Play all audios:
ABSTRACT OBJECTIVES To assess the appropriateness of oral surgery referrals, after triage, to intermediate minor oral surgery (IMOS) practices in East Kent and whether or not referrals vary
according to the referring general dental practitioner's (GDP's) place of qualification and experience. DESIGN A retrospective study of the records of 441 triaged referrals sent to
three IMOS practices in East Kent, over a ten-week period. An assessment tool was developed in line with local and national referral guidelines. Information on all referrals was obtained
from the IMOS provider and referral records. Descriptive analysis of the data was performed. RESULTS The most common reason for referral was for extraction of teeth requiring bone removal (n
= 155; 35%). However, the majority of teeth removed were recorded as a non-surgical extraction (n = 363; 82%). Medical histories were included appropriately in the referral communications,
with only 0.2% of all referrals being inappropriate. The proportion of appropriate and inappropriate referrals was very similar and it was found that referral rate was lower from dentists
who had been qualified for more than ten years. GDPs working in the same location as the IMOS provider made a greater total number of referrals as well as more inappropriate referrals.
CONCLUSIONS In the group of GDPs and IMOS providers studied, a wide variation was observed between the GDP's reason for referral and the treatment provided. It may be concluded that the
vast majority of extractions were safely completed in an IMOS dental practice in a primary care setting. You have full access to this article via your institution. Download PDF SIMILAR
CONTENT BEING VIEWED BY OTHERS INVESTIGATING THE APPROPRIATENESS OF SURGICAL ENDODONTIC REFERRALS TO A WEST SUSSEX REGIONAL REFERRAL UNIT Article 24 February 2021 AN EVALUATION OF ORAL
SURGERY REFERRALS TO AID DEVELOPMENT OF AN INTEGRATED SERVICE IN SOUTH WEST ENGLAND Article 21 October 2024 THE VALUE OF A REMOTE ORTHODONTIC ASSESSMENT FOR CHILDREN HAVING PERMANENT TEETH
EXTRACTED UNDER GENERAL ANAESTHESIA Article 01 May 2024 KEY POINTS * Discusses the efficacy of treating simpler minor oral surgery cases within primary care. * Highlights that general dental
practitioner experience does not necessarily lead to a decrease in inappropriate referrals. * Suggests clinicians continue developing oral surgery skills in order to prevent unnecessary
referrals. INTRODUCTION Patients who require treatment deemed to be outside the scope of a general dental practitioner's (GDP's) skills might require their care to be provided by a
dentist with greater capability in that area. Traditionally, in the UK, this has been provided in secondary care. However, it is becoming increasingly common to provide much of this
treatment in the primary care setting by either specialists or general dentists with enhanced skills. A substantial proportion of referrals made to hospital-based specialists have included
dento-alveolar surgery.1 This less complex work increases hospital waiting lists and raises questions regarding cost-effectiveness.2 The Dental Programme Board published a review which
recommended that more oral surgery should take place in primary care, to increase the availability of secondary care for more complex cases.1 Studies have also demonstrated the safety and
efficacy of treating patients for dento-alveolar surgery within a primary care setting.3,4 Intermediate minor oral surgery (IMOS) services have been commissioned in Kent to receive routine
oral surgery referrals, in order to reduce the numbers of referrals to hospital oral and maxillofacial surgery (OMFS) departments and provide prompter local care for patients. After a poor
initial uptake of IMOS services, there has been much expansion. NHS England has produced a guide for commissioning oral surgery and oral medicine, which has further prompted contractual
changes.5 In Croydon, the introduction of a primary care IMOS service saw an overall increase in numbers of referrals, which was fully absorbed by primary care practices.6 Referrals for
dento-alveolar surgery are most commonly made due to the perceived difficulty of surgery, medical history complications and a request for sedation or general anaesthesia.2 It has also been
suggested that a lack of experience and equipment are also contributory reasons.7 Prior to the introduction of IMOS, one study found that a large proportion of dentists were dissatisfied
with the service offered by their specialist oral surgery provider. The most commonly cited reason for this was the length of waiting lists.8 Patients have also expressed dissatisfaction
with the referral system, with one fifth of GDPs reporting their patients showing some reluctance to be referred away from the practice.2 Furthermore, it has been suggested that patient
satisfaction is high when oral surgical procedures are provided in a primary care environment.2,8 Referrals are the main and usually the only source of communication between the referrer and
the specialist practitioner. Deficiencies in the information provided may compromise effective triaging and, consequently, patient management.9 It has been shown that the content of
referral letters for oral surgery is often inadequate and that the treating clinician does not receive all the required information.10 Referral guidelines are commonly utilised in an attempt
to reduce inappropriate referrals. They may be introduced with or without associated training.11 Referral to the IMOS system in Kent initially used a hand written proforma. In 2015, Vantage
Health was commissioned to provide a dental electronic referral system (DERS) named 'REGO' which replaced the initial paper-based system. This electronic system is compatible with
most dental software systems and has a built in proforma. Since the introduction of DERS, referrals are no longer triaged manually. Instead, electronic algorithms triage referrals
automatically into their complexities as advised by the national commissioning document.5 This may allow for some error, as extra clinical detail may not be perceived by a computer-based
triage system. However, the advantages of DERS are instant triaging and shorter waiting times. Patients are then contacted and offered an appointment for treatment with a specialist oral
surgeon at the chosen provider practice in Kent. Health care overuse is a common problem faced by health systems in developed countries across the world and has been discussed extensively in
medical literature.12 There is evidence to suggest that dentists are referring cases which they may have previously treated themselves. This may be due to the feeling of decreased
competence which interestingly has not been shown to be affected by experience.13 Contributory factors to over-referral may include fear of litigation, the time and effort required in
detailing the risks of the procedure, and financial interests.12 OBJECTIVES Against this background, the aims of the current study were to determine the appropriateness of oral surgery
referrals made to three contracted IMOS practices in East Kent by various GDPs during the period from May 2017 to July 2017, and to assess whether or not referrals varied according to the
referring GDP's place of qualification and experience. METHODS A data collection tool was designed and piloted. The criteria for the collection of data are shown in Table 1. They follow
the referral criteria for the Kent and Medway IMOS service and record reasons given for referral, as well as treatment undertaken and whether it would be regarded as appropriate to the
referral.14 Data were collected by a clinician (AP) from clinical and IMOS referral records for all patients who underwent oral surgical procedures in the three practices located in Ashford,
Sittingbourne and Canterbury, over a period of ten weeks between May 2017 and July 2017. This sample provided a total of 95 referring GDPs and 441 consecutive cases. For each referral, the
GDP's referral and IMOS provider clinical records were interpreted and assessed retrospectively by one clinician (AP). The sample did not include patients who failed to attend their
treatment appointment post-referral, or patients for whom the referral record was unobtainable from the archives. Data from each case were recorded manually on a proforma. Later, these were
transferred into a Microsoft Excel database. The study was approved by the Research Ethics Advisory Group of the Centre for Professional Practice (CPP), University of Kent. RESULTS GDP
DEMOGRAPHICS The mean post-qualification experience of referring GDPs was 13 years (range 1-40 years). The largest groups of referring GDPs had 6-10 and 11-15 years post qualification
experience. The majority of GDPs (69; 72%) referred between zero and five patients in the ten-week period. On average, each GDP made five referrals in the ten-week period (Table 2). REASONS
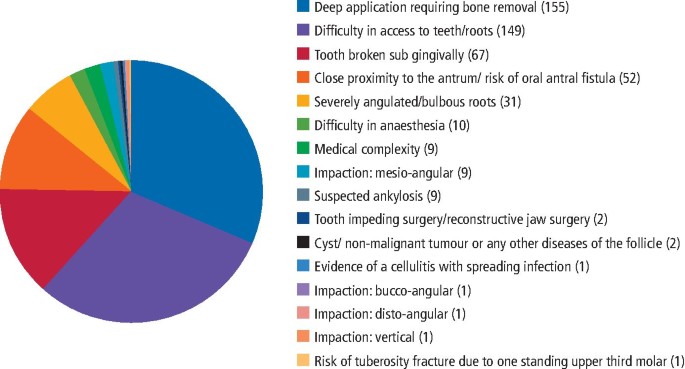
FOR MAKING AN ORAL SURGERY REFERRAL GDPs are able to choose reasons from 22 options in the referral computer program (Fig. 1). They may select one or more reasons for referral, and all
reasons provided are recorded. The commonest two reasons for referral were the requirement for bone removal and difficulty in access to teeth (Table 3). At the time of this study the options
did not include the proximity of the inferior dental nerve in relation to lower third molars as a possible reason for referral. Since then, the REGO referral program has been modified to
include this. REPORTING OF MEDICAL HISTORY Nine (2%) referrals received by the IMOS providers were made with at least one reason being a perceived complex medical history. Two of these nine
referrals did not have a truly complex medical history (0.2%). ORAL SURGICAL PROCEDURES UNDERTAKEN The majority of patients had a simple forceps extraction (n = 363; 82%) which, in some
cases, included the use of elevators and luxators but without any bone removal. A minority of cases necessitated a surgical extraction requiring bone removal (n = 25; 6%). A relative
minority of the procedures (18; 4%) were third molar extractions. They were performed in accordance with the Kent and Medway Area Team guidelines.15 Full details of treatments provided by
the IMOS service are presented in Table 4 and Figure 2. The most common reason for no treatment was the patient declining extraction (10; 2%), closely followed by the conservative management
of wisdom teeth (7; 2%) as detailed in the National Institute for Health and Care Excellence (NICE) guidelines.16 One patient was not treated on the grounds that they were unaware of the
reason for or nature of the referral. Four cases (1%) experienced post-operative complications. These were as follows: * Creation of an OAC (2) * Osteomyelitis (1) * Incidental finding on
radiograph leading to an urgent referral for suspected cancer (1). The four cases (1%) received treatment other than the dental extractions for which they had been referred. These treatments
were: * Coronectomy (1) * Operculectomy (2) * Extraction of an opposing upper third molar, rather than the lower third molar, which had been the original reason for the referral (1).
COUNTRY OF QUALIFICATION OF THE REFERRING GDP The number of appropriate referrals totalled 209, with 232 being inappropriate, leading to an approximate ratio of 1:1.1. The number of GDPs
qualifying in the UK totalled 35, with 60 qualifying abroad. GDPs qualifying in the UK made 171 referrals and those qualifying abroad made 270. Of all the UK qualifying GDP referrals, 78
(46%) were deemed as appropriate. A similar pattern was found with the non-UK referrers, as 131 (49%) were deemed to be appropriate (Table 5). EXPERIENCE OF THE REFERRING GDP Most referrals
were made by GDPs who had been qualified for 20 years or less. (Table 6). The greatest number of inappropriate referrals were made by GDPs within six and 10 years of qualification. However,
as a proportion, newly-qualified GDPs within five years of qualification made most inappropriate referrals. Although the referral rate reduced after 10 years of experience, the ratio of
inappropriate to appropriate referrals remained the same. REFERRING GDPS PRACTISING IN THE SAME LOCATION AS AN IMOS PROVIDER Thirteen referring GDPs practised in the same practice as the
IMOS provider. In total, GDPs working in the same practice as the IMOS provider made 147 referrals (33%), and GDPs from other practices 294 (67%). GDPs working at the same location as the
IMOS provider made on average 11 referrals per GDP whereas GDPs working in a different location made four (Table 7). GDPs working in the same practice as the IMOS provider also made a larger
number of inappropriate referrals, averaging seven inappropriate referrals per GDP, whereas for GDPs working at a different practice it was two per GDP. DISCUSSION Not all teeth that were
referred for bone removal were considered to require this by the IMOS providers. Although 155 referrals were sent with at least one reason being the need for bone removal, 363 (82%) of
patients received a non-surgical extraction involving the use of forceps, with or without the use of an elevator. Only 25 patients required a surgical extraction including bone removal.
Thus, when judged by this acceptance criteria, 130 referrals can be viewed as inappropriate. However, GDP assessment of a surgical extraction may be different to that of an IMOS provider.
For instance, a GDP may consider tooth sectioning to be categorised as a surgical procedure, and there is no distinction on the referral proforma to distinguish this. Also, none of the IMOS
providers made any comments about the difficulty of extractions in the clinical records. IMOS providers also have enhanced oral surgery skills compared to the average GDP and what may be
recorded as a seemingly 'simple forceps extraction' by an IMOS provider could be difficult for the average GDP. Perceived difficulty was impossible to quantify in the current
investigation. However, this finding suggests a gap in the skill-set of many of the GDPs whose referrals were assessed in the current study. GDPs may be referring cases due to a lack of
equipment as they may work in a practice where they do not have easy access to equipment for surgical exodontia, resulting in them not taking the risk of an extraction becoming surgical,
thus leading them to refer simpler cases. A counter argument is that it would be reasonable to expect this equipment to be present in a dental practice and if it is not present then perhaps
the local dental network (LDN) might be interested in investigating the relevant practices. One patient was not treated because they were unaware of the reason for their referral. For
dentists to be able to refer any patient, they must legally seek the patient's consent. This highlights wider issues in communication between a GDP and their patients. The very low
proportion of cases referred onward to secondary care (2%) from the IMOS practices suggests an effective triaging system. Furthermore, the cases which were referred to the local OMFS
department were not being sent back to the IMOS service, suggesting that the consultants concerned agreed with the need for the tertiary referrals. One case that was referred for a suspicion
of malignancy by the IMOS provider was due to an incidental finding on a radiograph which was not reported on the referral form by the GDP concerned. This may be a reflection of a lack of
insight from the referring GDP which could have had serious consequences. Only one case was not treated due to the absence of an appropriate radiograph. Although it was reassuring, it was an
unexpectedly low number in comparison with one previous study which found that 93% of referrals failed to include an appropriate radiograph.17 The very low number was almost certainly due
to the DERS computer algorithm used in Kent, which does not allow a referral to be sent in absence of a radiograph. Nevertheless, the records gave no indication of the quality of the
radiographs or of how many extractions were completed, despite the lack of an optimal radiograph. The one case where no extraction was completed highlighted a serious issue as it was not
possible to evaluate the difficulty of an extraction without a radiograph of the root. This raises questions regarding the degree of assessment as well as radiographic examination by the
referring GDP. It becomes evident that reasons such as poor assessment and inaccuracy in referral communications could be a reason for the high proportion of cases perceived as simple by the
IMOS providers. Data were collected in December 2017, five months after the last IMOS treatment episode. This allowed for a reasonable length of time during which post-operative
complications could have arisen. Less than 1% of patients had a recorded post-operative complication. This is the same proportion as reported for the IMOS service in Croydon.18 However, a
previous study found a higher incidence of post-operative complications.19 Investigations into extractions undertaken in hospital have shown an even higher incidence. This may be explained
by referrals to hospital being more complex and perhaps presenting at a later stage in the disease process.20 Although the 1% incidence of post-operative complications is reassuring, it may
be a reflection of underreporting. No patients reported to the IMOS service with alveolar osteitis (AO). This is surprising, as dry socket rates have been reported as on average around 5%
and even up to 30% for wisdom teeth.20,21 In Kent, patients are advised to contact their own GDP if complications arise, and referring GDPs are responsible for the management of these
post-operative complications. Therefore, patients are likely to have visited their own GDP which would not have been recorded by the IMOS providers. Furthermore, no record was made of
telephone advice given to patients regarding relatively common post-operative complications such as pain, haemorrhage and infections. Cases where no OAC was created by the IMOS provider were
regarded as inappropriately referred, if this was the only reason given for referral. However, it would unfair to blame the GDP for this, as even oral surgeons can be unsure as to the
proximity of the sinus to the roots of upper posterior teeth, solely from an intraoral radiograph. The radiographs were not assessed by the IMOS providers in their clinical records. Thus
this may be reflected in an under-recording of appropriateness. In addition, IMOS providers have enhanced skills which may contribute to the lower incidence of an OAC compared to that
occurring if a GDP undertook the surgery. The UK has an ageing population with increased medical morbidities. The primary care service should be equipped to address this problem. It is
reassuring that only 0.4% of referrals were inappropriate on the grounds of medical history. However, this appears to be an unexpectedly low figure as other investigations have shown this to
be as high as 40%.22 Moreover, the current study did not look at underreporting of medical history conditions. The results showed that the greatest proportion of inappropriate referrals
were made by newly-qualified (between one and five years) GDPs. These newly qualified GDPs would be expected to have the most up to date knowledge. However, with the advent of widespread
fluoride use, better oral hygiene measures, combined with a shift towards retaining teeth rather than extraction, the number of oral surgery procedures a newly qualifying GDP undertakes
before and post-qualification can be small, thus impacting on their confidence.23 Although marked as inappropriate, these younger GDPs may be anticipating difficulty due to a lack of
experience. It would be interesting to review this cohort in a decade to see whether this trend continues in this particular cohort. In addition, it may also be that younger GDPs are
experiencing pressure to refer. Variation in referral rates may also be attributed to practice location.24 One of the practices in the study was one of very few NHS practices in a city with
two universities. This may explain an increased number of referrals for third molar surgery compared to other practices, such as those in a rural location. A future study with a larger
sample population could investigate whether this would be of significance. GDPs who were 36-40 years post-qualification made no inappropriate referrals. This may be explained by increased
experience and confidence with various oral surgical procedures, alongside complication management.25 It should also be noted that only four of the 95 GDPs were in this age bracket. If only
half of the referrals are appropriate, this may be a reflection of deficiency in the capability of GDPs, or may be due to non-clinical behavioural factors such as dento-legal issues.26 Other
reasons for a GDP to prefer not to manage a patient in primary care can include personality, relationships and patient communication.27 However, there may also be an under-estimation of
referral appropriateness. It was interesting to see that, in the current study, UK qualification did not have a significant impact on referral behaviour. A previous study3 found that
patients were reluctant to be referred out of their local practice for oral surgical procedures with geographical distance from a hospital being a barrier to referral. This investigation has
shown that GDPs working in the same practice as the IMOS provider made a greater number of referrals, as well as a greater proportion of inappropriate referrals. This finding may be related
to the non-clinical factors that have been discussed in previous sections. The current study only focused on GDP referrals to the IMOS service. It should be remembered that the skill-set of
each GDP was variable, hence those making high levels of referrals may not be making truly inappropriate referrals and wasting specialist services. It should also be noted that this
investigation has not measured the quality of care provided for patients and therefore caution must be applied when interpreting the results. It would be interesting to see if the referral
pattern over the ten-week period in East Kent, reported in this paper, was typical of that in the rest of the country. If it is then a number of questions about younger dentists'
ability and/or inclination to manage simple extractions and some minor oral surgery are raised. CONCLUSIONS In the group of GDPs and IMOS providers studied, a wide variation was observed
between the GDP's reason for referral compared to the treatment provided. The proportion of appropriate and inappropriate referrals was very similar and it was found that referral rate
reduced from dentists who had been qualified for more than ten years. UK and non-UK qualified dentists made the same proportion of inappropriate referrals. GDPs working in the same location
as the IMOS provider made a greater total number of referrals as well as more inappropriate referrals. In an attempt to reduce the number of inappropriate referrals, the authors suggest that
local oral surgery managed clinical networks contact GDPs inviting them for discussions. This would also allow referring GDPs to air any concerns or queries. Another possibility could be to
contact referring GDPs with IMOS statistics and ways of reducing inappropriate referrals. Medical histories were generally reported appropriately using the Kent and Medway area team
guidelines.16 Due to the mandatory attachment of radiographs to the online referral form, 99.7% of referrals were accompanied by a radiograph appropriate for the procedure. REFERENCES *
Medical Education England. Review of oral surgery services and training. 2011. Available at https://www.baos.org.uk/resources/MEEOSreview.pdf (accessed July 2019). * Coulthard P, Kazakou I,
Koron R, Worthington H V. Referral patterns and the referral system for oral surgery care. Part 1: General Dental Practitioner referral patterns._ Br Dent J_ 2000; 188: 142-145. * Coulthard
P, Bailey E, Bridgman C M. Introducing clinical triage for oral surgery referral management in England. _Oral Surg_ 2014; 7: 143-151. * Dyer T A. A five-year evaluation of an NHS dental
practicebased minor oral surgery service. _Community Dent Health_ 2013; 30: 219-226. * NHS England. Guide for Commissioning Specialist Dentistry Services. 2015. Available at
https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/09/introguidecommsdentspecl.pdf (accessed July 2019). * Kendall N. Improving access to oral surgery services in
primary care_._ _Prim Dent Care_ 2009; 16: 137-142. * Hashemipour M S, Mansouri M. Investigation of cases and referral patterns of patients to dental specialists by general dentists in 2011
in Kerman, Iran. _Journal of Isfahan Dent School_ 2012; 8: 433-443. * Clark S. Professional attitudes to specialisation and minor oral surgery in general dental practice. _Br Dent J_ 1995;
179: 209-213. * Webb J B, Khanna A. Can we rely on a general dental practitioner's referral letter to a skin lesion clinic to prioritize appointments and does it make a difference to
the patients prognosis? _Ann R Coll Surg Eng_ 2006; 88: 40-45. * Moloney J, Stassen L F. An audit of the quality of referral letters received by the Department of Oral and Maxillofacial
Surgery, Dublin Dental School and Hospital. _J Ir Dent Assoc_ 2010; 56: 221-223. * Dowie R. A review of research in the United Kingdom to evaluate the implementation of clinical guidelines
in general practice. _Fam Pract_ 1998; 15: 462-470. * Brownlee S, Chalkidou K, Doust J _et al._ Evidence for the overuse of medical services around the world. _Lancet_ 2017; 390: 156-168. *
Davies B J, Macfarlane F. Clinical decision making by dentists working in the NHS General Dental Services since April 2006. _Br Dent J_ 2010; 209: E17. * Powell A A, Bloomfield H E, Burgess
D J, Wilt T J, Partin M R. A conceptual framework for understanding and reducing overuse by primary care providers. _Med Care Res Rev_ 2013; 70: 451-472. * Public Health England, KSS Centre
for NHS England, Kent and Medway Area Team. Dental Referee: A guide for dental teams in Kent and Medway. 2015. * National Institute for Health and Care Excellence. Guidance on the Extraction
of Wisdom Teeth. 2000. Available at https://www.nice.org.uk/guidance/ta1 (accessed July 2019). * Shaffie N, Cheng L. Improving the quality of oral surgery referrals. _Br Dent J_ 2012; 213:
411-413. * O' Neill E, Gallagher J E, Kendall N. A Baseline Audit of Referral and Treatment Delivered to Patients in the Intermediate Minor Oral Surgery Service in Croydon PCT. _Prim
Dent Care_ 2012; 19: 21-28. * Bell G. An audit of 600 referrals to a primary care based oral surgery service_. Br Dent J_ 2007; 203: E6. * Venkateshwar G P, Padhye M N, Khosla A R, Kakkar S
T. Complications of exodontia: a retrospective study. _Indian J Dent Res_ 2011; 22: 633-638. * Akinbami B O, Godspower T. Dry Socket: Incidence, Clinical Features, and Predisposing Factors.
_Int Dent J_ 2014; 796102. * Björkeborn, M, Nilsson H, Anderud J. Quality of oral surgery referrals and how to improve them. _Clin Cosmet Investig Dent_ 2017; 9: 111-116. * NHS Digital. NHS
Dental Statistics for England 2015-2016. 2016. Available at https://digital.nhs.uk/dataandinformation/publications/statistical/nhsdentalstatistics/nhsdentalstatisticsforengland201516
(accessed July 2019). * Linden G J. Variation in periodontal referral by general dental practitioners. _J Clin Periodontol_ 1998; 25: 655-661. * Cottrell D A, Reebye U N Blyer S M, Hunter M
J, Mehta N_._ Referral Patterns of General Dental Practitioners for Oral Surgical Procedures. _J Oral Maxillofac Surg_ 2007; 65: 686-690. * Youngson C C. Referral rates to specialists from
general practice. _Br Dent J_ 2005; 199: 153. * Broome J L. Main Non-Clinical Factors Influencing Endodontic Referral. _Prim Dent J_ 2016; 5: 64-68. Download references ACKNOWLEDGEMENTS The
authors would like to thank the IMOS providers for allowing access to the referral communications and records. The study was self-funded. Contribution of authors Anika Patel designed the
study, collected the data and drafted the paper. Sami Stagnell contributed to the study design, supervised it and checked all drafts of the paper. Kenneth Eaton advised on the design and
data collection and edited all drafts of the paper. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * General Dental Practitioner, Kent and Centre for Professional Practice, University of Kent,
Medway Campus, Kent, UK Anika Patel * Specialist Oral Surgeon Intermediate Minor Oral Surgery, Wessex. Smilekind, 30 Ashley Road, Boscombe, UK Sami Stagnell * Honorary Professor, Centre for
Professional Practice, University of Kent, Medway Campus, Kent, ME4 4AG and Visiting Professor, University College London, London, UK Kenneth Eaton Authors * Anika Patel View author
publications You can also search for this author inPubMed Google Scholar * Sami Stagnell View author publications You can also search for this author inPubMed Google Scholar * Kenneth Eaton
View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Anika Patel. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT
THIS ARTICLE CITE THIS ARTICLE Patel, A., Stagnell, S. & Eaton, K. The appropriateness of oral surgery referrals and treatment in contracted intermediate minor oral surgery practices in
East Kent. _Br Dent J_ 227, 211–216 (2019). https://doi.org/10.1038/s41415-019-0574-2 Download citation * Published: 09 August 2019 * Issue Date: August 2019 * DOI:
https://doi.org/10.1038/s41415-019-0574-2 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative