Play all audios:
ABSTRACT STUDY DESIGN Cross-sectional study. OBJECTIVE Describe and compare ambulatory performance and cognitive capacity in relation to muscle function in an adult cohort with spina bifida.
Also, explore factors associated with ambulation in participants with muscle function level 3. SETTING Specialist clinic for adults with spinal cord disorders in Stockholm, Sweden. METHODS
A total regional cohort of adults (_n_ = 219) with spina bifida was invited, 196 (104 women, mean age 35 years, SD 13 years) participated. Mode of mobility, cognitive capacity and muscle
function were investigated. For participants with muscle function level 3, factors associated with ambulation were investigated using multivariate logistic regression analysis. RESULTS In
all, 84 participants (42%) were community ambulators, 22 (12%) household ambulators and 90 (46%) wheelchair users. There was a linear association between the lower degree of muscle function
and scoliosis (_P_ < 0.001). Mode of mobility varied despite similar muscle prerequisites in participants with muscle function level 3 (_n_ = 58). Factors associated with ambulation in
participants with muscle function level 3 were the absence of scoliosis, lower BMI and higher cognitive capacity. CONCLUSIONS Cognitive capacity and mode of mobility varied widely across the
cohort. However, in participants with muscle function level 3, despite similar muscular prerequisites, a large variation in the mode of mobility was found, suggesting that other factors
were involved. It is important to prevent scoliosis, support a healthy lifestyle, as well as offer cognitive screening and support to promote ambulatory function and optimise independence in
the everyday lives of adults with spina bifida. You have full access to this article via your institution. Download PDF SIMILAR CONTENT BEING VIEWED BY OTHERS RELATIONSHIP OF SAGITTAL
SPINAL ALIGNMENT WITH LOW BACK PAIN AND PHYSICAL PERFORMANCE IN THE GENERAL POPULATION Article Open access 18 October 2021 AN OBSERVATIONAL STUDY ON BODY MASS INDEX DURING REHABILITATION AND
FOLLOW-UP IN PEOPLE WITH SPINAL CORD INJURY IN DENMARK Article 03 January 2022 CHANGES IN CARDIORESPIRATORY FITNESS AND ACTIVITY LEVELS OVER THE FIRST YEAR AFTER DISCHARGE IN AMBULATORY
PERSONS WITH RECENT INCOMPLETE SPINAL CORD INJURY Article Open access 09 July 2020 INTRODUCTION Spina bifida (SB) is a complex congenital neural tube malformation involving multiple body
systems [1, 2] leading to a multifaceted disability. Due to better medical treatment, 75% of people with SB reach early adulthood [3]. In most cases, SB includes impaired motor and sensory
function, leading to partial or complete paralysis and/or sensory loss below the malformation. Mode of mobility ranges from ambulation in the community to the use of a powered wheelchair.
Musculoskeletal conditions, pain, bladder and bowel-related problems, and pressure ulcers are common [1]. Further, tethered cord syndrome and orthopaedic conditions such as contractures, hip
dislocations, scoliosis, and kyphosis have been frequently reported [2, 4]. Most people with open SB have shunted hydrocephalus, migration abnormalities of the central nervous system and
Chiari II malformation [2, 4]. A higher level of spinal lesion is a marker of more severe anomalous brain development which, in turn, is associated with reduced independence [5]. The
cognitive impairments, often affecting executive function, prospective memory, timing and time management [6], are highly variable between persons [2]. Timing and attention impairments are
associated with hydrocephalus [7] and brain dysmorphologies, such as the Chiari II malformation [8], while movement impairments are caused by spinal cord dysfunction and cerebellar
dysmorphologies that influence sensory-motor timing and motor regulation [5]. Impaired gait function [9,10,11,12] is common and associated with the level and degree of spinal malformation.
Gait is a complex activity requiring interactions between supraspinal locomotor and cognitive networks [13]. Long-term functional outcomes such as ambulation and sitting balance are closely
related to the neurological level of malformation [12, 14, 15], but the mode of mobility is difficult to predict since it is influenced by factors such as age, body mass index (BMI),
orthopaedic deformities and cognitive status [15]. Ambulatory persons with sacral or low-lumbar SB usually retain their walking ability into adulthood, whereas those with a high-lumbar or
thoracic level of malformation often become wheelchair users [4, 14, 16]. A key component for ambulatory performance is an adequate function in knee extensors [16], corresponding to muscle
function (MF) level 3, consistent with the classification of muscle function groups [9]. The aim of this paper was to describe and compare ambulatory performance and cognitive capacity in
relation to MF in an adult cohort with SB. The paper also aimed to explore factors associated with ambulation in adults with MF level 3. MATERIALS AND METHODS STUDY DESIGN A cross-sectional
study conducted by a multidisciplinary team at a regional clinic for spinal cord disorders, investigating medical, physical and cognitive functioning associated with the level of muscle
function. PARTICIPANTS A near-total regional cohort of adults (≥18 years) with SB (_n_ = 219) were consecutively invited to participate in conjunction with regular clinical follow-up. DATA
COLLECTION PROCEDURE The study is part of a larger research project aiming to describe the living and health issues of a regional cohort of adults with SB enrolled at a specialised clinic
for adults with spinal cord disorders [17]. In short, the data collection was conducted through regular clinical assessments and structured interviews by three persons, a physiotherapist
(MB), an occupational therapist (supervised by GH) and a nurse who were part of the clinic’s SB multi-professional team with over 10 years experience of adults with SB. Medical records were
used to validate the provided information. Muscle function was assessed via manual muscle testing of the lower extremities using a 0–5 graded scale [18], and participants were classified
according to the categories developed by Bartonek [9], with an additional category for those who had no loss of muscle strength, Table 1. For participants with an asymmetrical motor
function, the most severely impaired side was used for classification [15] in order to avoid overrating their function. As knee extensor function is a key component of gait, participants in
MF level 3 were further explored. Hip, knee and ankle joint contractures of more than 20 degrees were registered [9]. A clinical examination including visual inspection (by the
physiotherapist) for scoliosis in a sitting position was used in combination with participant statement and medical records to register scoliosis and/or previous spinal surgery resulting
from scoliosis. Both conditions are hereinafter referred to as scoliosis. The clinical examination also included height (m) in a standing position or, for participants who were unable to
stand, in lying position (from joint to joint in case of contractures) and measurement of weight (kg). BMI was calculated (kg/m2). The American Spinal Injury Association (ASIA) Impairment
Scale (AIS) was used according to the International Standards for Neurological Classification of Spinal Cord Injury [19]. Each interview included sociodemographic, medical and physical
factors, presence, and location of pain on examination day (yes/no), use of assistive devices and orthoses, and self-reported maximal walking distance (verified by control questions to
ensure accuracy and categorised as: >1000 m, ≤1000 m, ≤100 m, ≤10 m, 0 m, Table 3). Further, the ambulatory function was assessed according to Hoffer [14, 20]. The participants were
dichotomised as ambulatory (community and household ambulators) or wheelchair users (non-functional ambulators and wheelchair users). Physical exercise was self-reported and categorised as
no physical exercise, moderate exercise (minimum 30 min, 1–2 times per week) and vigorous physical exercise (minimum 30 minutes at least three times weekly). This was also verified by the
assessors via control questions about their exercise regimes. Cognitive capacity was assessed using three tests. The coding test for psychomotor speed and executive function and the block
design test for spatial/psychomotor ability and executive function, both from the Wechsler Abbreviated Scale of Intelligence, WASI [21]. Further, the FAS test was used, a phonemic word
