Play all audios:
ABSTRACT The prevalence of diverse MRSA (methicillin-resistant _Staphylococcus aureus_) types in both hospital and community settings is a major health problem worldwide. Here we compare
hospital-acquired MRSAs with large type II SCC_mec_ elements with those prevalent in both hospital and community settings with smaller type IV SCC_mec_ elements. We find that the type II but
not the type IV SCC_mec_ element causes the bacteria to reduce their levels of costly toxin expression. We compare the relative growth rates of these MRSA types and show that the type II
SCC_mec_ carrying MRSAs are more affected than those carrying type IV elements and from this we hypothesize that offsetting the costs associated with antibiotic resistance and toxin
expression is why the type II are confined to hospital environments where antibiotic use, the prevalence of immunocompromised individuals and vector-mediated transmission is high. In
contrast, those MRSAs that are also successful in the community can maintain their high levels of toxin expression due to a lower fitness burden associated with the smaller SCC_mec_ element.
SIMILAR CONTENT BEING VIEWED BY OTHERS UBIQUITOUS SELECTION FOR _MECA_ IN COMMUNITY-ASSOCIATED MRSA ACROSS DIVERSE CHEMICAL ENVIRONMENTS Article Open access 27 November 2020 ALTERED GENOMIC
METHYLATION PROMOTES _STAPHYLOCOCCUS AUREUS_ PERSISTENCE IN HOSPITAL ENVIRONMENT Article Open access 07 November 2024 ENVIRONMENTAL CONDITIONS DICTATE DIFFERENTIAL EVOLUTION OF VANCOMYCIN
RESISTANCE IN _STAPHYLOCOCCUS AUREUS_ Article Open access 25 June 2021 INTRODUCTION The prevalence and success of MRSA (methicillin-resistant _Staphylococcus aureus_) in health-care and
community settings have resulted in much research into its pathogenicity in the hopes of identifying novel means of control. In the UK, 2% of hospital admissions become infected with _S.
aureus_ and of those approximately 60% will be methicillin resistant (Emmerson et al., 1996; Jones, 2003). Of increasing concern is the emergence of MRSA outside health-care settings among
healthy individuals. In 2005 a study of invasive MRSA infections in nine US centers found that 13.7% were community acquired (Klevens et al., 2007), showing the emergence of this organism as
a threat both in and outside hospitals. The types of infections caused by _S. aureus_ vary widely in both severity and site of infection. They can be relatively minor skin and soft tissue
abscesses, life-threatening cases of septicemia or endocarditis, or chronic cases of osteomyelitis (Lowy, 1998; Gordon and Lowy, 2008). The genes expressed by _S. aureus_ facilitating such
varied infections are not fully understood, but can be grouped into three based on their function: the adhesins, the toxins and the immunomodulators. The adhesins are surface-attached
proteins that allow the bacteria to attach to a wide variety of human tissues. The toxins are secreted proteins that cause tissue damage, and generate pus in abscesses, which is believed to
facilitate transmission between hosts. The immunomodulators are proteins that interfere with host immunity preventing defense against, and clearance of, infections. The expression of these
three groups of proteins is critical in determining the success of an infection. Methicillin resistance is conferred by the acquisition of a piece of DNA referred to as the SCC_mec_ element
(Deurenberg et al., 2007). The size and content of this element vary and is currently classified into five major groups (SCC_mec_ types I–V) based on their content (Deurenberg et al., 2007).
There are two features common to all SCC_mec_ elements: the _mecA_ gene, which encodes the alternative penicillin-binding protein that confers methicillin resistance, and the _ccr_
recombination sites and associated recombinases that cause this mobile piece of DNA to excise and transmit horizontally (Hiramatsu et al., 2001). SCC_mec_ elements I–III are larger than the
others and are predominantly found causing hospital- and health-care-associated infections. SCC_mec_ types IV and V are not restricted to these environments and can cause infections in
otherwise healthy individuals with no health-care contact (Ito et al, 2004; Ma et al., 2002). Although many individual virulence factors have been found to be associated with
community-acquired MRSA (for example cytolytic proteins (Wang et al., 2007), α-toxin (Li et al., 2009) and the PVL leukotoxin (Labandeira-Rey et al., 2007), it is still not clear why these
strains are successful both in and outside health-care settings. Antibiotic resistance is often associated with a fitness cost (Andersson and Levin, 1999), but compensatory mutations can
arise elsewhere in the bacterial genome that alleviates some or all of these costs (Maisnier-Patin and Andersson, 2004). Previous studies have shown that the relative fitness of
hospital-acquired MRSAs carrying the type I SCC_mec_ element is reduced (Ender et al., 2004), whereas strains containing the smaller type IV element were not affected (Lee et al., 2007). It
has also been shown in vancomycin-resistant MRSA strains containing the type II SCC_mec_ element that deletion of _mecA_ compensated for some of the fitness costs associated with becoming
vancomycin resistant, suggesting that _mecA_ is also costly (Noto et al., 2008). A detailed study of the costs associated with all five classes of SCC_mec_ elements and whether these costs
have been compensated in clinical strains has not been performed to date. Work by us and others have reported diverse virulence phenotypes among MRSA and MSSA (methicillin-sensitive
_Staphylococcus aureus_) strains (Collins et al., 2008; Fowler et al., 2004; Vaudaux et al., 1998; O’Neill et al., 2008). Here we examine the ability of both clinical and isogenic MSSAs and
MRSAs with the large type II (hospital-associated) and smaller type IV (hospital- and community-associated) SCC_mec_ elements to lyse cells. We find that the type II SCC_mec_ carrying MRSA
strains have reduced toxicity. A measure of the relative fitness of these strains shows that the type II SCC_mec_ carrying MRSA strains also have a significant fitness burden associated with
them. We hypothesize that offsetting costly toxin expression with antibiotic resistance may explain the prevalence of these different MRSA type in diverse environment and test this using a
mathematical model. MATERIALS AND METHODS T-CELL TOXICITY ASSAY T2 cells (immortalized T-cell line, Salter and Cresswell, 1986) were propagated in T-cell media (50 ml aliquots of RPMI,
supplemented with 10% heat-inactivated fetal bovine serum, 1 mM L-glutamine, 200 U ml−1 penicillin and 0.1 mg ml−1 streptomycin, at 37 °C in a humidified incubator with 5% CO2 in air) for 48
h and then harvested by centrifugation for 5 min at 700 _g_, and gently washed and resuspended in 1 ml warm tissue culture-grade phosphate-buffered saline. Washing was repeated to ensure
all antibiotics were removed. T cells were diluted in phosphate-buffered saline to a final cell concentration of 3 × 106 ml−1. Cells (15 μl) were transferred to a sterile microfuge tube for
each assay undertaken. The bacteria (strains used are described in the Supplementary Table) were grown for 17 h in 5 ml BHI broth, 750 μl of culture was removed, centrifuged for 2 min and
the supernatant was harvested. Bacterial supernatant (15 μl) and washed T cells (15 μl) were incubated for 10 min. Cell death was measured using 15 μl Trypan blue (Sigma) and a Fast-Read
counting chamber (Immune Systems, Paignton, UK). Each clinical strain indicated in the Supplementary Table was assayed once as each was considered a biological replicate indicative of its
group; for the isogenic strains 10 independently grown cultures were assayed. RELATIVE FITNESS ASSAY Bacteria (strains used are described in the Supplementary Table) were grown overnight in
BHI broth to an OD600 of 2.0 to ensure that all cells are in a similar physiological state at the start of the experiment. Competitions were established in either 0.25X BHI broth or spent
broth (BHI broth in which _S. aureus_ strains RN4390B was grown overnight, the bacteria removed by centrifugation and the medium was filter sterilized). The competition medium was inoculated
with 103 c.f.u. per ml of the marker strain (MSSA466 which is tetracycline resistant) and the test strain. Initial cell numbers were confirmed by plating. The bacteria were competed at 37
°C in a shaking incubator (180 r.p.m.) for 24 h. Final cell numbers were enumerated by serial dilutions on TSA plates (total cell count), and TSA plates containing 2 μg ml−1 tetracycline
(marker strain count). The fitness of a strain was defined as a measure of the reproductive success of the population, which can be expressed as the natural logarithm of the ratio of the
final and initial cell densities of the culture (Lenski et al., 1991). Each clinical strain was assayed once as each was considered a biological replicate indicative of its group; for the
isogenic strains 10 independently grown cultures were assayed. where: _A_(0), estimated density of test strain at time 0; _M_(0), estimated density of marker strain at time 0; _A_(1),
estimated density of test strain at time 1 day; _M_(1), estimated density of marker strain at time 1 day; ln, natural logarithm (logarithm to the base _e_). CONSTRUCTION OF BH1CC ΔSCC_MEC_
MUTANT The plasmid pSR2 (Katayama et al., 2000) was used to excise the SCC_mec_ cassette from the methicillin-resistant _S. aureus_ chromosome. The vector pSR2 contain the genes _ccrA_ and
_ccrB_ encoding polypeptides having a partial homology to recombinases of the invertase/resolvase family. The open reading frames were found to catalyze precise excision of the SCC_mec_
element. The vector which has a temperature-sensitive origin of replication (one copy at 37 °C) was introduced into BH1CC by electroporation. The strain was subcultured in drug-free broth
for 7 nights at 37 °C and the proportion of colonies that had lost the SCC_mec_ was evaluated by plating onto agar plates with and without oxacillin and by PCR analysis. STATISTICS T-cell
toxicity data contained a number of zero values and as such it was not possible to normalize. The nonparametric Mann–Whitney test was used to determine a statistical difference between
groups. The relative fitness data were determined to be normal using the Anderson–Darling normality test. Statistical differences between groups were determined using a two-tailed _t_-test.
Tests between groups were carried out on different days (that is MRSA/MSSA CC30 strains were tested separately from MRSA/MSSA CC22 and CC8 strains); it is therefore not reliable to test
between these groups as small differences in the initial marker strain could cause a statistical effect. Where tests have been carried out, relative fitness tests were carried out at the
same time, using the same media, and the same marker strain. MATHEMATICAL MODELING The model describes the dynamics of three _S. aureus_ strains competing within the population: MSSA
(methicillin susceptible), IV-MRSA (type IV SCC_mec_ carrying MRSA) and II-MRSA (type II SCC_mec_ carrying MRSA). It is assumed that susceptible hosts, _S_, can only be infected by one
strain at the time on which they move into the infected classes, _I_MSSA, _I_IV-MRSA or _I_II-MRSA; after successful treatment infected individuals return to the susceptible class, that is
infection does not offer immunity to renewed infection. Infection itself has two components/routes: one is by direct host–host contact and to a degree dependent on the production of toxins,
the other is due to secondary contact, for example through health-care workers within a community or hospital environment. The model can then be given as the following set of differential
equations describing the rate of change in the proportion of the population currently susceptible or infected: where _μ_ (=0.013) is the average host birth and death rate (we assume constant
population size); _τ__i_ and _δi_, the rate of treatment- and infection-associated mortality of strain _i_ respectively. The force of infection of strain _i_ is given as: where _β_i_i_ and
_β_h are the transmission parameters through direct and secondary (that is vector-mediated) contact respectively, and _c_i_i_ and _c_r_i_ the respective fitness costs associated with toxin
production and antibiotic resistance. Note, secondary transmission is strain independent and will be used to describe the two different transmission environments: community and hospital. The
main assumption/parameter values are given in the following table 1: This means, we assume that the propensity of MSSA to cause transmissible illness/disease is greater than for II-MRSA as
these have reduced toxin production, which is also reflected in a reduced fitness cost, that is _β__t_MSSA>_β__t__I_I-MRSA and _c__t_MSSA>_c_tII-MRSA. IV-MRSA on the other hand is even
more transmissible than MSSA but at no extra fitness cost, that is _β__t_IV-MRSA>_β__t_MSSA and _c__t_MSSA=_c__t__I_V-MRSA. We furthermore assume that infections by methicillin-resistant
strains have a reduced treatment success rate and therefore a (slightly) higher chance of being lethal, although the latter assumption is not a necessary for the results presented here. We
distinguish between two different environments: (1) a community setting where the majority of transmission is through direct, rather than vector-mediated, contact; and (2) a hospital setting
with a greatly enhanced chance of vector-mediated transmission but also a higher rate of treatment. The basic reproductive ratios of the three strains are given as We can then find the
condition under which either type II or type IV-MRSA dominate the population simply as _R_0II-MRSA>_R_0IV-MRSA>_R_0MSSA or _R_0IV-MRSA>_R_0II-MRSA>_R_0MSSA respectively. Under
the assumption that the cost of resistance, rate of treatment and induced mortality are equal for type II and type IV MRSAs, we can also find an explicit condition for type II outcompeting
type IV MRSA as and _vice versa_. This can simply be interpreted as follows: if the cost of toxin production cannot be offset by a gain in transmissibility (in different environments), then
a particular strain will be outcompeted and replaced by another strain with either a lower fitness cost or higher transmissibility. RESULTS CARRIAGE OF THE TYPE II BUT NOT THE TYPE IV
SCC_MEC_ ELEMENT AFFECTS MRSA TOXICITY Hospital-acquired MRSA strains, such as those containing the type II SCC_mec_ element, rarely cause disease outside health-care setting among healthy
people (Hiramatsu et al., 2001). This has been partially attributed to diminished growth rates associated with antibiotic resistance, but our findings suggest that lower levels of toxicity
may also contribute to reduced virulence in healthy individuals (Collins et al., 2008). MRSA strains containing the smaller type IV SCC_mec_ element are successful both in and outside
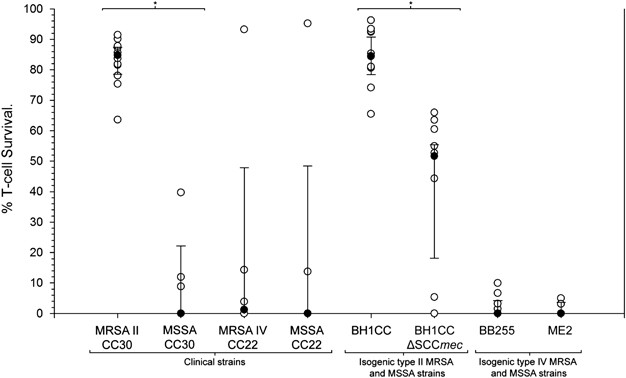
health-care settings, suggesting that these MRSA strains may be more toxic than strains carrying the type II element. To test this, we compared the toxicity of both clinical and isogenic
type II and type IV SCC_mec_ carrying MRSA strains. Figure 1 shows that the type II SCC_mec_ element reduces the toxicity of strains and shows that carriage of the type IV element has no
such effect. TOXIN EXPRESSION AND THE TYPE II SCC_MEC_ ELEMENT AFFECT THE RELATIVE FITNESS OF _S. AUREUS_ We hypothesize that the smaller type IV SCC_mec_ element may have less of a fitness
burden associated with it. To test this, we performed competitions in low-nutrient broth (0.25X BHI) against a marked MSSA strain (this medium was selected to provide the optimum nutrient
level to get direct competition for nutrients between the marked and tester strains as well as sufficient growth of the bacteria for fitness differences to be detectable). The relative
fitness of clonally matched clinical MSSA and MRSA strains (containing both type II and IV SCC_mec_ elements) and isogenic type II and IV MRSA/MSSA pairs was measured (Figure 2). For both
the clinical and isogenic strains the type II SCC_mec_ element reduced relative fitness of the strain carrying it (_P_<0.001, _T_=6.08, d.f.=57 and _P_=0.0044, _T_=−3.28, d.f.=17
respectively). The type IV SCC_mec_ carrying clinical strains were slightly less fit than MSSA strains from the same clonal complexes (CC8 and 22) that just reached statistical significance
(_P_=0.049, _T_=2.32, d.f.=8) but there was no difference in fitness between the isogenic pair of strains (_P_=0.64, _T_=−0.47, d.f.=26) showing that this element does not incur a fitness
cost in this experimental system. In all cases, a two-sample _t_-test was used to determine a statistical difference as the data were shown to be normal. The Agr system in _S. aureus_ is the
major global regulator of toxin expression. To determine if toxin expression was also costly, we also measured the relative fitness of an isogenic pair of Agr+ and Agr− MSSA strains
(RN6390B and RN6911 respectively; Ji et al., 1997) where the negative strain does not express toxins. These strains were competed against a marked MSSA strain, but the medium used was
freshly spent broth in which the wild-type Agr+ strain was grown for 24 h to ensure maximal toxin expression from the residual Agr-encoded autoinducing peptide during the competition. The
Agr mutant was significantly more fit than the toxin expressing wild-type strain (median relative fitness Agr+, 1.36; Agr−, 1.48; _P_=0.003, _T_=−5.74, d.f.=9, two-sample _t_-test), which
shows that toxin expression is costly in environments in which there is no selection for it. Although other Agr-regulated factors may contribute to the fitness effects observed here, our
previous work found it to be the most significant contributing factor to strain toxicity, and as such we consider it to be the major factor involved here. CAN THE RELATIVE COSTS OF TOXIN
EXPRESSION AND ANTIBIOTIC RESISTANCE EXPLAIN THE PREVALENCE OF DIFFERENT MRSAS IN DIFFERENT ENVIRONMENTS? Transmission of _S. aureus_ between humans can be either symptomatic or asymptomatic
(Massey et al., 2006). Asymptomatic transmission occurs by direct contact between a carrier and noncarrier. Symptomatic transmission can also occur by direct contact but also by
vector-mediated transmission through health-care workers. Symptomatic direct-contact transmission, such as in cases of impetigo, results from the production of sticky pus-filled vesicles
containing high densities of bacteria that get transmitted on fingers or during close-contact games such as rugby or American football (Lu and Holtom, 2005). Vector-mediated transmission
occurs in health-care settings between patients with underlying conditions that make them more susceptible to infection and where poor hand hygiene among health-care workers is prevalent.
These diverse means of transmission have the potential to select for different bacterial characteristics resulting in diverse virulence phenotypes among _S. aureus_ strains. Mathematical
modeling has been successfully used to help us understand transmission dynamics of many infectious diseases (Anderson and May, 1991). Here we use it to see if the relative costs associated
with antibiotic resistance and toxin expression can explain why certain MRSA strains are restricted to health-care environments and others are not. We hypothesize that in the hospital
environment the type II SCC_mec_-containing MRSA strains are successful because they are resistant to antibiotics and have offset some of the fitness costs associated with this by reducing
costly toxin expression. They can survive with reduced toxin expression because transmission through health-care workers means they are not dependent on toxin-related production of
transmissible material. They also have a population of compromised patients available with greater susceptibility to infection and so do not need to be as virulent to cause disease. This
would explain why these MRSA strains have not been successful in the community setting where transmission through health-care worker and the prevalence of susceptible hosts are lower. We
also hypothesize that the type IV SCC_mec_-containing MRSA strains are successful in both health-care and community settings because they have found an alternative means of reducing the
fitness burden associated with being antibiotic resistant, which has allowed them to retain full toxicity. To test our hypotheses and investigate whether these factors can explain the
prevalence of these MRSA strains in different environments, we developed a mathematical model in which we competed three strain types (see Material and methods for full details). One had
high-cost resistance and low-level (and therefore low-cost) toxin production, representative of type II SCC_mec_-containing MRSA strains. The second had low-cost resistance and high-level
and high-cost toxin production representative of type IV SCC_mec_-containing MRSA strains. The third had no antibiotic resistance and high-level and high-cost toxin expression representative
of MSSA strains. Two environments were established, the first representative of the community setting where the majority of transmission is through direct rather than vector-mediated
contact; the second representative of a hospital setting with a greatly enhanced chance of vector-mediated transmission but also a higher rate of treatment. Figure 3 shows the time series
for the proportion of the population infected with different _S. aureus_ strains for the two different transmission settings: community (Figure 3a) and hospital (Figure 3b). The simulations
started off with only MSSA being present in the population, and after it had reached a stable prevalence both MRSA types were introduced (at time _t_=0). Within the community (Figure 3a),
the type IV MRSA quickly becomes the dominant strain because of increased toxicity and antibiotic resistance and despite a lower treatment success and increased lethality. In contrast,
within a hospital setting (Figure 3b) the type II MRSA outcompetes the type IV MRSA because the now dominant secondary route of transmission (that is health-care workers) disadvantages
enhanced toxicity and its associated fitness cost. However, the interaction between the two MRSAs here is dependent on the relative costs associated with the larger type II SCC_mec_ element
and the cost of toxin production, neither of which is empirically measurable. The true picture of _S. aureus_ infection in hospitals is continually evolving and is currently slightly
different from this model where MSSAs remain in a significant presence. We believe that this reflects the infection of carriers with their own MSSA strain, and the continual reintroduction
of MSSAs on carriers as they enter hospitals. Our experimental system was closed such that after the introduction of the MRSAs, no further bacteria were introduced into the system.
DISCUSSION Our findings and mathematical model reveal that the costs associated with toxin production and antibiotic resistance can explain why hospital- and community-acquired MRSA strains
are successful in different environments where transmission routes and host susceptibility vary. We show that the large hospital-associated type II SCC_mec_ element has a significant effect
on the toxicity and growth rate of MRSAs. The mechanism by which the type II element reduces toxin expression is not fully understood but is possibly a consequence of the presence of the
recently identified _fudoh_ gene (Kaito et al., 2008). We believe the fitness burden associated with carrying the large type II SCC_mec_ element is partially compensated for by the reduction
in toxin expression, and that this contributes to the restriction of these MRSA strains to health-care settings where transmission is often through health-care workers and a large pool of
susceptible hosts are available. The smaller type IV SCC_mec_ element does not affect the relative fitness of the bacteria as much as the type II element, and does not affect toxicity
resulting in a fully virulent, antibiotic-resistant bacterium. We believe that this may explain why these MRSA strains are successful both in health-care settings and among healthy
individuals in the community. These findings suggest that in hospital environments transmission through health-care workers has significantly contributed to the evolution of this pathogen,
allowing them to adapt to the fitness burdens associated with antibiotic resistance. Vector-mediated transmission is more traditionally associated with selecting for increased virulence, as
the health of the host is not believed to contribute to their susceptibility to vectors (such as the transmission of malaria through mosquito). Here, however, the contrary seems to be true,
where vector transmission appears to be selecting for decreased virulence. However in this instance the interaction of the host with its vector (health-care workers) is a secondary feature
to infection. The patients are typically receiving the attention of health-care workers for treatment of underlying medical conditions or after surgery/trauma, so their immune system has
already been compromised. The more this is compromised, the more attention they are likely to get from health-care workers and the more susceptible they are to infection. As such the
dynamics are quite different to the traditional vector-transmitted diseases. In our model of the hospital environment, the weighting given to the cost associated with unnecessary toxin
production leads to the type II MRSAs eventually dominating. If however toxin production became an important part of the transmission of _S. aureus_ in this environment, this dynamic would
change. For example, if transmission through health-care workers was eliminated, the type IV MRSAs are likely to become dominant as their low-cost antibiotic resistance alongside high toxin
production would give them a significant advantage. The model of the community environment suggests that the type IV MRSAs become dominant and displace the MSSAs, however many other factors
contribute to the success of this pathogen in the real world so it is difficult to say with any certainty what the future holds. What is interesting to consider is how asymptomatic
transmission of _S. aureus_ occurs among healthy people and how modern sanitized lifestyles puts up barriers to this. We previously hypothesized that it is barriers to asymptomatic
transmission that have allowed _S. aureus_ to become more virulent relative to _S. epidermidis_ (Massey et al., 2006), and based on the work described here we suggest that it is possible
that increased use of antibiotics and barriers to asymptomatic transmission of _S. aureus_ between healthy people will continue to select for more virulent, antibiotic-resistant _S. aureus_
strains. REFERENCES * Anderson RM, May RM . (1991). _Infectious Disease of Humans: Dynamics and Control_. Oxford University Press: New York. Google Scholar * Andersson DI, Levin BR .
(1999). The biological cost of antibiotic resistance. _Curr Opin Microbiol_ 2: 489–493. Article CAS Google Scholar * Collins J, Buckling A, Massey RC . (2008). Identification of factors
contributing to T-cell toxicity of _Staphylococcus aureus_ clinical isolates. _J Clin Microbiol_ 46: 2112–2114. Article Google Scholar * Deurenberg RH, Vink C, Kalenic S, Friedrich AW,
Bruggeman CA, Stobberingh EE _et al_. (2007). The molecular evolution of methicillin-resistant _Staphylococcus aureus_. _Clin Microbiol Infect_ 13: 222–235. Article CAS Google Scholar *
Emmerson AM, Enstone JE, Griffin M, Kelsey MC, Smyth ET . (1996). The Second National Prevalence Survey of infection in hospitals—overview of the results. _J Hosp Infect_ 32: 175–190.
Article CAS Google Scholar * Ender M, McCallum N, Adhikari R, Berger-Bachi B . (2004). Fitness cost of SCCmec and methicillin resistance levels in _Staphylococcus aureus_. _Antimicrob
Agents Chemother_ 48: 2295–2297. Article CAS Google Scholar * Fowler Jr VG, Sakoulas G, McIntyre LM, Meka VG, Arbeit RD, Cabell CH _et al_. (2004). Persistent bacteremia due to
methicillin-resistant _Staphylococcus aureus_ infection is associated with agr dysfunction and low-level _in vitro_ resistance to thrombin-induced platelet microbicidal protein. _J Infect
Dis_ 190: 1140–1149. Article CAS Google Scholar * Gordon RJ, Lowy FD . (2008). Pathogenesis of methicillin-resistant _Staphylococcus aureus_ infection. _Clin Infect Dis_ 5: S350–S359.
Article Google Scholar * Hiramatsu K, Cui L, Kuroda M, Ito T . (2001). The emergence and evolution of methicillin-resistant _Staphylococcus aureus_. _Trends Microbiol_ 9: 486–493. Article
CAS Google Scholar * Ito T, Ma XX, Takeuchi F, Okuma K, Yuzawa H, Hiramatsu K . (2004). Novel type V staphylococcal cassette chromosome mec driven by a novel cassette chromosome
recombinase, ccrC. _Antimicrob Agents Chemother_ 48: 2637–2651. Article CAS Google Scholar * Ji G, Beavis R, Novick RP . (1997). Bacterial interference caused by autoinducing peptide
variants. _Science_ 276: 2027–2030. Article CAS Google Scholar * Jones RN . (2003). Global epidemiology of antimicrobial resistance among community-acquired and nosocomial pathogens: a
five-year summary from the SENTRY Antimicrobial Surveillance Program (1997–2001). _Semin Respir Crit Care Med_ 24: 121–134. Article Google Scholar * Kaito C, Omae Y, Matsumoto Y, Nagata M,
Yamaguchi H, Aoto T _et al_. (2008). A novel gene, _fudoh_, in the SCCmec region suppresses the colony spreading ability and virulence of _Staphylococcus aureus_. _PLoS One_ 3: 3921.
Article Google Scholar * Katayama Y, Ito T, Hiramatsu K . (2000). A new class of genetic element, staphylococcus cassette chromosome mec, encodes methicillin resistance in _Staphylococcus
aureus_. _Antimicrob Agents Chemother_ 44: 1549–1555. Article CAS Google Scholar * Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, et al., Active Bacterial Core surveillance
(ABCs) MRSA Investigators. (2007). Invasive methicillin-resistant _Staphylococcus aureus_ infections in the United States. _JAMA_ 298: 1763–1771. Article CAS Google Scholar *
Labandeira-Rey M, Couzon F, Boisset S, Brown EL, Bes M, Benito Y _et al_. (2007). _Staphylococcus aureus_ Panton–Valentine leukocidin causes necrotizing pneumonia. _Science_ 315: 1130–1133.
Article CAS Google Scholar * Lee SM, Ender M, Adhikari R, Smith JM, Berger-Bächi B, Cook GM . (2007). Fitness cost of staphylococcal cassette chromosome mec in methicillin-resistant
_Staphylococcus aureus_ by way of continuous culture. _Antimicrob Agents Chemother_ 51: 1497–1499. Article CAS Google Scholar * Lenski R, Rose M, Simpson S, Tadler S . (1991). Long-term
experimental evolution in _Escherichia coli_. I. Adaptation and divergence during 2,000 generations. _Am Nat_ 138: 1315. Article Google Scholar * Li M, Diep BA, Villaruz AE, Braughton KR,
Jiang X, DeLeo FR _et al_. (2009). Evolution of virulence in epidemic community-associated methicillin-resistant _Staphylococcus aureus_. _Proc Natl Acad Sci USA_ 106: 5883–5888. Article
CAS Google Scholar * Lowy FD . (1998). _Staphylococcus aureus_ infections. _N Engl J Med_ 339: 520–532. Article CAS Google Scholar * Lu D, Holtom P . (2005). Community-acquired
methicillin-resistant _Staphylococcus aureus_, a new player in sports medicine. _Curr Sports Med Rep_ 4: 265–270. Article Google Scholar * Ma XX, Ito T, Tiensasitorn C, Jamklang M,
Chongtrakool P, Boyle-Vavra S _et al_. (2002). Novel type of staphylococcal cassette chromosome mec identified in community-acquired methicillin-resistant _Staphylococcus aureus_ strains.
_Antimicrob Agents Chemother_ 46: 1147–1152. Article CAS Google Scholar * Maisnier-Patin S, Andersson DI . (2004). Adaptation to the deleterious effects of antimicrobial drug resistance
mutations by compensatory evolution. _Res Microbiol_ 155: 360–369. Article CAS Google Scholar * Massey RC, Horsburgh MJ, Lina G, Hook M, Recker M . (2006). The evolution and maintenance
of virulence in _Staphylococcus aureus_: a role for host-to-host transmission? _Nat Rev Microbiol_ 4: 953–958. Article CAS Google Scholar * O’Neill E, Pozzi C, Houston P, Humphreys H,
Robinson DA, Loughman A _et al_. (2008). A novel _Staphylococcus aureus_ biofilm phenotype mediated by the fibronectin-binding proteins, FnBPA and FnBPB. _J Bacteriol_ 190: 3835–3850.
Article Google Scholar * Noto MJ, Fox PM, Archer GL . (2008). Spontaneous deletion of the methicillin resistance determinant, mecA, partially compensates for the fitness cost associated
with high-level vancomycin resistance in _Staphylococcus aureus_. _Antimicrob Agents Chemother_ 52: 1221–1229. Article CAS Google Scholar * Salter RD, Cresswell P . (1986). Impaired
assembly and transport of HLA-A and -B antigens in a mutant TxB cell hybrid. _EMBO J_ 5: 943–949. Article CAS Google Scholar * Vaudaux PE, Monzillo V, Francois P, Lew DP, Foster TJ,
Berger-Bächi B. (1998). Introduction of the mec element (methicillin resistance) into _Staphylococcus aureus_ alters _in vitro_ functional activities of fibrinogen and fibronectin adhesins.
_Antimicrob Agents Chemother_ 42: 564–570. Article CAS Google Scholar * Wang R, Braughton KR, Kretschmer D, Bach TH, Queck SY, Li M _et al_. (2007). Identification of novel cytolytic
peptides as key virulence determinants for community-associated MRSA. _Nat Med_ 13: 1510–1514 http://saureus.mlst.net/. Article CAS Google Scholar Download references ACKNOWLEDGEMENTS
This work was funded by studentships to JC (Stiefel) and JR (BBSRC). We thank Brigitte Berger-Bachi for providing strains and Angus Buckling and Sarah Turner for constructive discussion of
the paper. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Zoology, University of Oxford, Oxford, UK James Collins & Mario Recker * Department of Biology and Biochemistry,
University of Bath, Somerset, UK Justine Rudkin & Ruth C Massey * School of Biomolecular and Biomedical Sciences, University College Dublin, Dublin, Ireland Clarissa Pozzi & James P
O'Gara Authors * James Collins View author publications You can also search for this author inPubMed Google Scholar * Justine Rudkin View author publications You can also search for
this author inPubMed Google Scholar * Mario Recker View author publications You can also search for this author inPubMed Google Scholar * Clarissa Pozzi View author publications You can also
search for this author inPubMed Google Scholar * James P O'Gara View author publications You can also search for this author inPubMed Google Scholar * Ruth C Massey View author
publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Ruth C Massey. ADDITIONAL INFORMATION Supplementary Information accompanies
the paper on The ISME Journal website (http://www.nature.com/ismej) SUPPLEMENTARY INFORMATION SUPPLEMENTARY TABLE (DOC 125 KB) SUPPLEMENTARY TABLE LEGEND (DOC 24 KB) RIGHTS AND PERMISSIONS
Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Collins, J., Rudkin, J., Recker, M. _et al._ Offsetting virulence and antibiotic resistance costs by MRSA. _ISME J_ 4, 577–584
(2010). https://doi.org/10.1038/ismej.2009.151 Download citation * Received: 20 October 2009 * Revised: 30 November 2009 * Accepted: 03 December 2009 * Published: 14 January 2010 * Issue
Date: April 2010 * DOI: https://doi.org/10.1038/ismej.2009.151 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * _Staphylococcus aureus_ * MRSA *
fitness costs * virulence costs