dilated, radially oriented, fluorescein-incontinent
capillaries1, 2, 3, 4, 5 was initially described in long-standing juvenile diabetic patients, many being asymptomatic, or having simultaneous bilateral disease. Diabetic papillopathy lasted
several months, and resolved with mild to moderate visual loss.3, 6, 7 Periocular corticosteroids were used to treat intermediate or posterior uveitis,8 optic disc neovascularization from
chronic uveitis,9 rubeosis iridis,10 cystoid macular oedema,11 and arteritic ischaemic optic neuropathy.12 We investigated the effect of periocular corticosteroids on the duration of
diabetic papillopathy. MATERIALS AND METHODS Six eyes of five consecutive adult-onset diabetic patients attending a referral clinic (AMM) over a 6-month period (August 2002–January 2003)
were treated for diabetic papillopathy (one patient was uniocular and four patients had bilateral disease) (Table 1). Eyes were diagnosed with diabetic papillopathy if the disc was swollen
with superficial telangiectatic radial vessels, fluorescein angiography did not show delay in either onset or time to completion of prelaminar optic disc filling, a positive history of
diabetes mellitus, and a negative history of temporal arteritis and pseudotumour cerebri. Treatment consisted of injecting corticosteroids (5 mg betamethasone dipropionate and 2 mg
betamethasone sodium phosphate in 2 ml, Schering-Plaugh, USA) in the superonasal subtenon space. The Ethics Committee of Khoury Hospital approved the therapy that was administered after
informed patient consent. The potential side effects of corticosteroid injections and the investigational nature of the therapy were thoroughly explained. CASE REPORTS _Case 1_. This
68-year-old white woman presented with sudden visual loss in the right eye. Systemic history included diabetes mellitus of 20 years, systemic hypertension, coronary artery disease, and prior
coronary bypass surgery. Examination of the right eye revealed a best-spectacle-corrected visual acuity of 6/60, diffuse disc oedema and peripapillary retinal venous dilation. After 2
weeks, visual acuity improved to 6/15 with decrease in disc oedema. She developed a similar attack in the left eye 6 weeks after presentation. Best-spectacle-corrected visual acuity in the
left eye was 6/120. The left optic disc was elevated and hyperaemic with flat dilated superficial capillaries, peripapillary nerve fibre layer haemorrhages, and mild cystoid macular oedema.
The right optic disc was pale. She consented to periocular injection of corticosteroids in the left eye. After 1 week, visual acuity improved to 6/9 with marked decrease in disc oedema. At 2
weeks after injection, visual acuity in the left eye was 6/6 with resolution of disc and macular oedema. The right disc was pale, small in size, and with an effaced cup. The right eye
underwent periocular injection of corticosteroids for mild cystoid macular oedema. At 4 weeks after presentation, the visual acuity was 6/6 bilaterally, without an afferent pupillary defect.
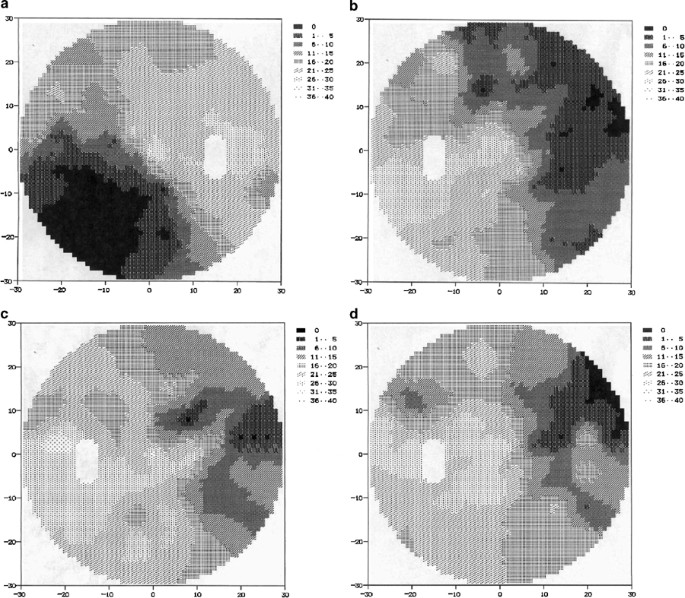
Visual fields revealed severe constriction bilaterally more pronounced in the right eye, and decreasing after therapy in the left eye (Figure 1). Pattern visual evoked responses had
comparable waveforms in both eyes (normal latency and mild attenuation of the amplitudes). Colour vision revealed mild red–green deficiency in the right eye only by H–R–R pseudo-isochromatic
plates (American Optical, USA, 2d ed, 1957). There was no change in visual acuity, appearance of disc and macula, and visual fields bilaterally till the last follow-up, 7.5 months after the
onset of papillopathy in the left eye. _Case 2_. This 50-year-old white man with diabetes mellitus of 10 years presented with sudden visual loss in the right eye. He had an afferent
pupillary defect in the right eye. The best-spectacle-corrected visual acuity was counting finger at 3 meters in the right eye and 6/6 in the left eye. Funduscopy revealed marked swelling of
the right optic disc, and preproliferative diabetic retinopathy changes bilaterally. He underwent panretinal laser photocoagulation to the right eye. At 2 weeks after laser, the disc oedema
decreased, and visual acuity stabilized at the 6/24 level. At 7 months after initial presentation, the patient underwent panretinal laser photocoagulation to the left eye. At 2 months after
laser therapy, he developed severe visual loss in the left eye to counting finger 2 m. The left optic disc was diffusely swollen with telangiectatic vessels. He received periocular
corticosteroids in the left eye. The patient reported marked visual improvement 2 weeks after injection. At 4 weeks after injection, best-spectacle-corrected visual acuity in the left eye
was 6/60 with resolved disc oedema. Intravenous fluorescein angiography demonstrated an absence of disc leakage in the left eye. Macular oedema was absent bilaterally. Both discs were small
in size and had an effaced cup. At 10 weeks after visual loss in the left eye, best-spectacle-corrected visual acuity was 6/12 bilaterally, with a right afferent pupillary defect. Automated
visual fields showed severe constriction bilaterally more pronounced in the right eye (Figure 2). Pattern visual evoked responses had comparable waveforms in both eyes (normal latency and
mild attenuation of the amplitudes). Both eyes failed to recognize any colour plate using the H–R–R pseudo-isochromatic plates. The optic nerve appearance, fovea, and visual fields were
bilaterally unchanged 22 and 34 weeks after the onset of papillopathy in the left eye. _Case 3_. This 47-year-old white man with diabetes mellitus for 12 years noted sudden visual loss in
the left eye. Best-spectacle-corrected visual acuity was 6/15 in the left eye with elevation of the optic disc superiorly, background diabetic retinopathy, and a normal-appearing fovea. He
had a large inferior arcuate visual field defect in the left eye. Colour vision was positive for medium red–green defect bilaterally by the H–R–R pseudo-isochromatic plates. Profuse disc
leakage of fluorescein dye was noted bilaterally. There was a diffuse perivascular dye leakage from dilated capillaries throughout the posterior pole, reminiscent of VEGF retinopathy
model.13 The patient consented to periocular injection of corticosteroids in the left eye. After 5 later, best-spectacle-corrected visual acuity improved to 6/9. After 11 days later,
best-spectacle-corrected visual acuity was 6/9 with resolution of disc oedema. Visual fields were unchanged. There was marked decrease in disc leakage in the left eye by fluorescein
angiography. At 3 weeks after presentation, best-spectacle-corrected visual acuity was 6/6 in the left eye. Intraocular tension rose to 30 mmHg, and was controlled by topical antiglaucoma
medication. The status of optic disc and macula in both eyes were unchanged 20 and 24 weeks after the onset of papillopathy. Visual field defects decreased in the left eye 24 weeks after
presentation. A 1-mm asymptomatic left ptosis was noted. _Case 4_. This 77-year-old white woman with diabetes mellitus of 20 years noted sudden visual loss in the left eye.
Best-spectacle-corrected visual acuity was 6/15 in the right eye, and finger counting 1 m in the left eye. The disc was swollen superiorly in both eyes. There was focal superior leakage in
the right disc and diffuse severe leakage in the left disc. There was mild cystoid macular oedema in the left eye. Visual fields showed severe contraction of the central field in the left
eye and superior arcuate defect in the right eye. The patient underwent bilateral periocular injection of corticosteroids. At 9 days after injection, best-spectacle-corrected visual acuity
was 6/9 in the right eye and finger counting 3 m in the left eye. Disc oedema and macular oedema decreased bilaterally. At 15 days after presentation, best-spectacle-corrected visual acuity
was 6/9 and finger counting at 4 m. Disk leakage decreased markedly in both eyes on repeat fluorescein angiography (Figure 3). The diffuse visual field defects decreased markedly in both
eyes. Posterior pole examination and visual fields were unchanged 10 and 23 weeks after presentation, with best-spectacle-corrected visual acuity of 6/360 in the left eye. Mild cataract
progression was noted bilaterally 24 weeks after therapy. _Case 5_. This 65-year-old uniocular white woman with diabetes mellitus of 18 years noted sudden visual loss in the left eye.
Best-spectacle-corrected visual acuity was finger counting at 2 m in the left eye with diffuse disc oedema, cystoid macular oedema, and background diabetic retinopathy changes. She received
periocular injection of corticosteroids. Fluorescein angiography showed early marked disc leakage. She had complete obliteration of central and nasal fields with islands of temporal fields
remaining. At 2 weeks after injection, best-spectacle-corrected visual acuity was finger counting at 3 m, with resolution of disc oedema, absence of disc leakage on fluorescein angiography,
and improvement in central visual field. Best-spectacle-corrected visual acuity stabilized at 6/120 and visual fields were unchanged 4, 7, 14, and 17 weeks after presentation. Summary of
case reports was tabulated (Table 1). The median duration of papillopathy in treated eyes was 2.5 weeks by 90-D slit-lamp examination, and 3 weeks by fluorescein angiography (Figure 3).
Best-spectacle-corrected visual acuity was attained at a median of 2 weeks after therapy. Macular oedema resolved in all treated eyes. Visual field defects decreased in treated eyes after 2
weeks of therapy and stayed stable thereafter (Figures 1 and 2). Ocular hypertension, mild cataract progression, and asymptomatic minimal ptosis occurred, noted in one patient each. Cases 1
and 2 had sequential papillopathy with the right untreated eye and the left treated eye. Both reported repeatedly ‘seeing better’ in the treated eye, and both had similar
best-spectacle-corrected visual acuity in either eye, comparable pattern visual evoked responses (latency and amplitude) in either eye, but denser scotomas on visual fields in untreated eyes
(Figures 1 and 2). DISCUSSION Lubow and Makley2 initially described diabetic papillopathy in 1971. Visual acuity was moderately reduced and tended to improve spontaneously. Relative
pupillary defects and dyschromatopsia were atypical.6 Visual field defects included enlarged blind spots, generalized constriction, and arcuate scotomas.3, 6, 7 Disc oedema was often diffuse
with hyperoemia. Diabetic papillopathy was considered one form of nonarteritic anterior ischaemic optic neuropathy, with special characteristics: long duration of disc oedema, mild
to-moderate initial visual loss, relatively mild-to-moderate optic nerve dysfunction, and good visual recovery. Unlike nonarteritic ischaemic optic neuropathy,14 fluorescein angiography in
diabetic papillopathy does not show delay in either onset or time to completion of prelaminar optic disk filling. By combining two large series with adult-onset diabetes mellitus (51 eyes of
35 patients6, 7), the median duration of papillopathy was 5 months. The aetiology of diabetic papillopathy included a combination of reversible microangiopathy15 and structural factors
(small disc or small cup–disc ratio).6 Several patients in the present study had poor initial visual acuity. More than 30% of reported patients with diabetic papillopathy3, 6, 7, 16, 17 (16
out of 52 patients) had initial visual acuities below or equal to 6/30 as follows: two patients had 6/30, eight patients had 6/60, and six patients had less than 6/60. The antioedema and
angiostatic effects of corticosteroids may explain the resolution of disc oedema in the present cases. Intraocular and periocular corticosteroids reduced the breakdown of blood–retinal
barrier18 partly by downregulating the production of vascular permeability growth factor, also known as vascular endothelial growth factor (VEGF).19, 20, 21, 22 Periocular corticosteroids
reached the posterior segment of the eye experimentally19, 20, 23, 24 and clinically.21, 22 Superonasal injections allowed a high drug concentration around the optic nerve head,23 while
superotemporal injections allowed a high drug concentration around the macular region.25 Early decongestion of small optic nerve head could decrease the damage to peripapillary axons and
minimize subsequent optic atrophy. The rapid visual recovery in our uncontrolled observational study could have been spontaneous, unrelated to therapy. Similarly, in the two patients with
sequential papillopathy, the patients' impression of better vision in the treated eye could be attributed to a placebo effect. Macular oedema was a frequent associated finding with
diabetic papillopathy, being detected in 70% of eyes.6 Macular oedema in diabetic papillopathy resulted from leakage of abnormal disc vessels.17 By stabilizing the blood–ocular barrier at
the disc17 and macula (Figure 3), periocular corticosteroids resulted in resolution of macular oedema in the present case series. Complications of periocular corticosteroids included ocular
hypertension,26 cataract,27 ptosis,27 inadvertent rupture of the globe,28 systemic toxicity29 and uncontrolled hyperglyecamia. Periocular corticosteroids are not advised in eyes with chronic
open-angle glaucoma and in steroid-responsive eyes. In these eyes, periocular (or intravitreal) injection of anti-VEGF EYE00130 or angiostatic steroids (anecortave acetate,31 budesonide19)
or bucillamine (antirheumatic drug),20 and hyperbaric therapy32 could be considered in the future. Besides these modalities, tight blood sugar control, blood pressure regulation,
anticoagulation, regular exercise, and good hydration need to be considered in the initial management of diabetic papillopathy. REFERENCES * Whittaker KW, Mehta JS, Tsaloumas MD . Bilateral
diabetic papillopathy associated with optic disc neovascularisation. _Eye_ 2000; 14: 914–915. Article CAS Google Scholar * Lubow M, Makley TA . Pseudopapilledema of juvenile diabetes
mellitus. _Arch Ophthalmol_ 1971; 85: 417–422. Article CAS Google Scholar * Barr CC, Glaser JS, Blankenship G . Acute disc swelling in juvenile diabetes. Clinical profile and natural
history of 12 cases. _Arch Ophthalmol_ 1980; 98: 2185–2192. Article CAS Google Scholar * Appen R, Chandra S, Klein R, Myers F . Diabetic papillopathy. _Am J Ophthalmol_ 1980; 90: 203–209.
Article CAS Google Scholar * Pavan PR, Aiello LM, Wafai MZ, Briones JC, Sebestyen JG, Bradbury MJ . Optic disc oedema in juvenile-onset diabetes. _Arch Ophthalmol_ 1980; 98: 2193–2195.
Article CAS Google Scholar * Regillo CD, Brown GC, Savino PJ, Byrnes GA, Benson WE, Tasman WS _et al_. Diabetic papillopathy. Patient characteristics and fundus findings. _Arch
Ophthalmol_ 1995; 113: 889–895. Article CAS Google Scholar * Bayraktar Z, Alacali N, Bayraktar S . Diabetic papillopathy in type II diabetic patients. _Retina_ 2002; 22: 752–758. Article
Google Scholar * Helm CJ, Holland GN . The effects of posterior subtenon injection of triamcinolone acetonide in patients with intermediate uveitis. _Am J Ophthalmol_ 1995; 120: 55–64.
Article CAS Google Scholar * Sanislo SR, Lowder CY, Kaiser PK, Gutman FA, Zegarra H, Dodds EM _et al_. Corticosteroid therapy for optic disc neovascularization secondary to chronic
uveitis. _Am J Ophthalmol_ 2000; 130: 724–731. Article CAS Google Scholar * Ehrenberg M, McCuen II BW, Schindler RH, Machemer R . Rubeosis iridis: preoperative iris fluorescein
angiography and periocular steroids. _Ophthalmology_ 1984; 91: 321–325. Article CAS Google Scholar * Thach AB, Dugel PU, Flindall RJ, Sipperley JO, Sneed SR . A comparison of retrobulbar
versus sub-tenon's corticosteroid therapy for cystoid macular oedema refractory to topical medications. _Ophthalmology_ 1997; 104: 2003–2008. Article CAS Google Scholar * Schimek RA,
Newsom SR . Restoration of vision in temporal arteritis by retrobulbar injections of steroids. _Am J Ophthalmol_ 1966; 62: 693–696. Article CAS Google Scholar * Tolentino MJ, McLeod DS,
Taomoto M, Otsuji T, Adamis AP, Lutty GA . Pathologic features of vascular endothelial growth factor-induced retinopathy in the nonhuman primate. _Am J Ophthalmol_ 2002; 133: 373–385.
Article CAS Google Scholar * Arnold AC, Hepler RS . Fluorescein angiography in acute nonarteritic anterior ischemic optic neuropathy. _Am J Ophthalmol_ 1994; 117: 222–230. Article CAS
Google Scholar * Inoue M, Tsukahara Y . Vascular optic neuropathy in diabetes mellitus. _Jpn J Ophthalmol_ 1997; 41: 328–331. Article CAS Google Scholar * Ho A, Maguire A, Yanuzzi L,
Fisher Y, Galetta S, Sergott R . Rapidly progressive optic disc neovascularization after diabetic papillopathy. _Am J Ophthalmol_ 1995; 120: 673–675. Article CAS Google Scholar *
Friedrich Y, Feiner M, Gawi H, Friedman Z . Diabetic papillopathy with macular star mimicking clinically significant macular oedema. _Retina_ 2001; 21: 80–82. Article CAS Google Scholar *
Lee JH, Kim SJ, Chung H . The effect of subtenon injection of methylprednisolone acetate on the breakdown of blood retinal barrier after cryotherapy. _Korean J Ophthalmol_ 1995; 9: 1–6.
Article Google Scholar * Kompella UB, Bandi N, Ayalasomayajula SP . Subconjunctival nano- and microparticles sustain retinal delivery of budesonide, a corticosteroid capable of inhibiting
VEGF expression. _Invest Ophthalmol Vis Sci_ 2003; 44: 1192–1201. Article Google Scholar * Yanagi Y, Tamaki Y, Obata R, Muranaka K, Homma N, Matsuoka B _et al_. Subconjunctival
administration of bucillamine suppresses choroidal neovascularization in rat. _Invest Ophthalmol Vis Sci_ 2002; 43: 3495–3499. PubMed Google Scholar * Weijtens O, Schoemaker RC, Lentjes
EGWM, Romijn FPHTM, Cohen AF, van Meurs JC . Dexamethasone concentration in the subretinal fluid after a subconjunctival injection, a peribulbar injection, or an oral dose. _Ophthalmology_
2000; 107: 1932–1938. Article CAS Google Scholar * Weijtens O, Feron EJ, Schoemaker RC, Cohen AF, Lentjes EG, Romijn FP _et al_. High concentration of dexamethasone in aqueous and
vitreous after subconjunctival injection. _Am J Ophthalmol_ 1999; 128: 192–197. Article CAS Google Scholar * Hyndiuk RA, Reagan MG . Radioactive depot-corticosteroid penetration into
monkey ocular tissue. _Arch Ophthalmol_ 1968; 80: 499–503. Article CAS Google Scholar * Kunou N, Ogura Y, Honda Y, Hyon SH, Ikada Y . Biodegradable scleral implant for controlled
intraocular delivery of betamethasone phosphate. _J Biomed Mater Res_ 2000; 51: 635–641. Article CAS Google Scholar * Freeman WR, Green RL, Smith RE . Echographic localization of
corticosteroids after periocular injection. _Am J Ophthalmol_ 1987; 103: 281–288. Article CAS Google Scholar * Levin DS, Han DP, Dev S, Wirostko WJ, Mieler WF, Connor TB _et al_.
Subtenon's depot corticosteroid injections in patients with a history of corticosteroid-induced intraocular pressure elevation. _Am J Ophthalmol_ 2002; 133: 196–202. Article CAS
Google Scholar * Lafranco Dafflon M, Tran VT, Guex-Crosier Y, Herbort CP . Posterior sub-Tenon's steroid injections for the treatment of posterior ocular inflammation: indications,
efficacy and side effects. _Graefes Arch Clin Exp Ophthalmol_ 1999; 237: 289–295. Article CAS Google Scholar * Gopal L, Bhende M, Sharma T . Vitrectomy for accidental intraocular steroid
injection. _Retina_ 1995; 15: 295–299. Article CAS Google Scholar * Ozerdem U, Levi L, Cheng L, Song MK, Scher C, Freeman WR . Systemic toxicity of topical and periocular corticosteroid
therapy in an 11-year-old male with posterior uveitis. _Am J Ophthalmol_ 2000; 130: 240–241. Article CAS Google Scholar * Eyetech Study Group. Preclinical and phase 1A clinical evaluation
of an anti-VEGF pegylated aptamer (EYE001) for the treatment of exudative age-related macular degeneration. _Retina_ 2002; 22: 143–152. * D'Amico DJ, Goldberg MF, Hudson H, Jerdan JA,
Krueger S _et al_. Anecortave Acetate Clinical Study Group. Anecortave acetate as monotherapy for the treatment of subfoveal lesions in patients with exudative age-related macular
degeneration (AMD): interim (month 6) analysis of clinical safety and efficacy. _Retina_ 2003; 23: 14–23. Article Google Scholar * Bojic L, Ivanisevic M, Gosovic G . Hyperbaric oxygen
therapy in two patients with non-arteritic arterior optic neuropathy who did not respond to prednisone. _Undersea Hyperb Med_ 2002; 29: 86–92. CAS PubMed Google Scholar Download
references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Ophthalmology, American University of Beirut, Beirut, Lebanon A M Mansour, M A El-Dairi & H K Shahin * Department
of Anesthesiology, Fouad Khoury Hospital, Beirut, Lebanon A M Mansour & J A Shaaban * Makassed General Hospital, Beirut, Lebanon M A Shehab * Beirut Eye Center, Rizk Hospital, Beirut,
Lebanon S R Antonios Authors * A M Mansour View author publications You can also search for this author inPubMed Google Scholar * M A El-Dairi View author publications You can also search
for this author inPubMed Google Scholar * M A Shehab View author publications You can also search for this author inPubMed Google Scholar * H K Shahin View author publications You can also
search for this author inPubMed Google Scholar * J A Shaaban View author publications You can also search for this author inPubMed Google Scholar * S R Antonios View author publications You
can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to A M Mansour. ADDITIONAL INFORMATION The authors have no proprietary interest in any product
mentioned in the manuscript. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Mansour, A., El-Dairi, M., Shehab, M. _et al._ Periocular corticosteroids in
diabetic papillopathy. _Eye_ 19, 45–51 (2005). https://doi.org/10.1038/sj.eye.6701418 Download citation * Published: 16 April 2004 * Issue Date: 01 January 2005 * DOI:
https://doi.org/10.1038/sj.eye.6701418 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * diabetic papillopathy * optic neuropathy * periocular
corticosteroids