fluency test for verbal executive ability and mental speed [22]. Results for the subtests were scaled according to age, with a mean of 10 (SD 3) and a range of 1–19. To calculate the scores
on the FAS test, the results were first converted to _Z_ values. DATA ANALYSIS The Shapiro–Wilk test (_P_ < 0.05) was used to analyse normal distribution. Descriptive data were presented
as numbers and proportions. Mean and standard deviation (SD) were used for normally distributed variables, while median (Md) and interquartile ranges (IQR) were used for non-normal
distributions. The differences were analysed using the Chi-square test for dichotomous variables, one-way ANOVA for normally distributed variables with more than two groups, Student’s _t_
test for normally distributed variables comparing two groups, and the Mann–Whitney _U_ test for variables with non-normal distribution. The Cochran–Armitage test of trend was used to
determine whether there was a linear association between the muscle function and dichotomic variable. Statistically significant differences are presented. For persons with MF level 3,
factors potentially associated with ambulation [15, 23] age [15], sex, height, weight, BMI [9], scoliosis [9, 23], daily bladder and/or bowel incontinence, sensory function in the feet and
cognitive capacity [15] (the coding test [21], FAS test [22] and block design test [21]) were investigated using bivariate logistic regression analysis. According to the “rule of thumb” of
ten persons per variable, five variables were included as there were 50 participants [24]. Age was considered a possible confounder and was therefore included, together with the variables
with the lowest _P_ values. A multivariate model was performed using backwards enter mode. The collinearity between the variables in the model was investigated using Spearman’s rank
correlations and were pre-set at less than 0.6. The results from the regression analysis were presented with odds ratios (OR) including 95% confidence intervals (CI) and Hosmer–Lemeshow
goodness-of-fit statistics were used for model fit of the final multivariate model. The analyses were performed using SPSS version 24 (IBM Corp., Armonk, NY, USA). The statistical
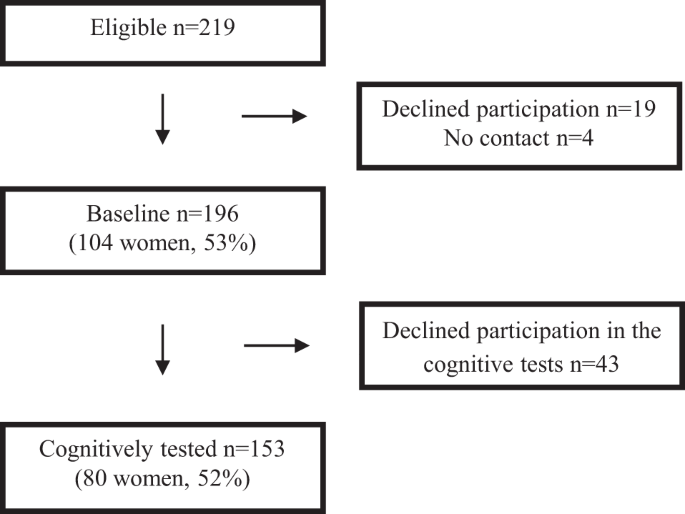
significance was determined at _P_ ≤ 0.05. RESULTS There were 196 persons (89%) (104 women, 53%) with a mean age of 35 years (SD 13) invited to participate, Table 2, Fig. 1. Nineteen persons
declined follow-up and four did not respond. Seventy-eight percent, 153 out of 196 (80 women), participated in the cognitive assessment, Fig. 1. Of those who declined, some had previously
completed another neuropsychiatric assessment (not included in the present investigation), but in most cases, no reason was given. No significant differences were seen in age, sex,
prevalence of hydrocephalus, muscle or ambulatory function between those persons who participated in the cognitive assessment and those who declined. The cohort comprised 84 (42%) community
ambulators, 22 household ambulators (12%) and 90 (46%) wheelchair users (including non-functional walkers). Out of 196 participants, 179 (91%) had myelomeningocele, 13 (7%) lipomeningocele
and four (2%) spina bifida occulta. The most common level of neurological impairment according to the American Spinal Injury Association Impairment Scale (AIS) [19] was L3 in 82 participants
(41%). Mean height was 158 cm (SD 14), mean weight 69 kg (SD 19) and median BMI 27 (IQR 23–31). For demographic and structural characteristics see Table 2, for mobility and the use of
orthoses and assistive devices see Table 3. There was a significant difference in mean height between participants in MF level 0, 1 and 2 compared to participants in MF level 3, 4 and 5 (_P_
< 0.000) with the successively lower height of participants in MF level 1 (170 cm) to MF level 5 (145 cm). Further, there was a significant linear association between a lower degree of
muscular function and a higher proportion of participants with hydrocephalus (_P_ < 0.001), a higher proportion of participants with contractures in the lower extremities (_P_ < 0.001)
and scoliosis (_P_ < 0.001). There was only a significant difference in BMI between MF level 2 and 4 (_P_ = 0.033). Other variables were not associated (_P_ > 0.05) with MF level. In
the subtests for cognitive capacity, participants with MF level 4 and 5 had significantly lower scores. On the coding tests, participants with MF level 5 showed significantly lower results
compared to all other MF levels. Further, in the block design test, participants in MF level 5 had significantly lower results compared to all other MF levels, except MF level 4. On the FAS
test, participants with MF level 4 and 5 showed significantly lower results compared to participants with MF levels 2 and 3, Table 3. For participants with MF level 3, the most common level
of malformation, (29 women), 16 (28%) were community ambulators, 19 (32%) household ambulators and 23 (40%) wheelchair users (including the non-functional ambulators). The community
ambulators (mean age 39 years, SD 14) and the wheelchair users (mean age 37 years, SD 11) were significantly older than the household ambulators (mean age 29 years, SD 11) (_P_ = 0.012 and
_P_ = 0.017). The ambulatory participants had a lower mean BMI (26, SD 3.7 and 27, SD 5.6) than the wheelchair users (mean of 32 with two outliers with a BMI of 47 and 49, SD 7.4) (_P_ =
0.001). Further, there were no significant differences regarding prevalence of pain, tethered cord symptoms or results from the cognitive tests. For participants with MF level 3, the
bivariate logistic regression analysis showed that sex, height, BMI and scoliosis were significantly associated with mode of mobility, Table 4. These variables were therefore included in the
multivariate model, together with age (possible confounder) and the coding test (_P_ value <0.1). Height was not included in the multivariate analysis as it is closely associated with
BMI, which was considered more relevant for ambulation [15]. In the final multivariate model, BMI, scoliosis and the coding test were independently associated with ambulation, Table 4. For
every increasing unit of BMI, the OR of being ambulatory decreased by ~24% (95% CI 0.613–0.948, _P_ = 0.015). The participants with scoliosis had an ~97% lower OR (95% CI 0.002–0.415, _P_ =
0.009) of being ambulatory. For every increasing unit of the coding test, the OR of being ambulatory increased by approximately 7% (95% CI 1.007–1.143, _P_ = 0.030). DISCUSSION In this
cohort of nearly 200 adults with SB, ambulatory function and cognitive capacity were investigated in relation to different muscle function. Interestingly, in participants with MF levels 2–4
(corresponding to a lumbar malformation), ambulatory function was highly variable. Mode of mobility, use of assistive devices and orthoses, as well as maximal walking distance, varied
between participants with similar muscular prerequisites for walking, indicating that ambulatory function is complex and depends on multiple factors. In the most common MF level (level 3),
the ambulatory participants had a lower BMI, lower presence of scoliosis and higher cognitive capacity. Walking aids were used by over half (51%) of the ambulatory persons with MF 3 and by
15% in MF2 (Table 3), indicating that ambulation is highly challenging for persons with MF level 3 category. Thus, optimising assistive devices is a prerequisite for promoting functional
independence in persons with SB. Combining ambulation and wheelchair at different circumstances could be beneficial and enable flexibility in everyday life. Wheelchair use could be regarded
as a limiting factor, associated with barriers [25], although it is also the most essential mobility device [25]. Thus, a retained walking function (when possible) could enhance the quality
of life as it may improve accessibility and social availability. However, clinical experience and the experience of adults with SB [26] indicate that if walking is too challenging using a
wheelchair could be a viable decision. Adults with SB seem positive about exploring their cognitive capacity, potentially reflecting a perceived gap of knowledge as most of the participants
(78%) approved the testing. For children with SB, cognitive screening and support are currently part of SB follow-up in many well-resourced countries. The guidelines for the care of adults
with SB [27] recommend a full neuropsychological assessment for persons with cognitive problems. However, our study showed that cognitive problems are widespread and common. To enable
optimal individual support in coping with aspects of daily life, we suggest that global cognitive screening such as Montreal Cognitive assessment [28] is offered when persons with SB are
enrolled in adult care and at follow-up. For persons, whose screening results indicate the need for further investigation, we suggest that they are offered a full neuropsychological
assessment, including assessment of psychomotor speed and executive function. In this study, almost two thirds of the participants (63%) had hydrocephalus which can be a major determinant
for cognitive function [2, 4, 7] depending on severity. However, no information could be found in the medical records about the severity of the hydrocephalus, only information about whether
hydrocephalus was present or not. Hydrocephalus is a rough measure that offers minimal information about the impact on cognitive or physical function i.e., the consequences for everyday
life. This means that a person with well-functioning hydrocephalus can be very different from a person with multiple complications and who has received multiple operations. Thus, we have
chosen not to focus on hydrocephalus in the manuscript. Almost half of the cohort (46%) had scoliosis. This is in line with a review by Heyns et al. [23] in which just over 50% of the study
cohort had scoliosis. More than nine out of ten participants with MF level 5, all wheelchair users, had scoliosis. According to clinical experience, scoliosis may negatively affect the
sitting posture in a wheelchair making it difficult to achieve an ergonomically sound position. We explored factors associated with ambulation in participants with MF level 3. In this
cohort, the ambulatory function was highly variable despite similar muscular prerequisites suggesting that other factors are important in predicting the level of ambulation. The ambulators
had better prerequisites for walking with a lower BMI, lower presence of scoliosis and better results from the coding test for psychomotor speed and executive function. Among these factors,
scoliosis and BMI had the highest impact. The association between scoliosis and ambulatory status has been previously indicated [29]. A high BMI is associated with a greater risk of
cardiovascular disease, pressure ulcers, decreased participation in physical activity, psychosocial consequences, and can negatively affect mobility and transfers [30]. As this was a
cross-sectional study, the causality dilemma of “which came first”—a higher BMI resulting from increased wheelchair use or a higher BMI being the reason for using a wheelchair more—could not
be answered. In this study, ambulatory persons demonstrated significantly higher coding test results, an easily administered and sensitive test of psychomotor capacity, that is relatively
unaffected by intellectual capacity, education or learning [31]. Further, the household ambulators, combining ambulation with wheelchair use for longer distances, were younger than both the
community ambulators and wheelchair users, potentially indicating a transition of mobility over time. The factors that potentially affect a changed mode of mobility would be interesting for
future studies. STRENGTHS AND LIMITATIONS This study comprises a large regional cohort of adults with SB, estimated to represent around 25% of the national cohort. The entire cohort was
invited to participate and more than 90% of the 219 adults who met the eligibility criteria agreed to participate. The cohort is assumed to represent more than 90% of adults with SB in the
Greater Stockholm area. This is due to the extensive system of follow-up and detection of new cases. We consider it a strength that the cohort represents adult persons with SB with a wide
age range (18–73 years), as well as mode of mobility and cognitive capacity. Patients did not receive standard radiographs as part of the data collection process, therefore there is a level
of uncertainty concerning the prevalence of scoliosis. However, as our numbers are in line with previous literature, we believe they are largely accurate. Of the participants, 21% declined
cognitive assessment, of which a few had previously performed similar tests. However, no obvious differences in characteristics (age, sex, prevalence of hydrocephalus, muscle, or ambulatory
function) could be detected between the participants who declined and those who performed the tests. Although the MF level 3 comprised a near-total regional cohort (_n_ = 58) it was a
relatively small group, hence the current results should be interpreted with caution. Further, the participants were classified according to the MF levels of the most severely impaired side,
potentially resulting in some of the participants having better prerequisites for walking compared to those participants with a symmetric level of MF. CLINICAL IMPLICATIONS First, it is
important to focus on modifiable factors such as BMI, starting already in childhood. In a review in 2017 [32], Polfuss et al. concluded that it is “critical to initiate prevention efforts
early with a multifactorial approach for this at-risk population”. They might be offered nutrition and health-related lifestyle coaching and be provided with an easy way to measure and
follow-up their weight (this also applies to wheelchair users). Moreover, as almost half of this cohort reported no weekly exercise, it is important to locate gyms that are also suited to
physically impaired persons and/or provide a programme for home exercises. Even non-exercise physical activity has been reported to increase energy expenditure in persons with complete
paraplegia [33] highlighting the importance of an active lifestyle. Second, to include spinal assessment in standardised clinical care is of importance to be able to prevent and address
scoliosis. Third, adults with SB should be offered the opportunity to try out and modify orthoses and assistive devices as this could significantly improve gait pattern, and thereby help
maintain ambulatory function and a higher level of physical activity. The association between ambulation and cognitive function might suggest that people with SB have difficulties performing
dual tasking, i.e., a cognitive and a motor task simultaneously. Difficulties in performing dual tasks or prioritising the most important tasks may have serious consequences in everyday
life, with an increased risk of falls and consequential injuries. Falls are common in persons with Spinal Cord Injuries [34], who have similar prerequisites for ambulation as persons with
SB. However, thus far, dual-task interference in adults with SB is an unexplored field. Further research is essential to identify the best intervention for this group. CONCLUSION Cognitive
capacity and mode of mobility varied widely across the cohort and the latter differed between persons with similar muscle function. In participants with MF level 3, factors independently
associated with ambulation included the absence of scoliosis, lower BMI, and better results on the coding test for psychomotor speed and executive function. It is important to prevent
scoliosis when possible, support a healthy lifestyle, as well as offer cognitive screening and support to promote ambulatory function and optimise independence in the everyday lives of
adults with SB. DATA ARCHIVING Due to Swedish and EU personal data legislation, the dataset is not publicly available but is available from the corresponding author upon appropriate request.
Any sharing of data will be regulated via a data transfer and user agreement with the recipient. REFERENCES * Wagner R, Linroth R, Gangl C, Mitchell N, Hall M, Cady R, et al. Perception of
secondary conditions in adults with spina bifida and impact on daily life. Disabil Health J. 2015;8:492–8. Article Google Scholar * Copp AJ, Adzick NS, Chitty LS, Fletcher JM, Holmbeck GN,
Shaw GM. Spina bifida. Nat Rev Dis Prim. 2015;1:1–18. Google Scholar * Bowman RM, McLone DG, Grant JA, Tomita T, Ito JA. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg.
2001;34:114–20. Article CAS Google Scholar * Liptak GS, Garver K, Dosa NP. Spina bifida grown up. J Dev Behav Pediatr. 2013;34:206–15. Article Google Scholar * Fletcher JM, Copeland K,
Frederick JA, Blaser SE, Kramer LA, Northrup H, et al. Spinal lesion level in spina bifida: a source of neural and cognitive heterogeneity. J Neurosurg. 2005;102:268–79. PubMed Google
Scholar * Dennis M, Barnes MA. The cognitive phenotype of spina bifida meningomyelocele. Dev Disabilities Res Rev. 2010;16:31–9. Article Google Scholar * Del Bigio MR. Neuropathology and
structural changes in hydrocephalus. Dev Disabilities Res Rev. 2010;16:16–22. * Miller E, Widjaja E, Blaser S, Dennis M, Raybaud C. The old and the new: supratentorial MR findings in Chiari
II malformation. Child’s Nervous Syst. 2008;24:563–75. Article Google Scholar * Bartonek A, Saraste H. Factors influencing ambulation in myelomeningocele: a cross-sectional study. Dev Med
Child Neurol. 2001;43:253–60. Article CAS Google Scholar * Gutierrez EM, Bartonek A, Haglund-Akerlind Y, Saraste H. Kinetics of compensatory gait in persons with myelomeningocele. Gait
Posture. 2005;21:12–23. Article Google Scholar * Bendt M, Bartonek Å. Walking in adults with spina bifida with respect to muscle function. Eur J Physiother. 2016;18:154–60. Article Google
Scholar * Thompson RM, Foley J, Dias L, Swaroop VT. Hip status and long-term functional outcomes in spina bifida. J Pediatr Orthopaedics. 2019;39:e168–e72. Article Google Scholar *
Takakusaki K. Neurophysiology of gait: from the spinal cord to the frontal lobe. Mov Disord. 2013;28:1483–91. Article Google Scholar * Tita AC, Frampton JR, Roehmer C, Izzo SE, Houtrow AJ,
Dicianno BE. Correlation between neurologic impairment grade and ambulation status in the adult spina bifida population. Am J Phys Med Rehabilitation. 2019;98:1045–50. Article Google
Scholar * Bartonek A, Saraste H, Knutson LM. Comparison of different systems to classify the neurological level of lesion in patients with myelomeningocele. Dev Med Child Neurol.
1999;41:796–805. Article CAS Google Scholar * Seitzberg A, Lind M, Biering-Sorensen F. Ambulation in adults with myelomeningocele. Is it possible to predict the level of ambulation in
early life? Child’s Nervous Syst. 2008;24:231–7. Article Google Scholar * Bendt M, Gabrielsson H, Riedel D, Hagman G, Hultling C, Franzen E, et al. Adults with spina bifida: a
cross-sectional study of health issues and living conditions. Brain Behav. 2020;10:e01736. Article Google Scholar * Hislop HJ. Daniel´s and Worthingham´s muscle testing. Techniques of
manual examination. Philadelphia, PA: Saunders Company; 1995. * Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A, et al. International standards for neurological
classification of spinal cord injury (revised 2011). J Spinal Cord Med. 2011;34:535–46. Article Google Scholar * Hoffer MM, Feiwell E, Perry R, Perry J, Bonnett C. Functional ambulation in
patients with myelomeningocele. J bone Jt Surg Am Vol. 1973;55:137–48. Article CAS Google Scholar * Wechsler D. WAIS-III/WMSIII technical manual: Updated. San Antonio: Psychological
Corporation; 2002. * Tallberg IM, Ivachova E, Jones Tinghag K, Ostberg P. Swedish norms for word fluency tests: FAS, animals and verbs. Scand J Psychol. 2008;49:479–85.
https://doi.org/10.1111/j.1467-9450.2008.00653.x. * Heyns A, Negrini S, Jansen K, Moens P, Schelfaut S, Peers K, et al. The prevalence of scoliosis in spina bifida subpopulations: a
systematic review. Am J Phys Med Rehabilitation. 2018;97:848–54. Article Google Scholar * Vittinghoff E, McCulloch CE. Relaxing the rule of ten events per variable in logistic and Cox
regression. Am J Epidemiol. 2007;165:710–8. Article Google Scholar * Chaves ES, Boninger ML, Cooper R, Fitzgerald SG, Gray DB, Cooper RA. Assessing the influence of wheelchair technology
on perception of participation in spinal cord injury. Arch Phys Med Rehabilitation. 2004;85:1854–8. Article Google Scholar * Gabrielsson H, Hultling C, Cronqvist A, Asaba E. Views on
everyday life among adults with spina bifida: an exploration through photovoice. Int J Qual Stud Health Well-being. 2020;15:1830702. Article Google Scholar * Guidelines for the care of
people with Spina Bifida. available from https://www.spinabifidaassociation.org/: Spina Bifida Association; 2020 [cited 2019 0407]. * Nasreddine ZS, Phillips NA, Bedirian V, Charbonneau S,
Whitehead V, Collin I, et al. The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatrics Soc. 2005;53:695–9. Article Google Scholar *
Müller EB, Nordwall A, Odén A. Progression of scoliosis in children with myelomeningocele. Spine. 1994;19:147–50. Article Google Scholar * Agha M, Agha R. The rising prevalence of obesity:
part A: impact on public health. Int J Surg Oncol. 2017;2:e17. Article Google Scholar * Hoyer WJ, Stawski RS, Wasylyshyn C, Verhaeghen P. Adult age and digit symbol substitution
performance: a meta-analysis. Psychol Aging. 2004;19:211–4. Article Google Scholar * Polfuss M, Bandini LG, Sawin KJ. Obesity prevention for individuals with spina bifida. Curr Obes Rep.
2017;6:116–26. Article Google Scholar * Holmlund T, Ekblom-Bak E, Franzén E, Hultling C, Wikmar LN, Wahman K. Energy expenditure in people with motor-complete paraplegia. Spinal Cord.
2017;55:774–81. Article CAS Google Scholar * Jørgensen V, Butler Forslund E, Opheim A, Franzén E, Wahman K, Hultling C, et al. Falls and fear of falling predict future falls and related
injuries in ambulatory individuals with spinal cord injury: a longitudinal observational study. J Physiother. 2017;63:108–13. Article Google Scholar Download references ACKNOWLEDGEMENTS We
would like to thank the study participants for taking part in this study. We would also like to thank OT, MSc Dorothy Riedel, RN Gabriella Innerstedt and RN PhD Hanna Gabrielsson for their
valuable contributions during the data collection and Lena Lindbo (Operational manager at the Spinalis Outpatient Clinic), Aleris Rehab Station and Karolinska Institutet for their support.
AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Aleris Rehab Station, Spinalis Outpatient Clinic, Solna, Sweden Martina Bendt, Åke Seiger & Emelie Butler Forslund * Department of
Neurobiology, Care Science and Society, Karolinska Institutet, Stockholm, Sweden Martina Bendt, Åke Seiger, Göran Hagman, Claes Hultling, Erika Franzén & Emelie Butler Forslund *
Spinalis, Foundation, Stockholm, Sweden Claes Hultling * Sophiahemmet, University College, Stockholm, Sweden Claes Hultling * Allied Health Professionals, Medical Unit Occupational Therapy
and Physical Therapy, Karolinska University Hospital, Stockholm, Sweden Erika Franzén * Stockholms Sjukhem R & D Unit, Stockholm, Sweden Erika Franzén Authors * Martina Bendt View author
publications You can also search for this author inPubMed Google Scholar * Åke Seiger View author publications You can also search for this author inPubMed Google Scholar * Göran Hagman
View author publications You can also search for this author inPubMed Google Scholar * Claes Hultling View author publications You can also search for this author inPubMed Google Scholar *
Erika Franzén View author publications You can also search for this author inPubMed Google Scholar * Emelie Butler Forslund View author publications You can also search for this author
inPubMed Google Scholar CONTRIBUTIONS MB, EBF, EF and ÅS designed the study. Authors MB, EBF and GH conducted the data analysis, while all authors (ÅS, EF, CH) contributed to the
interpretation of the data. MB drafted the manuscript. All authors revised the manuscript for important intellectual content and approved the final version. CORRESPONDING AUTHOR
Correspondence to Martina Bendt. ETHICS DECLARATIONS FUNDING The contents of this publication were developed with grants from the Caroline Montgomery Foundation, the Spinalis Foundation, the
Promobilia Foundation, and support from the Aleris Rehab Station. ETHICS We certify that all applicable institutional and governmental regulations concerning the ethical use of human
volunteers were followed during the course of this research. Verbal and written information was provided before the participants gave their written informed consent. The study was approved
by the Regional Ethical Review Board in Stockholm (Dnr: 2014/1111-31). COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature
remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE
Bendt, M., Seiger, Å., Hagman, G. _et al._ Adults with spina bifida: ambulatory performance and cognitive capacity in relation to muscle function. _Spinal Cord_ 60, 122–128 (2022).
https://doi.org/10.1038/s41393-021-00658-w Download citation * Received: 13 November 2020 * Revised: 10 June 2021 * Accepted: 11 June 2021 * Published: 14 July 2021 * Issue Date: February
2022 * DOI: https://doi.org/10.1038/s41393-021-00658-w SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable
link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative