Play all audios:
Visual acuity (VA), the cornerstone of eyecare, can yield symptoms despite 20/20 [1]. Optimal VA is 20/10 based on cone spacing. Vernier acuity (minimum misalignment) is 3” arc, 10x <
cone spacing, a _hyperacuity_ mediated by visual cortex [2,3,4]. Minimum visible acuity [2] (MVA, thinnest black line detectable on white background) is 1” arc. Hence MVA (pilot avoiding
fine wire), is a potential hyperacuity never used clinically. We describe a cone specific test of MVA, including monocular, binocular, chromatic, and orientation specific performance.
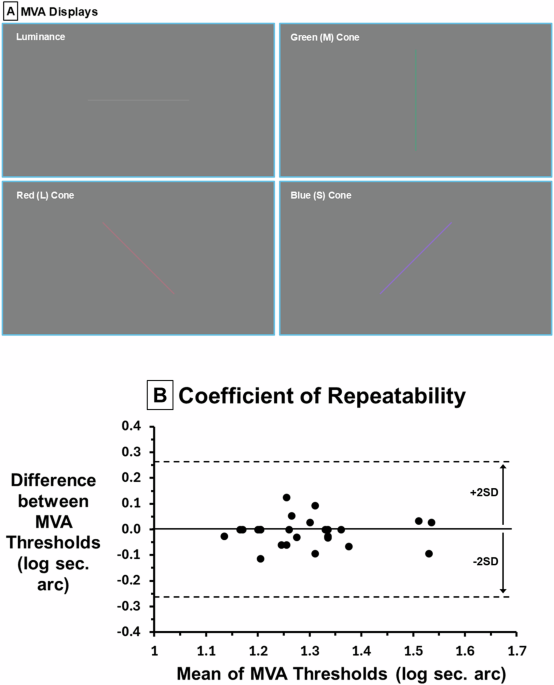
Twenty-five healthy young adults (VA ≥ 20/30, mean age ± SD: 26 ± 3, 13 females) participated in our IRB approved protocol after written informed consent. MVA stimuli were 1.4° vertical,
horizontal, or oblique (45°, 135°) lines centered on a Microsoft Surface display (3.7° x 2.1°) at 4 m in a dark room. Each line was an increase in red (L), green (M), blue (S) cone or
luminance (grey) against a grey background (24.7 cd/m2, _x, y_ = 0.318, 0.355) limiting stimulation to each pathway based on chromaticity and luminance [5]. Contrasts 16%: L, M, luminance;
128%: S cones due to sparse distribution and lower CS [5]. Line thicknesses varied from 60” to 10” arc in 0.16 log steps (16 stimuli/thickness level, 4 orientations, 4 colors). Each trial
consisted of a single line centered on the display wherein subjects identified stimulus orientation and color (0.01 log units/trial, Fig. 1a). Contrast, orientation, eye tested were
randomized across trials. Binocular followed monocular to minimize learning. Monocular (_P_ > 0.18) and binocular (_P_ > 0.47) MVA log thresholds were distributed normally
(Jarque–Berra test). Repeated-measures ANOVA, paired t-tests (Bonferroni correction) and Bland-Altman were used for analyses. Repeated measures ANOVA across eye tested and cone type showed
significant effects of eye (F = 15.5, _P_ < 0.001) and cone type (F = 50.8, _P_ < 0.001). Since MVA was not different between right and left eyes (_P_ > 0.73) means were used for
monocular analyses. The coefficient of repeatability, 95% confidence interval (CI) for within-patient change, was 0.3 log thickness (2” arc, Bland Altman, Fig. 1b). Across all colors, mean
binocular threshold (1.12 log s, 13”) was significantly lower than monocular (1.30, 20”, mean difference 0.18 log s, 95% CI 0.16–0.20, _P_ < 0.001, Fig. 2a). There was no difference
between L, M and grey MVA thresholds (_P_ > 0.32) while both S cone monocular MVA (1.40) was reduced vs. L, M, luminance (1.26, mean difference 0.14, 95% CI 0.09–0.17, _P_ < 0.001) as
was S cone binocular MVA (difference 0.08, 95% CI 0.04–0.13, _P_ < 0.001, Fig. 2b). Binocular S cone MVA was decreased for oblique vs. horizontal/vertical (_P_ < 0.02). Binocular L
cone MVA was improved for horizontal compared to vertical (_P_ < 0.001). MVA binocular and orientation effects support cortical processing. Decreased S cone MVA reflects the paucity of S
cones. 50% enhancement of binocular vs. monocular MVA exceeds 40% for CS indicating binocular cortical processing. Improved L cone binocular horizontal MVA may increase disparity enhancing
stereoacuity. MVA shows promise for disease detection/monitoring, occupational application, and as an outcome for gene therapy. Ongoing research is assessing age, orientation, and color
naming. Preliminary results show high sensitivity for detection of color deficiency and improvement with color correcting lenses. REFERENCES * Rabin J, Gooch J, Ivan D, Harvey R, Aaron M.
Beyond 20/20: new clinical methods to quantify vision performance. Mil Med 2011;176:324–6. https://doi.org/10.7205/milmed-d-10-00320 Article PubMed Google Scholar * Westheimer G. The
spatial sense of the eye. Proctor lecture. Investig Ophthalmol Vis Sci. 1979;18:893–912. CAS Google Scholar * Levi DM, Polat U, Hu YS. Improvement in vernier acuity in adults with
amblyopia. Practice makes better. Investig Ophthalmol Vis Sci. 1997;38:1493–510. CAS Google Scholar * Hu M, Ayton LN, Jolly JK. The clinical use of vernier acuity: resolution of the visual
cortex is more than meets the eye. Front Neurosci. 2021;15:714843. https://doi.org/10.3389/fnins.2021.714843 Article PubMed PubMed Central Google Scholar * Rabin J, Gooch J, Ivan D.
Rapid quantification of color vision: the Cone Contrast Test. Investig Ophthalmol Vis Sci 2011;52:816–20. https://doi.org/10.1167/iovs Article Google Scholar Download references FUNDING
Research reported in this publication was supported by the National Eye Institute of the National Institutes of Health under Award Number T35EY032441. The content is solely the
responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Open access funding provided by SCELC, Statewide California
Electronic Library Consortium. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * University of the Incarnate Word Rosenberg School of Optometry, San Antonio, TX, USA Jeff Rabin, Katelyn Goodroe,
Alyssa Hood, Cara Duka, Kyle Dunmon, Darien Bouaphavong & Thinh Truong Authors * Jeff Rabin View author publications You can also search for this author inPubMed Google Scholar *
Katelyn Goodroe View author publications You can also search for this author inPubMed Google Scholar * Alyssa Hood View author publications You can also search for this author inPubMed
Google Scholar * Cara Duka View author publications You can also search for this author inPubMed Google Scholar * Kyle Dunmon View author publications You can also search for this author
inPubMed Google Scholar * Darien Bouaphavong View author publications You can also search for this author inPubMed Google Scholar * Thinh Truong View author publications You can also search
for this author inPubMed Google Scholar CONTRIBUTIONS JR was responsible for designing the protocol, data collection, results interpretation and analyses, manuscript writing, and research
oversight. KG, AH, CD, KD, DB, and TT were responsible for designing the protocol, data collection, collating data, data curation, results interpretation and analyses. Contributions and
access to data: The Principal Investigator, Jeff Rabin, had full access to all data and takes responsibility for the integrity of the data and the accuracy of the data analysis.
CORRESPONDING AUTHOR Correspondence to Jeff Rabin. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature
remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original
author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the
article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use
is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Rabin, J., Goodroe, K., Hood, A. _et al._ Minimum visual acuity: a new cone
specific clinical test. _Eye_ 39, 195–197 (2025). https://doi.org/10.1038/s41433-024-03377-7 Download citation * Received: 14 September 2024 * Revised: 18 September 2024 * Accepted: 23
September 2024 * Published: 27 September 2024 * Issue Date: January 2025 * DOI: https://doi.org/10.1038/s41433-024-03377-7 SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative