Play all audios:
ABSTRACT Short sleep duration has a substantial influence on the overall health of an individual. Short sleep time can be a consequence of lifestyle habits, environmental factors, or the
presence of a sleep disorder, such as insomnia or sleep-disordered breathing. Short sleep time is associated with increased morbidity and mortality, mainly from cardiovascular disorders
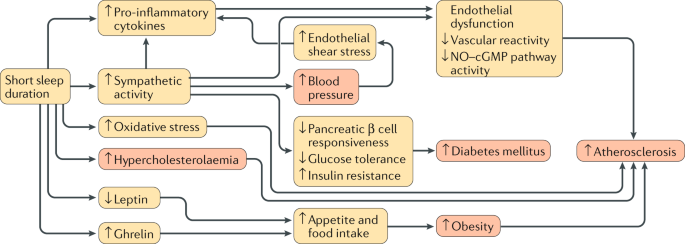
(including coronary artery disease, arrhythmias, and hypertension). Several biological mechanisms have been proposed as a possible link between short sleep duration and these diseases, such
as involvement of the autonomic nervous system, endothelial function, metabolic regulation, inflammation, and the coagulation system. In this Review, we provide an overview on the effects of
short sleep duration on cardiovascular health and diseases and discuss the main pathophysiological mechanisms involved, taking into account both experimental data and clinical evidence. KEY
POINTS * Regardless of the underlying cause, short duration of sleep seems to be associated with increased morbidity and mortality. * Experimental data show that sleep deprivation causes
important alterations in several intermediate biological mechanisms, such as the autonomic nervous system, endothelial function, insulin and glucose regulation, inflammation, and
coagulation. * Although a causal relationship between short sleep duration and cardiovascular risk is not confirmed, most of the data indicate a strong link between short sleep times and
diabetes mellitus, obesity, and cardiovascular disorders. * Physicians should consider sleep to be a modifiable risk factor for health status, with particular relevance to cardiovascular and
metabolic disorders. Access through your institution Buy or subscribe This is a preview of subscription content, access via your institution ACCESS OPTIONS Access through your institution
Access Nature and 54 other Nature Portfolio journals Get Nature+, our best-value online-access subscription $32.99 / 30 days cancel any time Learn more Subscribe to this journal Receive 12
print issues and online access $209.00 per year only $17.42 per issue Learn more Buy this article * Purchase on SpringerLink * Instant access to full article PDF Buy now Prices may be
subject to local taxes which are calculated during checkout ADDITIONAL ACCESS OPTIONS: * Log in * Learn about institutional subscriptions * Read our FAQs * Contact customer support SIMILAR
CONTENT BEING VIEWED BY OTHERS SLEEP DISTURBANCES: ONE OF THE CULPRITS OF OBESITY-RELATED CARDIOVASCULAR RISK? Article 20 July 2020 THE ASSOCIATION BETWEEN SLEEP DURATION AND HYPERTENSION: A
META AND STUDY SEQUENTIAL ANALYSIS Article 25 June 2020 INFLUENCE OF SLEEP ON PHYSIOLOGICAL SYSTEMS IN ATHEROSCLEROSIS Article 08 November 2024 REFERENCES * Watson, N. et al. Recommended
amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society. _J. Clin. Sleep Med._ 11, 931–952 (2015). Article
PubMed PubMed Central Google Scholar * Hirshkowitz, M. et al. National Sleep Foundation’s updated sleep duration recommendations: final report. _Sleep Heal._ 1, 233–243 (2015). Article
Google Scholar * Liu, Y. et al. Prevalence of healthy sleep duration among adults — United States, 2014. _MMWR Morb. Mortal. Wkly Rep._ 65, 137–141 (2016). Article PubMed Google Scholar
* Grandner, M. A., Patel, N. P., Gehrman, P. R., Perlis, M. L. & Pack, A. I. Problems associated with short sleep: bridging the gap between laboratory and epidemiological studies. _Sleep
Med. Rev._ 14, 239–247 (2010). Article PubMed Google Scholar * Wheaton, A. G., Jones, S. E., Cooper, A. C. & Croft, J. B. Short sleep duration among middle school and high school
students — United States, 2015. _MMWR Morb. Mortal. Wkly Rep._ 67, 85–90 (2018). Article PubMed PubMed Central Google Scholar * Schutte-rodin, S. et al. Clinical guideline for the
evaluation and management of chronic insomnia in adults. _J. Clin. Sleep Med._ 4, 487–504 (2008). PubMed PubMed Central Google Scholar * Young, T. et al. The occurrence of
sleep-disordered breathing among middle-aged adults. _N. Engl. J. Med._ 328, 1230–1235 (1993). Article CAS PubMed Google Scholar * Peppard, P. E. et al. Increased prevalence of
sleep-disordered breathing in adults. _Am. J. Epidemiol._ 177, 1006–1014 (2013). Article PubMed PubMed Central Google Scholar * Heinzer, R. et al. Prevalence of sleep-disordered
breathing in the general population: the HypnoLaus study. _Lancet Respir. Med._ 3, 310–318 (2015). Article CAS PubMed PubMed Central Google Scholar * Chin, K. et al. Associations
between obstructive sleep apnea, metabolic syndrome, and sleep duration, as measured with an actigraph, in an urban male working population in Japan. _Sleep_ 33, 89–95 (2010). Article
PubMed PubMed Central Google Scholar * Vgontzas, A. N. et al. Insomnia with short sleep duration and mortality: the Penn State cohort. _Hypertension_ 33, 1159–1164 (2010). Google Scholar
* Vgontzas, A. N., Fernandez-Mendoza, J., Liao, D. & Bixler, E. O. Insomnia with objective short sleep duration: the most biologically severe phenotype of the disorder. _Sleep Med.
Rev._ 17, 241–254 (2013). Article PubMed PubMed Central Google Scholar * Ren, R. et al. Objective but not subjective short sleep duration is associated with hypertension in obstructive
sleep apnea. _Hypertension_ 72, 610–617 (2018). Article CAS Google Scholar * Priou, P. et al. Cumulative association of obstructive sleep apnea severity and short sleep duration with the
risk for hypertension. _PLOS ONE_ 9, 1–12 (2014). Article CAS Google Scholar * Tobaldini, E. et al. Sleep, sleep deprivation, autonomic nervous system and cardiovascular diseases.
_Neurosci. Biobehav. Rev._ 74, 321–329 (2017). Article PubMed Google Scholar * Li, X. et al. U-shaped relationships between sleep duration and metabolic syndrome and metabolic syndrome
components in males: a prospective cohort study. _Sleep Med._ 16, 949–954 (2015). Article PubMed Google Scholar * Kim, J. Y. et al. A prospective study of total sleep duration and
incident metabolic syndrome: the ARIRANG study. _Sleep Med._ 16, 1511–1515 (2015). Article PubMed Google Scholar * Gottlieb, D. J. et al. Association of sleep time with diabetes mellitus
and impaired glucose tolerance. _Arch. Intern. Med._ 165, 863–867 (2005). Article PubMed Google Scholar * Wu, Y., Zhai, L. & Zhang, D. Sleep duration and obesity among adults: a
meta-analysis of prospective studies. _Sleep Med._ 15, 1456–1462 (2014). Article PubMed Google Scholar * Sabanayagam, C. & Shankar, A. Sleep duration and cardiovascular disease:
results from the National Health Interview Survey. _Sleep_ 33, 1037–1042 (2010). Article PubMed PubMed Central Google Scholar * Sauvet, F. et al. Effect of acute sleep deprivation on
vascular function in healthy subjects. _J. Appl. Physiol._ 108, 68–75 (2010). Article PubMed Google Scholar * Tobaldini, E. et al. One night on-call: sleep deprivation affects cardiac
autonomic control and inflammation in physicians. _Eur. J. Intern. Med._ 24, 664–670 (2013). Article PubMed Google Scholar * Zhong, X. et al. Increased sympathetic and decreased
parasympathetic cardiovascular modulation in normal humans with acute sleep deprivation. _J. Appl. Physiol._ 98, 2024–2032 (2005). Article PubMed Google Scholar * Dettoni, J. L. et al.
Cardiovascular effects of partial sleep deprivation in healthy volunteers. _J. Appl. Physiol._ 113, 232–236 (2012). Article CAS PubMed Google Scholar * Takase, B. et al. Effects of
chronic sleep deprivation on autonomic activity by examining heart rate variability, plasma catecholamine, and intracellular magnesium levels. _Biomed. Pharmacother._ 58, 35–39 (2004).
Article Google Scholar * Grimaldi, D., Carter, J. R., Van Cauter, E. & Leproult, R. Adverse impact of sleep restriction and circadian misalignment on autonomic function in healthy
young adults. _Hypertension_ 68, 243–250 (2016). Article CAS PubMed Google Scholar * Spiegel, K., Leproult, R. & Van Cauter, E. Impact of sleep debt on metabolic and endocrine
function. _Lancet_ 354, 1435–1439 (1999). Article CAS PubMed Google Scholar * Neufeld, E. V., Carney, J. J., Dolezal, B. A., Boland, D. M. & Cooper, C. B. Exploratory study of heart
rate variability and sleep among emergency medical services shift workers. _Prehospital Emerg_. _Care_ 21, 18–23 (2017). Google Scholar * Chung, M. et al. Recovery after three-shift work:
relation to sleep-related cardiac neuronal regulation in nurses. _Ind. Health_ 1, 24–30 (2012). Article Google Scholar * Su, T. C. et al. Elevated blood pressure, decreased heart rate
variability and incomplete blood pressure recovery after a 12-hour night shift work. _J. Occup. Health_ 50, 380–386 (2008). Article PubMed Google Scholar * Yamasaki, F., Schwartz, J. E.,
Gerber, L. M., Warren, K. & Pickering, T. G. Impact of shift work and race/ethnicity on the diurnal rhythm of blood pressure and catecholamines. _Hypertension_ 32, 417–423 (1998).
Article CAS PubMed Google Scholar * Irwin, M. R. Sleep deprivation and activation of morning levels of cellular and genomic markers of inflammation. _Arch. Intern. Med._ 166, 1756
(2006). Article CAS PubMed Google Scholar * Irwin, M. R., Witarama, T., Caudill, M., Olmstead, R. & Breen, E. C. Sleep loss activates cellular inflammation and signal transducer and
activator of transcription (STAT) family proteins in humans. _Brain. Behav. Immun._ 47, 86–92 (2015). Article CAS PubMed Google Scholar * Sauvet, F. et al. Vascular response to 1 week of
sleep restriction in healthy subjects. A metabolic response? _Int. J. Cardiol._ 190, 246–255 (2015). Article PubMed Google Scholar * Vgontzas, A. N. et al. Circadian interleukin-6
secretion and quantity and depth of sleep. _J. Clin. Endocrinol. Metab._ 84, 2603–2607 (1999). Article CAS PubMed Google Scholar * Meier-Ewert, H. K. et al. Effect of sleep loss on
C-Reactive protein, an inflammatory marker of cardiovascular risk. _J. Am. Coll. Cardiol._ 43, 678–683 (2004). Article CAS PubMed Google Scholar * van Leeuwen, W. M. A. et al. Sleep
restriction increases the risk of developing cardiovascular diseases by augmenting proinflammatory responses through IL-17 and CRP. _PLOS ONE_ 4, e4589 (2009). Article PubMed PubMed
Central CAS Google Scholar * Ferrie, J. E. et al. Associations between change in sleep duration and inflammation: findings on C-reactive protein and interleukin 6 in the Whitehall II
study. _Am. J. Epidemiol._ 178, 956–961 (2013). Article PubMed PubMed Central Google Scholar * Miller, M. a et al. Gender differences in the cross-sectional relationships between sleep
duration and markers of inflammation: Whitehall II study. _Sleep_ 32, 857–864 (2009). PubMed PubMed Central Google Scholar * Faraut, B., Boudjeltia, K. Z., Vanhamme, L. & Kerkhofs, M.
Immune, inflammatory and cardiovascular consequences of sleep restriction and recovery. _Sleep Med. Rev._ 16, 137–149 (2012). Article PubMed Google Scholar * Boudjeltia, K. et al.
Temporal dissociation between myeloperoxidase (MPO)-modified LDL and MPO elevations during chronic sleep restriction and recovery in healthy young men. _PLOS ONE_ 6, e28230 (2011). Article
PubMed CAS Google Scholar * Weil, B. R. et al. Short sleep duration is associated with enhanced endothelin-1 vasoconstrictor tone. _Can. J. Physiol. Pharmacol._ 88, 777–781 (2010).
Article CAS PubMed Google Scholar * Nakazaki, C. et al. Association of insomnia and short sleep duration with atherosclerosis risk in the elderly. _Am. J. Hypertens._ 25, 1149–1155
(2012). Article PubMed Google Scholar * Matthews, K. A., Dahl, R. E., Owens, J. F., Lee, L. & Hall, M. Sleep duration and insulin resistance in healthy black and white adolescents.
_Sleep_ 35, 1353–1358 (2012). Article PubMed PubMed Central Google Scholar * Rodrigues, De. Bernardi A. M. et al. Association of sleep deprivation with reduction in insulin sensitivity
as assessed by the hyperglycemic clamp technique in adolescents. _JAMA Pediatr._ 170, 487–494 (2016). Article Google Scholar * Reynolds, A. C. et al. Impact of five nights of sleep
restriction on glucose metabolism, leptin and testosterone in young adult men. _PLOS ONE_ 7, e41218 (2012). Article CAS PubMed PubMed Central Google Scholar * Donga, E. et al. Partial
sleep restriction decreases insulin sensitivity in type 1 diabetes. _Diabetes Care_ 33, 1573–1577 (2010). Article CAS PubMed PubMed Central Google Scholar * Francesco, T., Peverini, F.,
De Benedetto, M. & De Nuccio, F. Obstructive sleep apnea syndrome: blood viscosity, blood coagulation abnormalities, and early atherosclerosis. _Lung_ 191, 1–7 (2013). Article CAS
Google Scholar * Robinson, G. V., Pepperell, J. C. T., Segal, H. C., Davies, R. J. O. & Stradling, J. R. Circulating cardiovascular risk factors in obstructive sleep apnoea: data from
randomised controlled trials. _Thorax_ 59, 777–783 (2004). Article CAS PubMed PubMed Central Google Scholar * Kondo, Y. et al. Significant relationship between platelet activation and
apnea-hypopnea index in patients with obstructive sleep apnea syndrome. _Tokai J. Exp. Clin. Med._ 36, 79–83 (2011). PubMed Google Scholar * Von Känel, R. et al. Association between
polysomnographic measures of disrupted sleep and prothrombotic factors. _Chest_ 131, 733–739 (2007). Article Google Scholar * Libby, P. Inflammation and cardiovascular disease mechanisms.
_Am. J. Clin. Nutr._ 83, 456–460 (2006). Article Google Scholar * Visser, M., Bouter, L. M., Mcquillan, G. M., Wener, M. H. & Harris, T. B. Elevated C-reactive protein levels in
overweight and obese adults. _JAMA_ 282, 2131–2135 (1999). Article CAS PubMed Google Scholar * Danesh, J. et al. Fibrin D-dimer and coronary heart disease prospective study and
meta-analysis. _Circulation_ 103, 2323–2327 (2001). Article CAS PubMed Google Scholar * Kim, H. C. et al. Multimarker prediction of coronary heart disease risk. _J. Am. Coll. Cardiol._
55, 2080–2091 (2010). Article CAS PubMed Google Scholar * Münzel, T. et al. Impact of oxidative stress on the heart and vasculature: Part 2 of a 3-Part series. _J. Am. Coll. Cardiol._
70, 212–229 (2017). Article PubMed PubMed Central CAS Google Scholar * Itani, O., Jike, M., Watanabe, N. & Kaneita, Y. Short sleep duration and health outcomes: a systematic review,
meta-analysis, and meta-regression. _Sleep Med._ 32, 246–256 (2017). Article PubMed Google Scholar * Chien, K.-L. et al. Habitual sleep duration and insomnia and the risk of
cardiovascular events and all-cause death: report from a community-based cohort. _Sleep_ 33, 177–184 (2010). Article PubMed PubMed Central Google Scholar * Campanini, M. Z. et al.
Agreement between sleep diary and actigraphy in a highly educated Brazilian population. _Sleep Med._ 35, 27–34 (2017). Article PubMed Google Scholar * Lockley, S. W., Skene, D. J. &
Arendt, J. Comparison between subjective and actigraphic measurement of sleep and sleep rhythms. _J. Sleep Res._ 8, 175–183 (1999). Article CAS PubMed Google Scholar * Arora, T.,
Broglia, E., Pushpakumar, D., Lodhi, T. & Taheri, S. An investigation into the strength of the association and agreement levels between subjective and objective sleep duration in
adolescents. _PLOS ONE_ 8, 1–6 (2013). Google Scholar * Girschik, J., Fritschi, L., Heyworth, J. & Waters, F. Validation of self-reported sleep against actigraphy. _J. Epidemiol._ 22,
462–468 (2012). Article PubMed PubMed Central Google Scholar * Ross, R. Atherosclerosis — An inflammatory disease. _N. Engl. J. Med._ 340, 115–126 (1999). Article CAS PubMed Google
Scholar * Willerson, J. T. Inflammation as a cardiovascular risk factor. _Circulation_ 109, II2–10 (2004). PubMed Google Scholar * Vgontzas, A. N. et al. Adverse effects of modest sleep
restriction on sleepiness, performance, and inflammatory cytokines. _J. Clin. Endocrinol. Metab._ 89, 2119–2126 (2004). Article CAS PubMed Google Scholar * Orshal, J. M. & Khalil, R.
a. Interleukin-6 impairs endothelium-dependent NO-cGMP-mediated relaxation and enhances contraction in systemic vessels of pregnant rats. _Am. J. Physiol. Regul. Integr. Comp. Physiol_.
286, R1013–R1023 (2004). Article CAS PubMed Google Scholar * Gangwisch, J. E. et al. Short sleep duration as a risk factor for hypertension: analyses of the first National Health and
Nutrition Examination survey. _Hypertension_ 47, 833–839 (2006). Article CAS PubMed Google Scholar * Cappuccio, F. P. et al. Gender-specific associations of short sleep duration with the
Whitehall II study. _Hypertension_ 50, 693–700 (2007). Article CAS PubMed Google Scholar * Knutson, K. L. et al. Association between sleep and blood pressure in midlife. _Arch. Intern.
Med._ 169, 1055 (2009). Article PubMed PubMed Central Google Scholar * Ridker, P. M. C-reactive protein and the prediction of cardiovascular events among those at intermediate risk
moving an inflammatory hypothesis toward consensus. _J. Am. Coll. Cardiol._ 49, 2129–2138 (2007). Article CAS PubMed Google Scholar * Albert, C. M., Ma, J., Rifai, N., Stampfer, M. J.
& Ridker, P. M. Prospective study of C-reactive protein, homocysteine, and plasma lipid levels as predictors of sudden cardiac death. _Circulation_ 105, 2595–2599 (2002). Article CAS
PubMed Google Scholar * Danesh, J. et al. C-reactive protein and other circulating markers of inflammation in the prediction of coronary heart disease. _N. Engl. J. Med._ 350, 1387–1397
(2004). Article CAS PubMed Google Scholar * Calvin, A. D. et al. Experimental sleep restriction causes endothelial dysfunction in healthy humans. _J. Am. Heart Assoc._ 3, 1–7 (2014).
Article Google Scholar * Pongratz, G. & Straub, R. H. The sympathetic nervous response in inflammation. _Arthritis Res. Ther._ 16, 1–12 (2014). Article CAS Google Scholar * Podrez,
E. A., Schmitt, D., Hoff, H. F. & Hazen, S. L. Myeloperoxidase-generated reactive nitrogen species convert LDL into an atherogenic form in vitro. _J. Clin. Invest._ 103, 1547–1560
(1999). Article CAS PubMed PubMed Central Google Scholar * van Leeuwen, W. M. A. et al. Prolonged sleep restriction affects glucose metabolism in healthy young men. _Int. J.
Endocrinol._ 2010, 108641 (2010). PubMed PubMed Central Google Scholar * Paneni, F., Diaz Cañestro, C., Libby, P., Lüscher, T. F. & Camici, G. G. The aging cardiovascular system:
understanding it at the cellular and clinical levels. _J. Am. Coll. Cardiol._ 69, 1952–1967 (2017). Article PubMed Google Scholar * Miller, M. A., Kandala, N., Kumari, M., Marmot, M. G.
& Cappuccio, F. P. Clinical and population studies relationships between sleep duration and von Willebrand factor, factor vii, and fibrinogen Whitehall II study. _Arter. Thromb. Vasc.
Biol._ 30, 2032–2039 (2010). Article CAS Google Scholar * Tosur, Z. et al. The association between sleep characteristics and prothrombotic markers in a population based sample: Chicago
area sleep study. _Sleep Med._ 15, 973–978 (2014). Article PubMed PubMed Central Google Scholar * Chouchou, F. et al. Sympathetic overactivity due to sleep fragmentation is associated
with elevated diurnal systolic blood pressure in healthy elderly subjects: the PROOF-SYNAPSE study. _Eur. Heart J._ 34, 2122–2131 (2013). Article CAS PubMed Google Scholar * Muenter, N.
K. et al. Effect of sleep restriction on orthostatic cardiovascular control in humans. _J. Appl. Physiol._ 88, 966–972 (2000). Article CAS PubMed Google Scholar * Sforza, E. et al. Heart
rate activation during spontaneous arousals from sleep: effect of sleep deprivation. _Clin. Neurophysiol._ 115, 2442–2451 (2004). Article PubMed Google Scholar * Malliani, A. &
Montano, N. Emerging excitatory role of cardiovascular sympathetic afferents in pathophysiological conditions. _Hypertension_ 39, 63–68 (2002). Article CAS PubMed Google Scholar * Shen,
M. J. & Zipes, D. P. Role of the autonomic nervous system in modulating cardiac arrhythmias. _Circ. Res._ 114, 1004–1021 (2014). Article CAS PubMed Google Scholar * Agarwal, S. K. et
al. Cardiac autonomic dysfunction and incidence of atrial fibrillation in a large population-based cohort. _J. Am. Coll. Cardiol._ 69, 291–299 (2017). Article PubMed PubMed Central
Google Scholar * Meredith, I. T., Broughton, A., Jennings, G. L. & Esler, M. D. Evidence of a selective increase in cardiac sympathetic activity in patients with sustained ventricular
arrhythmias. _N. Engl. J. Med._ 325, 618–624 (1991). Article CAS PubMed Google Scholar * Mancia, G. & Grassi, G. The autonomic nervous system and hypertension. _Circ. Res._ 114,
1804–1814 (2014). Article CAS PubMed Google Scholar * Airaksinen, K. E., Ikaheimo, M. J., Linnaluoto, M. K., Niemela, M. & Takkunen, J. T. Impaired vagal heart rate control in
coronary artery disease. _Heart_ 58, 592–597 (1987). Article CAS Google Scholar * Kochiadakis, G. E. et al. Autonomic nervous system activity before and during episodes of myocardial
ischemia in patients with stable coronary artery disease during daily life. _Pacing Clin. Electrophysiol._ 23, 2030–2039 (2000). Article CAS PubMed Google Scholar * Huikuri, H. V. et al.
Heart rate variability and progression of coronary atherosclerosis. _Arter. Thromb. Vasc. Biol._ 19, 1979–1985 (1999). Article CAS Google Scholar * van Bilsen, M. et al. The autonomic
nervous system as a therapeutic target in heart failure: a scientific position statement from the Translational Research Committee of the Heart Failure Association of the European Society of
Cardiology. _Eur. J. Hear. Fail._ 19, 1361–1378 (2017). Article Google Scholar * Floras, J. S. & Ponikowski, P. The sympathetic/parasympathetic imbalance in heart failure with reduced
ejection fraction. _Eur. Heart J._ 36, 1974–1982 (2015). Article CAS PubMed PubMed Central Google Scholar * Wang, Y. et al. Chronic sleep fragmentation promotes obesity in young adult
mice. _Obesity_ 22, 758–762 (2014). Article CAS PubMed Google Scholar * Tracey, K. J. The inflammatory reflex. _Nature_ 420, 853–859 (2002). Article CAS PubMed Google Scholar *
Itani, O., Kaneita, Y., Murata, A., Yokoyama, E. & Ohida, T. Association of onset of obesity with sleep duration and shift work among Japanese adults. _Sleep Med._ 12, 341–345 (2011).
Article PubMed Google Scholar * Cassidy, S., Chau, J. Y., Catt, M., Bauman, A. & Trenell, M. I. Cross-sectional study of diet, physical activity, television viewing and sleep duration
in 233 110 adults from the UK Biobank; the behavioural phenotype of cardiovascular disease and type 2 diabetes. _BMJ Open_ 6, e010038 (2016). Article PubMed PubMed Central Google Scholar
* Venancio, D. P. & Suchecki, D. Prolonged REM sleep restriction induces metabolic syndrome-related changes: mediation by pro-inflammatory cytokines. _Brain Behav. Immun._ 47, 109–117
(2015). Article CAS PubMed Google Scholar * Moraes, D. A., Venancio, D. P. & Suchecki, D. Sleep deprivation alters energy homeostasis through non-compensatory alterations in
hypothalamic insulin receptors in Wistar rats. _Horm. Behav._ 66, 705–712 (2014). Article CAS PubMed Google Scholar * Zhan, S. et al. Decrease in circulating fatty acids is associated
with islet dysfunction in chronically sleep-restricted rats. _Int. J. Mol. Sci._ 17, 2102 (2016). Article PubMed Central CAS Google Scholar * Jha, P. K., Foppen, E., Kalsbeek, A. &
Challet, E. Sleep restriction acutely impairs glucose tolerance in rats. _Physiol_. _Rep._ 4, e12839 (2016). Google Scholar * Spiegel, K., Tasali, E., Penev, P. & Van Cauter, E. Brief
communication: Sleep curtailment in healthy young men is associated with decreased leptin levels, elevated ghrelin levels, and increased hunger and appetite. _Ann. Intern. Med._ 141, 846–850
(2004). Article PubMed Google Scholar * Broussard, J. L. et al. Insulin access to skeletal muscle is impaired during the early stages of diet-induced obesity. _Obesity_ 24, 1922–1928
(2016). Article CAS PubMed Google Scholar * Chapman, C. D. et al. Acute sleep deprivation increases food purchasing in men. _Obesity_ 21, E555–E560 (2013). Article CAS PubMed Google
Scholar * St-Onge, M.-P., O’Keeffe, M., Roberts, A. L., RoyChoudhury, A. & Laferrere, B. Short sleep duration, glucose dysregulation and hormonal regulation of appetite in men and
women. _Sleep_ 35, 1503–1510 (2012). Article PubMed PubMed Central Google Scholar * Markwald, R. R. et al. Impact of insufficient sleep on total daily energy expenditure, food intake,
and weight gain. _Proc. Natl Acad. Sci. USA_ 110, 5695–5700 (2013). Article CAS PubMed PubMed Central Google Scholar * de Oliveira, E. M. et al. Serum amyloid A production is triggered
by sleep deprivation in mice and humans: is that the link between sleep loss and associated comorbidities? _Nutrients_ 9, E311 (2017). Article PubMed CAS Google Scholar * DePorter, D.
P., Coborn, J. E. & Teske, J. A. Partial sleep deprivation reduces the efficacy of orexin-A to stimulate physical activity and energy expenditure. _Obesity_ 25, 1716–1722 (2017). Article
CAS PubMed Google Scholar * Parrish, J. B. & Teske, J. A. Acute partial sleep deprivation due to environmental noise increases weight gain by reducing energy expenditure in rodents.
_Obesity_ 25, 141–146 (2017). Article PubMed Google Scholar * de Oliveira, E. M. et al. Late effects of sleep restriction: potentiating weight gain and insulin resistance arising from a
high-fat diet in mice. _Obesity_ 23, 391–398 (2015). Article PubMed CAS Google Scholar * Zhang, S. X. L. et al. Sleep fragmentation promotes NADPH oxidase 2-mediated adipose tissue
inflammation leading to insulin resistance in mice. _Int. J. Obes._ 38, 619–624 (2014). Article CAS Google Scholar * Weyer, C. et al. Hypoadiponectinemia in obesity and type 2 diabetes:
close association with insulin resistance and hyperinsulinemia. _J. Clin. Endocrinol. Metab._ 86, 1930–1935 (2001). Article CAS PubMed Google Scholar * Yamauchi, T. et al. The
fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. _Nat. Med._ 7, 941–946 (2001). Article CAS PubMed Google Scholar * Simpson, N.
S., Banks, S., Arroyo, S. & Dinges, D. F. Effects of sleep restriction on adiponectin levels in healthy men and women. _Physiol. Rep._ 101, 693–698 (2010). CAS Google Scholar *
Nilsson, P. M., Rööst, M., Engström, G., Hedblad, B. & Berglund, G. Incidence of diabetes in middle-aged men is related to sleep disturbances. _Diabetes Care_ 27, 2464–2469 (2004).
Article PubMed Google Scholar * Tasali, E., Leproult, R., Ehrmann, D. A. & Van Cauter, E. Slow-wave sleep and the risk of type 2 diabetes in humans. _Proc. Natl Acad. Sci. USA_ 105,
1044–1049 (2008). Article CAS PubMed PubMed Central Google Scholar * Benedict, C., Barclay, J. L., Ott, V., Oster, H. & Hallschmid, M. Acute sleep deprivation delays the
glucagon-like peptide 1 peak response to breakfast in healthy men. _Nutr. Diabetes_ 3, e78 (2013). Article CAS PubMed PubMed Central Google Scholar * Aho, V. et al. Prolonged sleep
restriction induces changes in pathways involved in cholesterol metabolism and inflammatory responses. _Sci. Rep._ 6, 24828 (2016). Article CAS PubMed PubMed Central Google Scholar *
O’Keeffe, M., Roberts, A. L., Kelleman, M., RoyChoudhury, A. & St-Onge, M.-P. No effects of short-term sleep restriction, in a controlled feeding setting, on lipid profiles in normal
weight adults. _J. Sleep Res_. 22 (2013). * Skuladottir, G. V., Nilsson, E. K., Mwinyi, J. & Schioth, H. B. One-night sleep deprivation induces changes in the DNA methylation and serum
activity indices of stearoyl-CoA desaturase in young healthy men. _Lipids Health Dis._ 15, 137 (2016). Article PubMed PubMed Central CAS Google Scholar * Broussard, J. L. et al. Sleep
restriction increases free fatty acids in healthy men. _Diabetologia_ 58, 791–798 (2015). Article CAS PubMed PubMed Central Google Scholar * Riggs, D. W., Yeager, R. A. & Bhatnagar,
A. An omics approach for assessing the environmental risk of cardiovascular disease. _Circ. Res._ 122, 1259–1275 (2018). Article CAS PubMed PubMed Central Google Scholar * Cappuccio,
F. P., Cooper, D., D.’Elia, L., Strazzullo, P. & Miller, M. A. Sleep duration predicts cardiovascular outcomes: a systematic review and meta-analysis of prospective studies. _Eur. Heart
J_. 32, 1484–1492 (2011). Article PubMed Google Scholar * Ikehara, S. et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and
women: the JACC study. _Sleep_ 32, 295–301 (2009). Article PubMed PubMed Central Google Scholar * Pepin, J. L. et al. Hypertension and sleep: overview of a tight relationship. _Sleep
Med. Rev._ 18, 509–519 (2014). Article PubMed Google Scholar * Gottlieb, D. J. et al. Association of usual sleep duration with hypertension: the Sleep Heart Health Study. _Sleep_ 29,
1009–1014 (2006). Article PubMed Google Scholar * Guo, X. et al. Epidemiological evidence for the link between sleep duration and high blood pressure: a systematic review and
meta-analysis. _Sleep Med._ 14, 324–332 (2013). Article PubMed Google Scholar * Wang, Q., Xi, B., Liu, M., Zhang, Y. & Fu, M. Short sleep duration is associated with hypertension risk
among adults: a systematic review and meta-analysis. _Hypertens. Res._ 35, 1012–1018 (2012). Article PubMed Google Scholar * Wang, Y. et al. Relationship between duration of sleep and
hypertension in adults: a meta-analysis. _J. Clin. Sleep Med._ 11, 1047–1056 (2015). PubMed PubMed Central Google Scholar * Meng, L., Zheng, Y. & Hui, R. The relationship of sleep
duration and insomnia to risk of hypertension incidence: a meta-analysis of prospective cohort studies. _Hypertens. Res._ 36, 985–995 (2013). Article PubMed PubMed Central Google Scholar
* Wu, X. et al. Association of self-reported sleep duration and hypertension: results of a Chinese prospective cohort study. _Clin. Exp. Hypertens._ 38, 514–519 (2016). Article PubMed
Google Scholar * Kim, J. & Jo, I. Age-dependent association between sleep duration and hypertension in the adult Korean population. _Am. J. Hypertens._ 23, 1286–1291 (2010). Article
PubMed Google Scholar * Fang, J. et al. Association of sleep duration and hypertension among US adults varies by age and sex. _Am. J. Hypertens._ 25, 335–341 (2012). Article PubMed
Google Scholar * Stranges, S. et al. A population-based study of reduced sleep duration and hypertension: the strongest association may be in premenopausal women. _J. Hypertens._ 28,
896–902 (2010). Article CAS PubMed Google Scholar * Javaheri, S., Storfer-Isser, A., Rosen, C. L. & Redline, S. Sleep quality and elevated blood pressure in adolescents.
_Circulation_ 118, 1034–1040 (2008). Article PubMed PubMed Central Google Scholar * Ramos, A. R. et al. Sleep patterns and hypertension using actigraphy in the Hispanic Community Health
Study/Study of Latinos. _Chest_ 153, 87–93 (2018). Article PubMed Google Scholar * Haack, M. et al. Increasing sleep duration to lower beat-to-beat blood pressure — a pilot study. _J.
Sleep Res._ 22, 295–304 (2013). Article PubMed Google Scholar * Acar, G. et al. Acute sleep deprivation in healthy adults is associated with a reduction in left atrial early diastolic
strain rate. _Sleep Breath._ 17, 975–983 (2013). Article PubMed Google Scholar * Cakici, M. et al. Negative effects of acute sleep deprivation on left ventricular functions and cardiac
repolarization in healthy young adults. _Pacing Clin. Electrophysiol._ 38, 713–722 (2015). Article PubMed Google Scholar * Ozer, O. et al. Acute sleep deprivation is associated with
increased QT dispersion in healthy young adults. _Pacing Clin. Electrophysiol._ 31, 979–984 (2008). Article PubMed Google Scholar * Miner, S. E. S. et al. Sleep disruption is associated
with increased ventricular ectopy and cardiac arrest in hospitalized adults. _Sleep_ 39, 927–935 (2016). Article PubMed PubMed Central Google Scholar * Ayas, N. T. et al. A prospective
study of sleep duration and coronary heart disease in women. _Arch. Intern. Med._ 163, 205–209 (2003). Article PubMed Google Scholar * Chandola, T., Ferrie, J. E., Perski, A., Akbaraly,
T. & Marmot, M. G. The effect of short sleep duration on coronary heart disease risk is greatest among those with sleep disturbance: a prospective study from the Whitehall II cohort.
_Sleep_ 33, 739–744 (2010). Article PubMed PubMed Central Google Scholar * Liu, Y., Wheaton, A. G., Chapman, D. P. & Croft, J. B. Sleep duration and chronic diseases among US adults
age 45 years and older: evidence from the 2010 Behavioral Risk Factor Surveillance System. _Sleep_ 36, 1421–1427 (2013). Article PubMed PubMed Central Google Scholar * King, C. R. et al.
Short sleep duration and incident coronary artery calcification. _JAMA_ 300, 2859–2866 (2008). Article CAS PubMed PubMed Central Google Scholar * Barger, L. K. et al. Short sleep
duration, obstructive sleep apnea, shiftwork, and the risk of adverse cardiovascular events in patients after an acute coronary syndrome. _J. Am. Heart Assoc._ 6, e006959 (2017). Article
PubMed PubMed Central Google Scholar * McHill, A. W. & Wright, K. P. J. Role of sleep and circadian disruption on energy expenditure and in metabolic predisposition to human obesity
and metabolic disease. _Obes. Rev._ 18 (Suppl. 1), 15–24 (2017). Article PubMed Google Scholar * Rafalson, L., Donahue, R. P. & Trevisan, M. Short sleep duration is associated with
the development of impaired fasting glucose: the Western New York Health study. _Ann. Epidemiol._ 20, 883–889 (2010). Article PubMed PubMed Central Google Scholar * Spiegel, K., Tasali,
E., Leproult, R. & Van Cauter, E. Effects of poor and short sleep on glucose metabolism and obesity risk. _Nat. Rev. Endocrinol._ 5, 253–261 (2009). Article CAS PubMed PubMed Central
Google Scholar * Cohen, D. A. et al. Uncovering residual effects of chronic sleep loss on human performance. _Sci. Transl. Med._ 2, 14ra3 (2010). Article PubMed PubMed Central Google
Scholar * Buxton, O. M. et al. Adverse metabolic consequences in humans of prolonged sleep restriction combined with circadian disruption. _Sci. Transl. Med_. 4, 129ra43 (2012). Article
PubMed PubMed Central Google Scholar * Broussard, J. L., Ehrmann, D. A., Van Cauter, E., Tasali, E. & Brady, M. J. Impaired insulin signaling in human adipocytes after experimental
sleep restriction: a randomized, crossover study. _Ann. Intern. Med._ 157, 549–557 (2012). Article PubMed PubMed Central Google Scholar * Cappuccio, F. P. & Miller, M. A. Sleep and
cardio-metabolic disease. _Curr. Cardiol. Rep._ 19, 110 (2017). Article PubMed PubMed Central Google Scholar * Al Khatib, H. K., Harding, S. V., Darzi, J. & Pot, G. K. The effects of
partial sleep deprivation on energy balance: a systematic review and meta-analysis. _Eur. J. Clin. Nutr._ 71, 614–624 (2017). Article CAS PubMed Google Scholar * Nuyujukian, D. S. et
al. Sleep duration and diabetes risk in American Indian and Alaska Native participants of a lifestyle intervention project. _Sleep_ 39, 1919–1926 (2016). Article PubMed PubMed Central
Google Scholar * Heianza, Y. et al. Role of sleep duration as a risk factor for Type 2 diabetes among adults of different ages in Japan: the Niigata Wellness study. _Diabet. Med._ 31,
1363–1367 (2014). Article CAS PubMed Google Scholar * Beihl, D. A., Liese, A. D. & Haffner, S. M. Sleep duration as a risk factor for incident type 2 diabetes in a multiethnic
cohort. _Ann. Epidemiol._ 19, 351–357 (2009). Article PubMed Google Scholar * Bromley, L. E., Booth, J. N. 3rd, Kilkus, J. M., Imperial, J. G. & Penev, P. D. Sleep restriction
decreases the physical activity of adults at risk for type 2 diabetes. _Sleep_ 35, 977–984 (2012). Article PubMed PubMed Central Google Scholar * Booth, J. N. et al. Reduced physical
activity in adults at risk for type 2 diabetes who curtail their sleep. _Obesity_ 20, 278–284 (2012). Article PubMed Google Scholar * Leproult, R., Deliens, G., Gilson, M. & Peigneux,
P. Beneficial impact of sleep extension on fasting insulin sensitivity in adults with habitual sleep restriction. _Sleep_ 38, 707–715 (2015). Article PubMed PubMed Central Google Scholar
* Krueger, P. M., Reither, E. N., Peppard, P. E., Burger, A. E. & Hale, L. Cumulative exposure to short sleep and body mass outcomes: a prospective study. _J. Sleep Res._ 24, 629–638
(2015). Article PubMed PubMed Central Google Scholar * Li, L., Zhang, S., Huang, Y. & Chen, K. Sleep duration and obesity in children: a systematic review and meta-analysis of
prospective cohort studies. _J. Paediatr. Child Health_ 53, 378–385 (2017). Article PubMed Google Scholar * Morrissey, B. et al. Sleep duration and risk of obesity among a sample of
Victorian school children. _BMC Publ_. _Health_ 16, 245 (2016). Google Scholar * Halal, C. S. E. et al. Short sleep duration in the first years of life and obesity/overweight at age 4
years: a birth cohort study. _J. Pediatr._ 168, 99–103.e3 (2016). Article PubMed PubMed Central Google Scholar * Martinez, S. M. et al. Is it time for bed? Short sleep duration increases
risk of obesity in Mexican American children. _Sleep Med._ 15, 1484–1489 (2014). Article PubMed PubMed Central Google Scholar * Taveras, E. M., Gillman, M. W., Pena, M.-M., Redline, S.
& Rifas-Shiman, S. L. Chronic sleep curtailment and adiposity. _Pediatrics_ 133, 1013–1022 (2014). Article PubMed PubMed Central Google Scholar * Martinez, S. M. et al. Short sleep
duration is associated with eating more carbohydrates and less dietary fat in Mexican American children. _Sleep_ 40, zsw057 (2017). Article Google Scholar * Beebe, D. W. et al. Dietary
intake following experimentally restricted sleep in adolescents. _Sleep_ 36, 827–834 (2013). Article PubMed PubMed Central Google Scholar * Mullins, E. N. et al. Acute sleep restriction
increases dietary intake in preschool-age children. _J. Sleep Res._ 26, 48–54 (2017). Article PubMed Google Scholar * Garaulet, M. et al. Short sleep duration is associated with increased
obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. _Int. J. Obes._ 35, 1308–1317 (2011). Article CAS Google Scholar * Wang, F. et
al. Sleep duration and overweight/obesity in preschool-aged children: a prospective study of up to 48,922 children of the Jiaxing birth cohort. _Sleep_ 39, 2013–2019 (2016). Article PubMed
PubMed Central Google Scholar * Cespedes, E. M. et al. Chronic insufficient sleep and diet quality: contributors to childhood obesity. _Obesity_ 24, 184–190 (2016). Article PubMed
Google Scholar * Kobayashi, D., Takahashi, O., Deshpande, G. A., Shimbo, T. & Fukui, T. Association between weight gain, obesity, and sleep duration: a large-scale 3-year cohort study.
_Sleep Breath._ 16, 829–833 (2012). Article PubMed Google Scholar * Haghighatdoost, F., Karimi, G., Esmaillzadeh, A. & Azadbakht, L. Sleep deprivation is associated with lower diet
quality indices and higher rate of general and central obesity among young female students in Iran. _Nutrition_ 28, 1146–1150 (2012). Article PubMed Google Scholar * Sun, W. et al. Sleep
duration associated with body mass index among Chinese adults. _Sleep Med._ 16, 612–616 (2015). Article PubMed Google Scholar * Kim, K., Shin, D., Jung, G.-U., Lee, D. & Park, S. M.
Association between sleep duration, fat mass, lean mass and obesity in Korean adults: the fourth and fifth Korea National Health and Nutrition Examination surveys. _J. Sleep Res._ 26,
453–460 (2017). Article PubMed Google Scholar * Theorell-Haglow, J., Berglund, L., Berne, C. & Lindberg, E. Both habitual short sleepers and long sleepers are at greater risk of
obesity: a population-based 10-year follow-up in women. _Sleep Med._ 15, 1204–1211 (2014). Article PubMed Google Scholar * Sperry, S. D., Scully, I. D., Gramzow, R. H. & Jorgensen, R.
S. Sleep Duration and waist circumference in adults: a meta-analysis. _Sleep_ 38, 1269–1276 (2015). Article PubMed PubMed Central Google Scholar * Chaput, J.-P., McNeil, J., Despres,
J.-P., Bouchard, C. & Tremblay, A. Short sleep duration as a risk factor for the development of the metabolic syndrome in adults. _Prev. Med._ 57, 872–877 (2013). Article PubMed Google
Scholar * Thomson, C. A. et al. Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. _Obesity_ 20, 1419–1425 (2012).
Article PubMed Google Scholar * Chaput, J.-P. & Dutil, C. Lack of sleep as a contributor to obesity in adolescents: impacts on eating and activity behaviors. _Int. J. Behav. Nutr.
Phys. Act._ 13, 103 (2016). Article PubMed PubMed Central Google Scholar * Tasali, E., Chapotot, F., Wroblewski, K. & Schoeller, D. The effects of extended bedtimes on sleep duration
and food desire in overweight young adults: a home-based intervention. _Appetite_ 80, 220–224 (2014). Article PubMed PubMed Central Google Scholar * Lucassen, E. A. et al. Sleep
extension improves neurocognitive functions in chronically sleep-deprived obese individuals. _PLOS ONE_ 9, e84832 (2014). Article PubMed PubMed Central CAS Google Scholar * Scheer, F.
A. J. L., Van Montfrans, G. A., Van Someren, E. J. W., Mairuhu, G. & Buijs, R. M. Daily nighttime melatonin reduces blood pressure in male patients with essential hypertension.
_Hypertension_ 43, 192–197 (2004). Article CAS PubMed Google Scholar * Grossman, E. et al. Melatonin reduces night blood pressure in patients with nocturnal hypertension. _Am. J. Med._
119, 898–902 (2006). Article CAS PubMed Google Scholar * Sateia, M. J. International classification of sleep disorders - third edition. _Chest_ 146, 1387–1394 (2014). Article PubMed
Google Scholar Download references ACKNOWLEDGEMENTS REVIEWER INFORMATION _Nature Reviews Cardiology_ thanks M. A. Grandner, O. Oldenburg and the other anonymous reviewer(s) for their
contribution to the peer review of this work. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Internal Medicine, Fondazione IRCCS Ca’ Granda, Ospedale Maggiore Policlinico and
Department of Clinical Sciences and Community Health, University of Milan, Milan, Italy Eleonora Tobaldini, Elisa M. Fiorelli, Monica Solbiati, Giorgio Costantino & Nicola Montano *
Child Neuropsychiatry Unit, IRCCS Istituto Giannina Gaslini, DINOGMI, University of Genoa, Genoa, Italy Lino Nobili Authors * Eleonora Tobaldini View author publications You can also search
for this author inPubMed Google Scholar * Elisa M. Fiorelli View author publications You can also search for this author inPubMed Google Scholar * Monica Solbiati View author publications
You can also search for this author inPubMed Google Scholar * Giorgio Costantino View author publications You can also search for this author inPubMed Google Scholar * Lino Nobili View
author publications You can also search for this author inPubMed Google Scholar * Nicola Montano View author publications You can also search for this author inPubMed Google Scholar
CONTRIBUTIONS E.T., E.M.F., and N.M. researched data for the article and wrote the manuscript. E.T., M.S., G.C., L.N., and N.M. discussed the content of the article, and E.M.F., M.S., G.C.,
L.N., and N.M. reviewed and edited it before submission. CORRESPONDING AUTHOR Correspondence to Nicola Montano. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing
interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. GLOSSARY *
Actigraphy A method for noninvasive monitoring of rest and activity cycles in humans via a wrist-worn device; although actigraphy is not the gold standard for diagnosing a sleep disorder, it
is a useful research tool because data can be recorded inexpensively and in a natural sleep environment. * Polysomnography A type of sleep study, based on the simultaneous recording of
several biological functions during sleep (electrocardiogram, respiration, brain activity, muscles, and ocular movements); in clinical practice, polysomnography is the gold-standard
technique for recording sleep and diagnosing sleep disorders. * Non-dipper profile In ambulatory blood-pressure monitoring, a non-dipper profile is characterized by the absence of a
physiological fall in blood pressure during night time compared with daytime. RIGHTS AND PERMISSIONS Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Tobaldini, E., Fiorelli,
E.M., Solbiati, M. _et al._ Short sleep duration and cardiometabolic risk: from pathophysiology to clinical evidence. _Nat Rev Cardiol_ 16, 213–224 (2019).
https://doi.org/10.1038/s41569-018-0109-6 Download citation * Published: 08 November 2018 * Issue Date: April 2019 * DOI: https://doi.org/10.1038/s41569-018-0109-6 SHARE THIS ARTICLE Anyone
you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the
Springer Nature SharedIt content-sharing initiative