Play all audios:
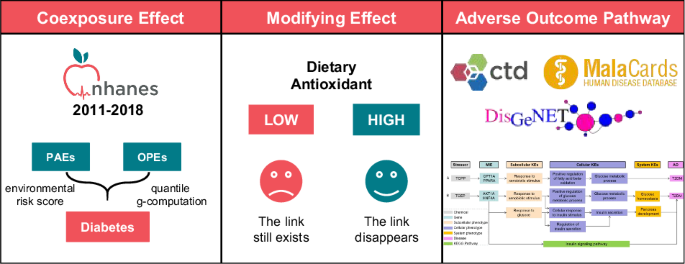
ABSTRACT BACKGROUND The association of plastic additive mixture exposure with diabetes and the modifying effects of dietary antioxidants are unclear. METHODS The data from the NHANES
2011–2018 were retrieved, and phthalates and organophosphate esters (OPEs) were selected as exposures. The coexposure effect was analyzed by the environmental risk score (ERS) and quantile
g-computation. To mitigate any potential bias caused by using the internal weights, another version of ERS was constructed using the cross-validation approach. The level of dietary
antioxidant intake was measured by the composite dietary antioxidant index (CDAI). The biological mechanism underlying the association was studied by the adverse outcome pathway (AOP)
framework. RESULTS Fifteen chemicals (ten phthalates and five OPEs) were measured in 2824 adult participants. A higher ERS was significantly associated with an increased risk of diabetes (OR
per 1-SD increment of ERS: 1.25, 95% CI: 1.13–1.39). This association apparently interacted with the CDAI level (ORlow: 1.83, 95% CI: 1.37–2.55; ORhigh: 1.28, 95% CI: 1.15–1.45;
_P_interaction = 0.038). Moreover, quantile g-computation also revealed higher level of combined exposure was positively associated with diabetes (OR: 1.27, 95% CI: 1.05–2.87), and the
addition of dietary antioxidants showed a null association (OR: 1.09, 95% CI: 0.85–2.34). The AOP study identified TCPP and TCEP as key chemicals that cause aberrant glucose metabolism and
insulin signaling pathways and result in diabetes. CONCLUSIONS Coexposure to phthalates and OPEs is positively associated with diabetes, where an antioxidative diet plays a modifying role.
Several potential mechanisms have been proposed by AOP framework. SIMILAR CONTENT BEING VIEWED BY OTHERS NON-PERSISTENT EXPOSURES FROM PLASTICIZERS OR PLASTIC CONSTITUENTS IN REMOTE ARCTIC
COMMUNITIES: A CASE FOR FURTHER RESEARCH Article Open access 28 March 2022 ASSOCIATION BETWEEN PER- AND POLYFLUOROALKYL SUBSTANCES EXPOSURE AND RISK OF DIABETES: A SYSTEMATIC REVIEW AND
META-ANALYSIS Article 15 August 2022 ASSOCIATION OF MIXED POLYCYCLIC AROMATIC HYDROCARBONS EXPOSURE WITH OXIDATIVE STRESS IN KOREAN ADULTS Article Open access 29 March 2024 INTRODUCTION
Plastic materials are indispensable durable materials in modern daily life. They are widely used in various fields, such as automobile, agricultural, healthcare, construction, toy,
packaging, and textile production [1]. Annual global use reached 460 million metric tons in 2019, and this value is expected to nearly triple by 2060. Low-cost and durable plastic products
are convenient for use in our lives. However, a significant amount of plastic waste is generated each year, accounting for 54% of the global anthropogenic waste quality [2]. The large
production volume, low recycling rate, and insufficient sustainable policies supporting plastic recycling have led to a large influx of plastic waste into the environment. Plastic waste is
toxic when it contacts different species, including humans. Toxicity can be caused by the polymer matrix, additives, degradation products, and adsorbed pollutants [3]. According to previous
reports, polyvinyl chloride is the most toxic type of polymer (monomer or additive) commonly used in daily life; additionally, additives are more toxic to wildlife and humans than monomers
[1]. Presently, the most common chemical additives used, such as flame retardants, and plasticizers, such as phosphate-based flame retardants and phthalate esters (PAEs), pose significant
threats to human health [3]. PAEs are currently the most widely used plasticizers and one of the most toxic additives in polyvinyl chloride products [1]. The global annual production of PAEs
can reach 11 billion pounds. Organic phosphate esters (OPEs) are widely used as substitutes for brominated flame retardants in production and daily life. The global consumption of OPEs was
500,000 tons in 2011, and this number increased to 680,000 tons in 2015 [4]. In addition to being a flame retardant, OPE is also used as a plasticizer and solvent and in other industrial
applications [5]. PAEs and OPEs are used as plasticizers, flame retardants, solvents, and in other industrial applications [5, 6]. These additives are not chemically bound to the products
and are vulnerable to volatilization and leaching into the environment. The combined exposure levels of PAEs and OPEs are greater in environmental media and in living organisms, including
humans [7,8,9,10]. Ingestion, inhalation, and skin contact are the main pathways of coexposure to PAEs and OPEs. Studies have shown that coexposure to PAEs and OPFRs is associated with
adverse early reproductive outcomes resulting from in vitro fertilization [11], childhood asthma resulting from disruption of inflammatory lipids and fatty acid metabolism [10], and
neurodevelopmental deficits [12]. Although a positive correlation between PAE or OPEs alone and the risk of diabetes in adults has been found [13,14,15], the effect of their combined
exposure on diabetes has not been studied. However, the biological mechanism underlying the impact of PAEs or OPEs exposure on the risk of diabetes is still unclear. The adverse outcome
pathway (AOP) is a framework commonly used in the field of computational toxicology to explore the toxic action patterns of chemicals. By integrating public database resources, such as the
comparative toxicogenomics database (CTD), disease gene network (DisGeNET), and MalaCards human disease database, researchers have effectively developed some AOPs for potential mechanistic
pathways between chemical exposure and disease [16,17,18,19]. Interestingly, evidence has suggested that PAE exposure is associated with increased oxidative stress, which mediates the
development of insulin resistance and diabetes [20, 21]. The positive association between PAE exposure and insulin resistance weakened among participants with higher concentrations of serum
β-carotene, which is an abundant antioxidant [22]. In addition to β-carotenoids, a large amount of other vitamins and trace elements in food are antioxidants. Studying the protective effects
of antioxidant nutrient intake on the health hazards of PAE and OPE exposure is highly important. Utilizing NHANES data from 2011 to 2018, this study aimed to: (1) analyze the association
between exposure to key substances of PAEs and OPEs combined and diabetes; (2) investigate whether antioxidant diets can modify this association; and (3) identify the potential biological
mechanism behind the increased diabetes risk associated with PAEs and OPEs. METHODS STUDY DESIGN AND POPULATION The NHANES is an ongoing national cross-sectional survey specifically designed
to evaluate the health and nutritional status of representative individuals of the U.S. civilian noninstitutionalized resident population. Recognizing that the measurement of PAE and OPE in
subsamples might not yield sufficient stability for robust analyses within a single survey cycle, we extracted and combined data from four survey cycles spanning the years 2011–2018, which
included 5434 participants with information on the concentrations of PAEs and OPEs, self-reported diabetes and other covariates. After excluding individuals who were younger than 18 years
(_n_ = 2046), pregnant (_n_ = 29), or missing data for the outcome (_n_ = 3) or for exposure and other covariates (_n_ = 514), a total of 2824 individuals were included in the analysis (Fig.
S1). Diabetes status was determined through the question “Did you have diabetes or sugar diabetes?” The respondents who refused to answer or did not know the answer were treated as missing.
Since some participants had borderline hyperglycemia, we created two scenarios of diabetes: the first scenario included patients with diabetes and borderline high blood sugar levels, while
the second scenario did not include the borderline levels. We conducted the primary analyses with the outcome defined as diabetes in the first scenario and then repeated the procedure by
changing the outcome to diabetes in the second scenario. MEASUREMENT OF PAES AND OPES IN URINE The concentrations of PAEs and OPEs in urine were measured in participants aged 6 years and
older from a one-third subsample by NHANES researchers using analytical methods that have been previously described elsewhere [23, 24]. Briefly, the method uses 0.2 mL of urine and is based
on enzymatic hydrolysis of urinary conjugates of the target analytes, automated off-line solid-phase extraction, reversed-phase high-performance liquid chromatography separation, and isotope
dilution-electrospray ionization-tandem mass spectrometry detection. For this study, we focused on ten PAEs and five OPEs with missing data rates lower than 30% [25] (details in Table S1),
including MEP (mono-ethyl phthalate), MnBP (mono-_n_-butyl phthalate), MiBP (mono-isobutyl phthalate), MBzP (monobenzyl phthalate), MEHHP (mono-(2-ethyl-5-hydroxyhexyl) phthalate), MEOHP
(mono-(2-ethyl-5-oxohexyl) phthalate), MECPP (mono-2-ethyl-5-carboxypentyl phthalate), MCPP (mono-(3-carboxypropyl) phthalate), MCNP (mono (carboxynonyl) phthalate), MCOP (mono
(carboxyoctyl) phthalate), BCPP (bis(1-chloro-2-propyl) phosphate), BCEP (bis(2-chloroethyl) phosphate), BDCP (bis-p-cresyl phosphate), DBUP (dibutyl phosphate), and DPHP (diphenyl phosphate
(DPHP). In cases where the result was below the limit of detection, the value for that variable was the detection limit divided by the square root of 2. To mitigate the impact of diluted
urine, PAEs and OPEs concentrations were adjusted for urinary creatinine and were expressed as μg/g creatinine. COVARIATES The selection of covariates for this analysis was based on previous
knowledge about the association between environmental exposure and diabetes. The included covariates were time of sampling, sex, age, race, marital status, education, body mass index (BMI),
household poverty-to-income ratio, smoking status, alcohol consumption status, hypertension status, gout status, family history of diabetes, daily intake of nutrients (total energy, fat,
protein, and carbohydrate), alanine transaminase (ALT), aspartate aminotransferase (AST), blood urea nitrogen (BUN), and creatinine. We used the composite dietary antioxidant index (CDAI) to
describe the level of antioxidants in the diet. The CDAI was calculated by adding the six normalized vitamins and minerals, including vitamins A, C, and E, selenium, zinc, and carotenoids
from food only [26]. The diet-derived intake information was obtained from a detailed dietary interview component that estimated the types and amounts of foods and beverages consumed during
the 24-h period prior to the interview. The CDAI score was subsequently transformed into a binary variable (low/high) according to the 75th percentile value. STATISTICAL ANALYSIS All
analyses were performed using R software (Vienna, Austria, version 4.3.0), and a _P_ value less than 0.05 was considered as significant. The demographic characteristics accounting for the
sampling design effect were shown as the median (p25, p75) and percentage (standard error) for continuous and categorical variables, respectively. To test the equality of two medians or two
proportions, the design-based rank test or Rao‐Scott chi‐square test was used. The exposure levels of each chemical were shown by weighted percentiles (5th, 25th, 50th, 75th, and 95th). The
Spearman correlation coefficients of each pair of chemicals were calculated and illustrated by a heatmap. These procedures were implemented using the “survey” package [27]. To investigate
the association between single exposure (logarithm-transformed) and diabetes, survey-weighted logistic regression was used, and odds ratios (ORs) with 95% confidence intervals (CIs) were
calculated. The strategy of covariate adjustment was as follows: Model 1 included sampling time, age, sex, poverty status, race, education, marital status, smoking status, drinking status,
BMI, hypertension status, gout status, and family history of diabetes; Model 2 additionally included total nutrient intake, liver function, and kidney function. These procedures were
implemented using the “survey” package [27]. We computed the environmental risk score (ERS) to assess the cumulative risk of diabetes from exposure to PAEs and OPEs [28]. The score is a
weighted sum of exposed chemicals, whose weights (β) are derived from the adaptive elastic net (adENET) method. This method utilizes two tuning parameters (lambda 1 and lambda 2) to select
the subsets of chemicals within the mixture that are most predictive of individual diabetes and to quantify the relationship between pollutants and diabetes. Specifically, lambda 1 shrinks
the coefficients of unimportant predictors exactly to zero, and lambda 2 stabilizes selection in the presence of highly correlated predictors. Five-fold cross-validation and optimization of
cross-validated prediction errors were used to estimate lambda 1 and lambda 2 (Fig. S2a). To avoid overfitting issues and mitigate any potential bias caused by using the internal weights, we
constructed another ERS (ERS_CV) by a cross-validation approach as a supplementary analysis. Briefly, the data were randomly divided into 5 folds, with weights for each fold predicted from
the adENET model trained on the other fourfolds [29]. To evaluate the effect of mixed exposure, scaled ERS and the tertile category of ERS were used in the logistic regression adjusting for
Model 2 covariates. The linear trend across tertiles of ERS was additionally tested by assigning 1–3 for the tertile and modeling this value as a continuous variable. These procedures were
implemented using the R packages “gcdnet” [30] and “caret” [31]. To ensure the robustness of the findings, a quantile g computation (qg-computation) model was also used to evaluate the
combined effect of PAEs and OPEs on diabetes, conditional on no covariate (crude model) or Model 2 covariate (adjusted model). The overall mixture effect from the qg-computation model (psi1)
is interpreted as the effect on the outcome of increasing every exposure by one quantile. These analyses were implemented using the “qgcomp” package [32]. The modifying effect of the CDAI
on the association between mixed exposure and diabetes was examined by adding an interaction term (ERSscaled × CDAIlow/high) to the weighted logistic regression model and testing whether the
_P_ value for the interaction was significant. In addition, the modifying effect was investigated by adding CDAI components to the aforementioned qg-computation model. We hypothesized that
a modifying effect would occur if the mixture effect of the new model reversed to null, which implied that adding antioxidant nutrients would decrease the positive mixture effect of PAEs and
OPEs. AOP DEVELOPMENT BASED ON PUBLIC DATABASES The research results suggest that the metabolites TCEP and TCPP have the highest weights under additive mixture exposure. Type 2 diabetes
mellitus (T2DM) is the main type of diabetes in adults and is considered an “adverse outcome (AO)”. On January 14, 2024, the “Gene” and “Phenotype” tags of TCEP and TCPP were searched in the
CTD database. The TCEP- and TCPP-related genes and phenotypes were obtained and are referred to as “TCEP-gene”, “TCPP-gene”, “TCEP-phenotype”, and “TCPP-phenotype”, respectively. In
addition, under the “disease” tag in the CTD database, candidate genes for T2DM associated with TCEP and TCPP were identified and named “TCEP-gene-T2DM” and “TCPP-gene-T2DM”, respectively.
Similarly, information related to the T2DM gene and T2DM phenotype was obtained from the DisGeNET and MalaCards public databases. A summary of the collected genes and phenotypes is shown in
Table S2. A Venn diagram was generated to identify the genes intersecting the TCEP-gene or TCPP-gene with the T2DM gene (Fig. 1A). The genes were subsequently subjected to Gene Ontology (GO)
and Kyoto Encyclopedia of Genes and Genomes (KEGG) enrichment analyses using the package “clusterProfiler” [33]. These analyses focused on _Homo sapiens_ as the source organism.
Furthermore, these statistically significant GO and KEGG analysis results (_P_ < 0.05) were intersected with the T2DM phenotype to obtain the target phenotype set (Fig. 1B). To obtain
more reliable genes related to T2DM and chemical exposure, the above genes were merged with the TCEP-gene-T2DM or TCPP-gene-T2DM gene sets to obtain the two target gene sets. Finally, the
interaction network between the target gene set and target phenotype set was visualized using Cytoscape 3.8.0 (https://cytoscape.org/) if available. On the basis of this information, a
putative AOP was proposed, serving as a potential clue for understanding the mechanism through which TCPP/TCEP may contribute to the development of T2DM. RESULTS DEMOGRAPHIC CHARACTERISTICS
The median age and BMI of the overall participants were 48 years and 28.2 kg/m2, respectively, with interquartile ranges of 29 years and 8.8 kg/m2, respectively. A total of 50.52% of the
participants were female. Most of them were non-Hispanic White (63.84%), had an education above the college (62.24%), had high blood pressure (30.51%), or were non-gout (93.05%).
Approximately half of the participants were married (53.26%) and were examined or sampled between May and October (55.49%). A total of 40.81% of them smoked more than 100 cigarettes during
their life, and 37.54% of them consumed more than 12 alcohol drinks per year. Overall, 20.14% of people have a family income-to-poverty ratio higher than 1. A total of 42.15% of participants
reported that their close relatives had diabetes. The median intake of energy was 2036.63 kcal/m2. The median protein, carbohydrate, and fat intake were 76.60, 234.99, and 79.70 gm,
respectively. The medians of ALT and AST were 20.00 and 22.00 U/L, respectively. The median BUN and creatinine levels were 14.00 and 0.85 mg/dL, respectively. The median and quartiles of the
CDAI were 0.00 and (−1.98, 2.55), respectively. All demographic characteristics of people with or without diabetes are presented in detail in Table 1. There were statistically significant
differences in age, BMI, education, marital status, smoking status, blood pressure, gout status, family history of diabetes, energy intake, ALT, and BUN between people with and without
diabetes. CONCENTRATIONS OF CONTAMINATED METABOLITES All concentrations of contaminated metabolites are shown in Table 2. The exposure levels of OPEs are lower than those of PAEs. Among the
groups of PAEs, the MEP had the highest value, with a median of 26.081 µg/g Cr, followed by MBP (median 8.380 µg/g Cr), MECPP (median 7.066 µg/g Cr), and MiBP (median 6.908 µg/g Cr). The
MCPP had the lowest median concentration (0.968 µg/g Cr). Among the OPE metabolites, BDCP had the highest concentration, with a median of 1.068 µg/g Cr, followed by DPHP, with a median
concentration of 0.747 µg/g Cr. DBUP was detected at the lowest concentration, with a median of 0.108 µg/g Cr. Except for the greater correlations between metabolites of DEHP, such as MEHHP,
MEOHP, and MECPP, all the other correlations showed low to medium levels (Fig. S3). ASSOCIATION BETWEEN EACH CONTAMINATING METABOLITE AND DIABETES INCIDENCE STATUS In the first scenario,
individuals with a borderline clinical diagnosis and clinical diagnosis of diabetes were combined into the diabetes group, and exposure to most PAE metabolites, such as MEP, MnBP, MEHHP,
MEOHP, MECPP, and MCNP, was associated with an increased risk of diabetes according to the crude models. The BDCP concentration in OPEs is also positively correlated with the risk of
diabetes. After we adjusted for demographic variables such as age and sex, these associations became statistically insignificant. However, after further adjusting for CDAI components, the
association between PAE metabolite exposure and increased risk of diabetes was marginally statistically significant (Table S3). In the second scenario, where individuals with borderline
clinical diagnosis of diabetes were included in the normal population, the observed associations between exposure to additive metabolites and the risk of diabetes were similar (Table S4).
ASSOCIATION BETWEEN CONTAMINATED METABOLITE MIXTURE AND DIABETES In both the first and second scenarios, for every 1-SD increase in ERS, the risk of diabetes increased by 25 and 21%,
respectively (Table 3). BCEP and BCPP provided the highest weights for the positive relationships. The other four substances that provided higher weights were DBUP, BDCP, MCNP, and MEOHP
(Fig. S2b, c). Compared with the lowest tertile array of ERS, the middle tertile array of ERS increased the risk of diabetes by 17 and 41%, while the highest tertile array of ERS increased
the risk of diabetes by 1.77 times and 1.97 times, respectively. A chi-square test for trend indicated that exposure to the additive mixture (ERS) was positively associated with an increased
risk of diabetes in a linear manner. The sensitivity analysis results of the relationships between diabetes risk and the ERS constructed by the cross-validation method were also similar
(Table 3). MODIFYING EFFECTS OF THE CDAI ON THE ASSOCIATIONS BETWEEN ERS EXPOSURE AND DIABETES RISK The _p_ values for the interaction showed that there was an interaction between the ERS
and the CDAI. Regardless of the scenario or CDAI, ERS, and the CDAI had a positive interaction effect on the risk of diabetes, with values ranging from 9 to 90%. Interestingly, in the high
CDAI subgroup, the association between ERS and diabetes risk was lower than that in the low CDAI subgroup (Table 4). According to the quantile g-computation models, without adjusting for
confounding factors, the risk of diabetes increased by 27.4 and 36.0% when all metabolites increased by one quantile simultaneously (Table 5). When adjusting for confounding factors, the
risk of diabetes increased by 1.285 times and 1.393 times when all metabolites increased by one quantile simultaneously. According to both the coarse model and the adjusted model, when both
CDAI components and additive metabolites are included in the quantile g-computation, the risk of diabetes is no longer significantly increased when all metabolites (protecting CDAI
components) increase by one quantile simultaneously. Overall, MECPP and MCNP provided the greatest positive weights, while vitamin C and zinc provided the greatest negative weights (Fig. S4,
S5). POTENTIAL MECHANISMS For TCPP, 17 genes and three phenotypes were identified in relation to T2DM (Fig. 1A, B). After merging these genes with TCPP-gene-T2DM, four genes associated with
T2DM were identified: CPT1A (degree = 3), PPARA (degree = 2), PPARG (degree = 1), and FGF21 (degree = 1). The top two strongest genes (CPT1A and PPARA) and their related three phenotypes
(GO: 0009410; GO: 0032000; GO: 0006006) were considered potential molecular initiating events (MIEs) and key events (KEs) in the TCPP-induced AOP for T2DM, respectively. Therefore, a
putative AOP for TCPP-associated effects on T2DM was proposed, the sequence of which is described below. When exposed to TCPP, the CPT1A gene or PPARA gene is activated, resulting in an
enhanced response to xenobiotic stimulus (GO: 0009410), which positively regulates the fatty acid beta-oxidation (GO: 0032000), and further changes in glucose metabolic process (GO:
0006006), which eventually leads to T2DM (Fig. 1D). For TCEP, a total of 36 genes and 11 phenotypes were identified in relation to T2DM (Fig. 1A, C). After merging these genes with
TCEP-gene-T2DM, 14 target genes were found to be associated with T2DM (Fig. 1D). Among these genes, the two genes with the strongest association with T2DM were AKT1 (degree = 6) and HNF4A
(degree = 5) (Fig. 1E). These two genes and their ten related phenotypes (hsa04910; GO: 0032869; GO: 0042593; GO:0050796; GO:0009749; GO:0030073; GO:0009410; GO:0006006; GO: 0031016) are
considered as MIEs and KEs, respectively, in the TCEP-induced AOP for T2DM. Therefore, a putative AOP network (Fig. 1D) for TCEP-associated effects on T2DM was proposed with a sequence of
events described below. When exposed to TCEP, the AKT1A or HNF4A genes are activated in response to exogenous stimuli (GO: 0009410) or in response to glucose (GO: 0009749) and then
positively regulate the process of glucose metabolism (GO: 0010907), increase the cellular response to insulin stimulus (GO: 0032869), or regulate insulin secretion (GO: 0050796), further
disturbing the process of glucose metabolism (GO: 0006006) or insulin secretion (GO: 0030073) to destroy glucose homeostasis (GO: 0042593) or pancreas development (GO: 0031016); these
changes ultimately lead to the development of T2DM. Another possibility is that the activation of the AKT1A or HNF4A gene leads to the development of T2DM through the aberrant insulin
signaling pathway (hsa04910). DISCUSSION In summary, the risk of diabetes is significantly increased when individuals are exposed to a mixture of PAE and OPE metabolites, with BCEP, BCPP,
MCNP, and MECPP being key active substances. The simultaneous consumption of antioxidant foods, especially foods containing vitamin C and zinc, can alleviate the risk of diabetes caused by
PAEs and OPEs. Previous studies have not investigated the association between mixed exposure to PAEs or OPEs and the risk of diabetes, but harmful effects on other health issues, such as
adverse reproductive outcomes [11], childhood asthma [10], and neurodevelopmental deficits [12], have been reported. Regarding exposure to PAEs alone, data from the Korean National
Environmental Health Survey (KoNEHS) showed significant positive associations between diabetes and PAEs, and ORs of the highest quartile were for DEHP (2.49, 95% CI = 1.43–4.33), MEHHP
(3.03, 95% CI = 1.69–5.45), MEOHP (1.74, 95% CI = 1.03–2.92), MECCP (1.67, 95% CI = 1.02–2.73), MnBP (2.17, 95% CI = 1.28–3.66), MBzP (1.89, 95% CI = 1.11–3.22), and MCPP (2.01, 95% CI =
1.19–3.42) compared to the first quartile of PAEs [13]. A case‒control study in China revealed significant positive associations between urinary concentrations of the most studied PAE
metabolites and T2DM, with odd ratios indicating extreme PAE quartiles ranging from 2.09 to 40.53, whereas two secondary metabolites, MECPP and mono[(2-carboxymethyl)hexyl] phthalate
(MCMHP), showed significant inverse relationships with T2DM [34]. Women with higher levels of mono-_n_-butyl phthalate (MnBP), mono-isobutyl phthalate (MiBP), monobenzyl phthalate (MBzP),
mono-(3-carboxypropyl) phthalate (MCPP), and three di-(2-ethylhexyl) phthalate metabolites (ΣDEHP) had greater odds of diabetes than women with the lowest levels of these phthalates. Women
in the highest quartile for MBzP and MiBP had almost twice the odds of having diabetes [OR = 1.96 (95% CI: 1.11, 3.47) and OR = 1.95 (95% CI: 0.99, 3.85), respectively] compared with women
in the lowest quartile [35]. At present, there is insufficient evidence about the association between combined exposure to multiple PAE metabolites and diabetes [36]. For OPE exposure alone,
according to the data from the NHANES 1999-2008 and 2011-2012, DMTP was significantly associated with higher levels of serum insulin (β = 0.21, 95% CI = 0.06-0.36) and HOMA-IR (β = 0.08,
95% CI = 0.02-0.14) and increased odds of T2DM (OR = 1.05, 95% CI = 1.01–1.08). Other OPEs were not significantly associated with serum markers of glucose homeostasis or T2DM [15]. Evidence
from the China BAPE Study [14] demonstrated that exposure to five OPE mixtures (trimethylolpropane phosphate, triphenyl phosphate, tri-iso-butyl phosphate, dibutyl phosphate, and diphenyl
phosphate) was associated with increased levels of glycometabolic markers [14]. A comparison between these research results and the results of this study is difficult. The demographic
characteristics and OPE exposure levels differed, as did the sample size, study design and statistical analysis methods. For instance, all the evidence, including this study, comes from
cross-sectional surveys or case‒control studies, which are designed to make it difficult to infer causality. More prospective research evidence is needed in the future to explore the causal
relationships between PAE and OPE exposure and diabetes. However, the biological mechanism underlying the increased risk of diabetes caused by these plastic additives is still unclear. By
mining public database resources and bioinformatics analysis, we proposed that two key substances, TCPP and TCEP, may lead to AOP in T2DM, suggesting that the enhanced response to exogenous
substances regulates fatty acid beta-oxidation or glucose metabolism, further disrupting glucose metabolism disorders and ultimately leading to T2DM. In addition, abnormalities in the
insulin signaling pathway may also be one of the possible mechanisms. This finding is consistent with previous findings [14]. This putative AOP model was proposed based on the data from
multiomics analyses. It has been suggested that triggers of molecular initiation events (e.g., insulin receptor and glucose transporter type 4) with subsequent key events, including
disruptions in signal transduction pathways (e.g., phosphatidylinositol 3-kinase/protein kinase B and insulin secretion signaling) and biological functions (glucose uptake and insulin
secretion), may constitute the diabetogenic effects of OPEs [14]. Another possible mechanism is oxidative stress and inflammation. Increased oxidative stress and inflammation can lead to
insulin resistance, impaired insulin secretion, and, ultimately, T2DM [37,38,39]. The inflammatory response and metabolic regulation are highly coordinated because abnormal inflammatory
function can lead to a series of chronic metabolic diseases, including T2DM [40]. Phthalates are thought to be important environmental risk factors that may influence inflammation and
oxidative stress [41,42,43]. Multiple metabolites of organophosphate flame retardants and their mixed exposures have also been found to be associated with elevated levels of biomarkers of
oxidative stress [44]. An animal experiment showed that TCPP induced the overexpression of adipogenic genes and inhibited the expression of fatty acid β-oxidation genes. Excessive lipid
synthesis and insufficient consumption can damage the antioxidant system and lead to the overexpression of fatty acid β-oxidation proinflammatory cytokines, which triggers oxidative damage
and inflammation [45]. These findings seem to coincide with the results of this study. This study identified fatty acid beta-oxidation as one of the important phenotypes associated with
potential TCPP-associated AOP in patients with T2DM. In addition, in the TCEP-induced AOP, the target genes also include IL6, PPARA, and PPARGC1A, which are closely related to inflammation
and oxidative stress. These changes may also constitute the mechanism by which the antioxidant foods found in this study mitigate the increased risk of diabetes from mixed exposure to
plastic additives. There are still many shortcomings that need to be taken into consideration in this study. First, this was a cross-sectional survey study design, which has the inherent
drawback of not being able to determine the chronological order of exposure and outcome and cannot account for the causal relationship between exposure to plastic additives and diabetes.
Longitudinal studies would be more suitable to establish temporal relationships between exposure to plastic additives and the development of diabetes. Second, there may still be unmeasured
confounding variables that could influence the observed associations. Factors such as dietary habits, lifestyle factors, genetic predispositions were not fully accounted. Third, in addition
to plasticizers and flame retardants, plastic products contain other additives, polymer matrices, degradation products, and adsorbed pollutants that pose a threat to human health. Future
research should aim to explore a wider range of plastic product chemicals to better understand their health effects. Forth, the type of diabetes in this study was not detailed as to whether
it was type 1 or type 2. The pathogenesis of these two types of diabetes may be different [46, 47], so this limits the study’s ability to draw specific conclusions about the association
between plastic additives and each type of diabetes. Finally, we utilized two commonly used adaptive elastic network models and quantile g computation models to evaluate the effects of mixed
chemical exposure. Although the results of these two studies are consistent and suggest that mixed exposure to PAEs and OPEs is associated with an increased risk of diabetes, slight
differences in the key substances were found. This approach is not conducive to formulating further precise intervention measures or informing the direction of policy reform. CONCLUSION In
conclusion, the combination of plastic plasticizers and flame retardants, such as PAEs and OPEs, increases the risk of developing diabetes. Special attention should be given to reducing
contact and exposure to parent chemicals such as TCEP (the parent chemical of BCEP), TCPP (the parent chemical of BCPP), DCNP (the parent chemical of MCNP), and DEHP (the parent chemical of
MECPP). It is recommended that individuals consume more antioxidant foods, such as vitamin C and zinc, which may reduce the risk of diabetes caused by exposure to plastic additives. In the
future, it is necessary to incorporate a wider range of plastic product chemicals to explore the impact of plastic pollution on human health. DATA AVAILABILITY The datasets generated during
and/or analysed during the current study are available in the NHANES website (https://www.cdc.gov/nchs/nhanes/index.htm). REFERENCES * Rodrigues MO, Abrantes N, Goncalves F, Nogueira H,
Marques JC, Goncalves A. Impacts of plastic products used in daily life on the environment and human health: what is known? Environ Toxicol Pharm. 2019;72:103239. Article CAS Google
Scholar * Hoellein T, Rojas M, Pink A, Gasior J, Kelly J. Anthropogenic litter in urban freshwater ecosystems: distribution and microbial interactions. PLos ONE. 2014;9:e98485. Article
PubMed PubMed Central Google Scholar * Seewoo BJ, Goodes LM, Mofflin L, Mulders YR, Wong EV, Toshniwal P, et al. The plastic health map: a systematic evidence map of human health studies
on plastic-associated chemicals. Environ Int. 2023;181:108225. Article CAS PubMed Google Scholar * Yan S, Wu H, Qin J, Zha J, Wang Z. Halogen-free organophosphorus flame retardants
caused oxidative stress and multixenobiotic resistance in Asian freshwater clams (Corbicula fluminea). Environ Pollut. 2017;225:559–68. Article CAS PubMed Google Scholar * Liu Y, Gong S,
Ye L, Li J, Liu C, Chen D, et al. Organophosphate (OP) diesters and a review of sources, chemical properties, environmental occurrence, adverse effects, and future directions. Environ Int.
2021;155:106691. Article CAS PubMed Google Scholar * Zhang H, Hua Y, Chen J, Li X, Bai X, Wang H. Organism-derived phthalate derivatives as bioactive natural products. J Environ Sci
Health C Environ Carcinog Ecotoxicol Rev. 2018;36:125–44. Article CAS PubMed Google Scholar * Xie Z, Zhang X, Liu F, Xie Y, Sun B, Wu J, et al. First determination of elevated levels of
plastic additives in finless porpoises from the South China Sea. J Hazard Mater. 2024;465:133389. Article CAS PubMed Google Scholar * Wang C, Su ZH, He MJ. Dynamic variation and
inhalation exposure of organophosphates esters and phthalic acid esters in face masks. Environ Pollut. 2023;316:120703. Article CAS PubMed Google Scholar * Luongo G, Ostman C.
Organophosphate and phthalate esters in settled dust from apartment buildings in Stockholm. Indoor Air. 2016;26:414–25. Article CAS PubMed Google Scholar * Chen Z, Li F, Fu L, Xia Y, Luo
Y, Guo A, et al. Role of inflammatory lipid and fatty acid metabolic abnormalities induced by plastic additives exposure in childhood asthma. J Environ Sci. 2024;137:172–80. Article CAS
Google Scholar * Yang P, Xie J, Huang S, Li X, Deng L, Zhang J, et al. Cocktail” of environmental chemicals and early reproductive outcomes of IVF: The insight from paternal and maternal
exposure. J Environ Manag. 2023;348:119462. Article CAS Google Scholar * Ramos AM, Herring AH, Villanger GD, Thomsen C, Sakhi AK, Cequier E, et al. The association of prenatal phthalates,
organophosphorous pesticides, and organophosphate esters with early child language ability in Norway. Environ Res. 2023;225:115508. Article CAS PubMed PubMed Central Google Scholar *
Nam DJ, Kim Y, Yang EH, Lee HC, Ryoo JH. Relationship between urinary phthalate metabolites and diabetes: Korean National Environmental Health Survey (KoNEHS) cycle 3 (2015-2017). Ann Occup
Environ Med. 2020;32:e34. Article PubMed PubMed Central Google Scholar * Ding E, Deng F, Fang J, Li T, Hou M, Liu J, et al. Association between organophosphate ester exposure and insulin
resistance with glycometabolic disorders among older Chinese adults 60-69 years of age: evidence from the China BAPE study. Environ Health Perspect. 2023;131:47009. Article CAS PubMed
Google Scholar * Bo Y, Zhu Y. Organophosphate esters exposure in relation to glucose homeostasis and type 2 diabetes in adults: a national cross-sectional study from the national health and
nutrition survey. Chemosphere. 2022;301:134669. Article CAS PubMed Google Scholar * Pogrmic-Majkic K, Samardzija ND, Tesic B, Fa NS, Kokai D, Stanic B, et al. Mapping DEHP to the
adverse outcome pathway network for human female reproductive toxicity. Arch Toxicol. 2022;96:2799–813. Article CAS PubMed PubMed Central Google Scholar * Zhang T, Wang S, Li L, Zhu A,
Wang Q. Associating diethylhexyl phthalate to gestational diabetes mellitus via adverse outcome pathways using a network-based approach. Sci Total Environ. 2022;824:153932. Article CAS
PubMed Google Scholar * Bozic D, Zivancevic K, Baralic K, Miljakovic EA, Djordjevic AB, Curcic M, et al. Conducting bioinformatics analysis to predict sulforaphane-triggered adverse
outcome pathways in healthy human cells. Biomed Pharmacother. 2023;160:114316. Article CAS PubMed Google Scholar * Chai Z, Zhao C, Jin Y, Wang Y, Zou P, Ling X, et al. Generating adverse
outcome pathway (AOP) of inorganic arsenic-induced adult male reproductive impairment via integration of phenotypic analysis in comparative toxicogenomics database (CTD) and AOP wiki.
Toxicol Appl Pharm. 2021;411:115370. Article CAS Google Scholar * Li AJ, Martinez-Moral MP, Al-Malki AL, Al-Ghamdi MA, Al-Bazi MM, Kumosani TA, et al. Mediation analysis for the
relationship between urinary phthalate metabolites and type 2 diabetes via oxidative stress in a population in Jeddah, Saudi Arabia. Environ Int. 2019;126:153–61. Article CAS PubMed
Google Scholar * Dong R, Chen J, Zheng J, Zhang M, Zhang H, Wu M, et al. The role of oxidative stress in cardiometabolic risk related to phthalate exposure in elderly diabetic patients from
Shanghai. Environ Int. 2018;121:340–8. Article CAS PubMed Google Scholar * Li MC, Minguez-Alarcon L, Bellavia A, Williams PL, James-Todd T, Hauser R, et al. Serum beta-carotene modifies
the association between phthalate mixtures and insulin resistance: the National Health and Nutrition Examination Survey 2003-2006. Environ Res. 2019;178:108729. Article CAS PubMed PubMed
Central Google Scholar * Jayatilaka NK, Restrepo P, Davis Z, Vidal M, Calafat AM, Ospina M. Quantification of 16 urinary biomarkers of exposure to flame retardants, plasticizers, and
organophosphate insecticides for biomonitoring studies. Chemosphere. 2019;235:481–91. Article CAS PubMed PubMed Central Google Scholar * Silva MJ, Samandar E, Preau JJ, Reidy JA,
Needham LL, Calafat AM. Quantification of 22 phthalate metabolites in human urine. J Chromatogr B Anal Technol Biomed Life Sci. 2007;860:106–12. Article CAS Google Scholar * Li X, Zheng
N, Yu Y, Zhang W, Sun S, An Q, et al. Individual and combined effects of phthalate metabolites on eczema in the United States population. Environ Res. 2024;240:117459. Article CAS PubMed
Google Scholar * Tan Z, Meng Y, Li L, Wu Y, Liu C, Dong W, et al. Association of dietary fiber, composite dietary antioxidant index and risk of death in tumor survivors: National Health and
Nutrition Examination Survey 2001-2018. Nutrients. 2023;15:2968. Article PubMed PubMed Central Google Scholar * Lumley T. Complex surveys: a guide to analysis using R. Wiley, 2010. *
Cathey AL, Watkins DJ, Rosario ZY, Velez C, Mukherjee B, Alshawabkeh AN, et al. Biomarkers of exposure to phthalate mixtures and adverse birth outcomes in a Puerto Rico birth cohort. Environ
Health Perspect. 2022;130:37009. Article CAS PubMed Google Scholar * Burgess S, Thompson SG. Use of allele scores as instrumental variables for Mendelian randomization. Int J Epidemiol.
2013;42:1134–44. Article PubMed PubMed Central Google Scholar * Yang Y, Gu Y, Zou H. gcdnet: the (Adaptive) LASSO and elastic net penalized least squares, logistic regression, hybrid
huberized support vector machines, squared hinge loss support vector machines and expectile regression using a fast generalized coordinate descent algorithm. (2022). * Kuhn M. Building
predictive models in R using the caret package. J Stat Softw. 2008;28:1–26. * Keil A. qgcomp: quantile G-computation. 2022. * Yu G, Wang LG, Han Y, He QY. clusterProfiler: an R package for
comparing biological themes among gene clusters. OMICS. 2012;16:284–7. Article CAS PubMed PubMed Central Google Scholar * Duan Y, Sun H, Han L, Chen L. Association between phthalate
exposure and glycosylated hemoglobin, fasting glucose, and type 2 diabetes mellitus: a case-control study in China. Sci Total Environ. 2019;670:41–9. Article CAS PubMed Google Scholar *
James-Todd T, Stahlhut R, Meeker JD, Powell SG, Hauser R, Huang T, et al. Urinary phthalate metabolite concentrations and diabetes among women in the National Health and Nutrition
Examination Survey (NHANES) 2001-2008. Environ Health Perspect. 2012;120:1307–13. Article PubMed PubMed Central Google Scholar * Bai PY, Wittert G, Taylor AW, Martin SA, Milne RW,
Jenkins AJ, et al. The association between total phthalate concentration and non-communicable diseases and chronic inflammation in South Australian urban dwelling men. Environ Res.
2017;158:366–72. Article CAS PubMed Google Scholar * Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk TP. Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol
Pharmacol. 2019;70. * Yaribeygi H, Sathyapalan T, Atkin SL, Sahebkar A. Molecular mechanisms linking oxidative stress and diabetes mellitus. Oxid Med Cell Longev. 2020;2020:8609213. Article
PubMed PubMed Central Google Scholar * Rohm TV, Meier DT, Olefsky JM, Donath MY. Inflammation in obesity, diabetes, and related disorders. Immunity. 2022;55:31–55. Article CAS PubMed
PubMed Central Google Scholar * Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–7. Article CAS PubMed Google Scholar * Jin S, Cui S, Mu X, Liu Z, Han Y,
Cui T, et al. Exposure to phthalates and their alternatives in relation to biomarkers of inflammation and oxidative stress in adults: evidence from NHANES 2017-2018. Environ Sci Pollut Res
Int. 2023;30:123770–84. Article CAS PubMed Google Scholar * Ferguson KK, Loch-Caruso R, Meeker JD. Exploration of oxidative stress and inflammatory markers in relation to urinary
phthalate metabolites: NHANES 1999-2006. Environ Sci Technol. 2012;46:477–85. Article CAS PubMed Google Scholar * Oluranti OI, Alabi BA, Michael OS, Ojo AO, Fatokun BP. Rutin prevents
cardiac oxidative stress and inflammation induced by bisphenol A and dibutyl phthalate exposure via NRF-2/NF-kappaB pathway. Life Sci. 2021;284:119878. Article CAS PubMed Google Scholar
* Ait BY, Bastiaensen M, Araki A, Goudarzi H, Konno S, Ito S, et al. Multiple exposures to organophosphate flame retardants alter urinary oxidative stress biomarkers among children: the
Hokkaido Study. Environ Int. 2019;131:105003. Article Google Scholar * Liu Z, Su Z, Wang M, Chen T, Cui Z, Chen X, et al. Computerized characterization of spinal structures on MRI and
clinical significance of 3D reconstruction of lumbosacral intervertebral foramen. Pain Physician. 2022;25:E27–35. PubMed Google Scholar * Rea S, Della-Morte D, Pacifici F, Capuani B,
Pastore D, Coppola A, et al. Insulin and exendin-4 reduced mutated Huntingtin accumulation in neuronal cells. Front Pharm. 2020;11:779. Article CAS Google Scholar * Andreadi A, Muscoli S,
Tajmir R, Meloni M, Muscoli C, Ilari S, et al. Recent pharmacological options in type 2 diabetes and synergic mechanism in cardiovascular disease. Int J Mol Sci. 2023;24:1646. Article CAS
PubMed PubMed Central Google Scholar Download references FUNDING This work was supported by the Science and Technology Bureau of Jinhua [grant number 2022-4-130]; the Research Project
for Outstanding Young People in Universities of Anhui Province [grant number 2023AH030118]; the National Natural Science Foundation of China [grant number 82103856]; and the MOE Key
Laboratory of Population Health Across Life Cycle [grant number JK20204]. AUTHOR INFORMATION Author notes * These authors contributed equally: Yang Yang, Cheng Zhang. AUTHORS AND
AFFILIATIONS * Department of Prevention and Health Care, Affiliated Jinhua Hospital, Zhejiang University School of Medicine, Jinhua, 321000, Zhejiang, China Yang Yang * Department of
Oncology, The First Affiliated Hospital of Anhui Medical University, No.218 Jixi Road, Hefei, 230022, Anhui, China Cheng Zhang * Department of Biostatistics, Anhui Provincial Cancer
Institute, No.218 Jixi Road, Hefei, 230022, Anhui, China Cheng Zhang * Department of Pediatrics, the First Affiliated Hospital of Anhui Medical University, No.218 Jixi Road, Hefei, 230022,
Anhui, China Hui Gao Authors * Yang Yang View author publications You can also search for this author inPubMed Google Scholar * Cheng Zhang View author publications You can also search for
this author inPubMed Google Scholar * Hui Gao View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Yang Yang: Conceptualization, methodology,
software, investigation, supervision, funding acquisition, and writing—reviewing and editing. Zhang Cheng: Data curation, visualization, formal analysis, and writing—reviewing and editing.
Gao Hui: Conceptualization, writing—original draft preparation, supervision, and funding acquisition. CORRESPONDING AUTHOR Correspondence to Hui Gao. ETHICS DECLARATIONS COMPETING INTERESTS
The authors declare no competing interests. ETHICS APPROVAL AND CONSENT TO PARTICIPATE (1) All methods were performed in accordance with the relevant guidelines and regulations. (2) NHANES
is a publicly free database, and it was approved by the NCHS Research Ethics Review Board under the protocol numbers of #2018-01 and #2011-17. (3) Informed consent was obtained from all
participants in NHANES project 2011–2018. (4) No identifiable images from human research participants are involved. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral
with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION TABLE OF SUPPLEMENTARY CONTENTS FIGURE S1 FIGURE S2 FIGURE S3 FIGURE S4
FIGURE S5 RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and
reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if
changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the
material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to
obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS
ARTICLE Yang, Y., Zhang, C. & Gao, H. Potential mechanisms and modifications of dietary antioxidants on the associations between co-exposure to plastic additives and diabetes. _Nutr.
Diabetes_ 14, 72 (2024). https://doi.org/10.1038/s41387-024-00330-1 Download citation * Received: 19 February 2024 * Revised: 19 August 2024 * Accepted: 22 August 2024 * Published: 03
September 2024 * DOI: https://doi.org/10.1038/s41387-024-00330-1 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a
shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative