Play all audios:
ABSTRACT Extracellular vesicles (EVs) from mesenchymal stromal cells (MSC) are emerging as valuable therapeutic agents for tissue regeneration and immunomodulation, but their clinical
applications have so far been limited by the technical restraints of current isolation and characterisation procedures. This study shows for the first time the successful application of
Raman spectroscopy as label-free, sensitive and reproducible means of carrying out the routine bulk characterisation of MSC-derived vesicles before their use _in vitro_ or _in vivo_, thus
promoting the translation of EV research to clinical practice. The Raman spectra of the EVs of bone marrow and adipose tissue-derived MSCs were compared with human dermal fibroblast EVs in
order to demonstrate the ability of the method to distinguish the vesicles of the three cytotypes automatically with an accuracy of 93.7%. Our data attribute a Raman fingerprint to EVs from
undifferentiated and differentiated cells of diverse tissue origin, and provide insights into the biochemical characteristics of EVs from different sources and into the differential
contribution of sphingomyelin, gangliosides and phosphatidilcholine to the Raman spectra themselves. SIMILAR CONTENT BEING VIEWED BY OTHERS BIOMOLECULAR PHENOTYPING AND HETEROGENEITY
ASSESSMENT OF MESENCHYMAL STROMAL CELLS USING LABEL-FREE RAMAN SPECTROSCOPY Article Open access 23 February 2021 ISOLATION AND CHARACTERIZATION OF EXTRACELLULAR VESICLE SUBPOPULATIONS FROM
TISSUES Article 25 January 2021 MESENCHYMAL STEM CELL-DERIVED EXTRACELLULAR VESICLES FOR IMMUNOMODULATION AND REGENERATION: A NEXT GENERATION THERAPEUTIC TOOL? Article Open access 04 July
2022 INTRODUCTION Extracellular vesicles (EVs) are a heterogeneous group of membrane-bound vesicles that are constitutively released by cells of different tissue origins. Past controversies
concerning nomenclature have now been resolved by the scientific community, which defines EVs as the group of particles made up of exosomes, microvesicles and apoptotic bodies1. Exosomes
(30–100 nm) and microvesicles (up to 1000 nm) differ in size and cellular origin, but both mediate intercellular communication within a tissue and among organs thanks to body fluid
transportation1. As is the case for most body cells, part of the secretome of mesenchymal stromal cells (MSCs) includes exosomes and microvesicles, which are currently being investigated
because of their striking regenerative and immunomodulating potential. The bioactive molecules loaded onto/into EVs are involved in the paracrine effects of stem cells, and even the membrane
constituents of vesicles seem to trigger intracellular protective/regenerative pathways in recipient cells2. It has been suggested that MSC-derived EVs may be sometimes even more
therapeutically valuable than whole cells, because of their remarkable handling advantages, which can accelerate their clinical application in the so-called _cell therapy without cells_ 3.
The possibility of overcoming the cell therapy drawbacks of having to administer living, replicating and difficult to control cells is currently one of the main challenges facing
regenerative medicine, and EVs can be an effective means of stimulating the restoration of organ function through tissue regeneration and repair in the context of an integrated strategy of
_regenerative rehabilitation_ 4. Over the last ten years, many studies have demonstrated the role that MSC-derived EVs can play in tissue repair and immunomodulation5, 6 and, in 2014, EVs
ability to influence the activity of recipient cells and regulate immune responses was successfully exploited in a patient undergoing allogeneic hematopoietic stem cell transplantation who
developed therapy-refractory graft-versus-host disease7. Their regenerative potential has also been assessed in _in vitro_ and _in vivo_ models of many diseases affecting heart8,9,10,
kidney11,12,13, liver14, 15, bone and cartilage16, 17, muscle18, skin19, and central nervous system20,21,22,23. However, there are still concerns about the effect that the source of MSCs and
cell culture conditions can have on EV production and characteristics as there is no standardised and optimised method for isolating and characterising EVs. Furthermore, the technical
restraints of current techniques have limited their potential use in regenerative medicine24, 25 by preventing reproducible quality and safety assessments26. The aim of this study was to
test Raman spectroscopy (RS) as a label-free, non-destructive, sensitive, rapid and automatable means of carrying out the bulk characterization of EVs. This technique provides a spectrum
that qualitatively and quantitatively describes the chemical composition of a sample and thus avoids the need for specific protein biomarkers. It has been widely used in the pharmaceutical
industry as a mean of verifying raw materials and quality controlling drug production, and we suggest it could help in purity and quality checking vesicle suspensions. It has already proved
its value by characterising a wide range of cells and tissue samples for the purposes of basic research, and as an innovative alternative to classic, time-consuming and operator-dependent
diagnostic methods27,28,29,30,31,32,33,34. In the field of regenerative medicine, it has been used to analyse undifferentiated and differentiated human and murine embryonic stem
cells35,36,37 and to monitor MSCs stimulated towards osteogenic differentiation38, 39. Efforts have also been made to develop Raman-based methods for the individual characterisation of human
vesicles40, 41, but although these have provided information at single-vesicle level, they are still far from being used diagnostically. What is required to allow the immediate
transferability of EV research to clinical practice is a procedure that allows i) the rapid characterisation of a sample before its use _in vitro_ or _in vivo_; ii) the identification of
fingerprints of the EV populations used for regenerative purposes in order to determine the best experimental settings and compare results from different cell sources; and iii) the routine
application of the analysis. The third point should be favoured by the current availability of portable Raman spectrometers that can automatically scan and analyse complex samples, which
could bring Raman analysis easily in the reach of most laboratories. RS is much more suitable for achieving these goals than the widely used techniques of immunoblotting, cytofluorimetry and
spectrometry because it can provide reproducible results quickly and in a label-free manner, and only requires tiny sample volumes in comparison with the large amounts needed by other
methods, which cannot easily cope with the nanoscalar dimensions of exosomes. This study provides the first Raman-based characterisation of the EVs of human MSCs isolated from bone-marrow
(bone marrow mesenchymal stromal cells, BM-MSCs) and subcutaneous adipose tissue (adipose tissue mesenchymal stromal cells, ASCs). The results were compared with those obtained using EVs
released by dermal fibroblasts (DFs), in order to verify the ability of Raman analysis to distinguish vesicles from undifferentiated and differentiated cells, and gain insights into the
biochemical features of EVs from different sources. Multivariate analysis was used to assess spectral differences and automatically distinguish the three groups. In addition, given the
growing body of evidence concerning the pivotal role of lipids in mediating EV functions42, we also evaluated the contribution of lipid membrane constituents to the Raman spectra. Our
findings provide evidence supporting the use of RS for the routine characterisation of MSC-derived EVs before their _in vitro/in vivo_ application. RESULTS EV CHARACTERISATION EVs were
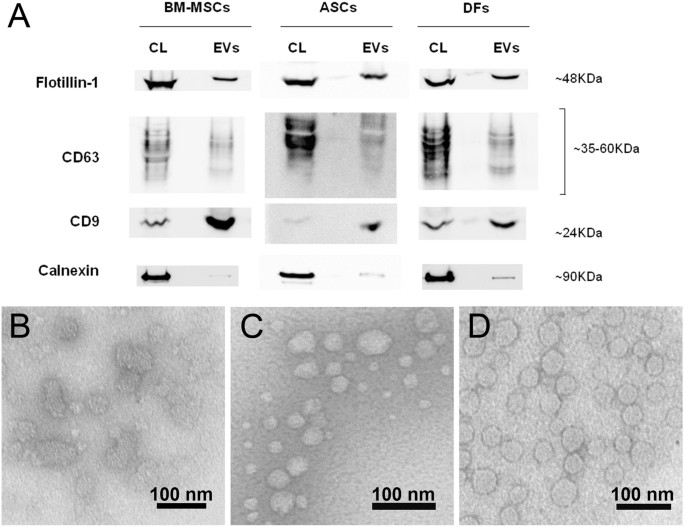
isolated from BM-MSCs, ASCs and DFs following a multi-step ultracentrifugation protocol43 and characterised by immunoblotting and transmission electron microscopy (TEM) to verify their
peculiar features as suggested by the International Society for Extracellular Vesicles (ISEV)44. Immunoblotting confirmed the presence of EVs carrying flotillin-1, CD63 and CD9, and a
significant reduction in calnexin-positive vesicles (Fig. 1A). The TEM images (Fig. 1B–D) confirmed the typical morphology of the EVs, whose ultrastructure and size were consistent with
published data45. The vesicles in all of the samples were round (Fig. 1B–D) and their general mean diameter as calculated on the TEM images was 46.5 nm (±15.8 nm) with slight differences
among cell groups. Supplementary Figure S1 shows a box plot with all of the recorded measurements. RAMAN SPECTROSCOPY BIOCHEMICAL OVERVIEW OF EVS Freshly isolated EVs were analySed by RS in
the spectral ranges of 500–1800 cm−1 and 2600–3200 cm−1, the most significant regions of the Raman spectrum for biological specimens. The spectra were obtained from random spots of air-dried
drops of EV suspension and, given the size of the laser beam, we speculate that every spectrum described the biochemical features of small clusters of aggregated EVs. Figure 2 shows
representative mean Raman spectra (±1 standard deviation) of the vesicles isolated from the supernatants of BM-MSCs, ASCs and DFs. Each mean spectrum represents the average of 40–50
independent recordings obtained from all of the donors of the same cell type. The overall homogeneity in the spectra from the same tissue source underlines the reproducibility of the
analytical method, which is not affected by the intrinsic inter-individual variability of donors. The spectra showed characteristic Raman bands of nucleic acids (NAs, 720–820 cm−1),
phenylalanine (Phe, 1003 cm−1), lipid and protein markers such as CH and CH2 groups (bands respectively centred at 1450 cm−1 and 2940 cm−1) (Fig. 2 and Table 1). In particular, lipids made a
large contribution, which is in line with previously reported spectroscopic evidence40, 41, 46. Lipid content was characterised by peaks attributable to cholesterol and cholesterol ester
(537; 702; 1130; 1442 cm−1) and peaks of varying intensity corresponding to the C-C stretch (around 1100 cm−1) and CH, CH2, and CH3 bonds (in the spectral range 2600–3200 cm−1). In addition,
the areas usually assigned to NA bases (718; 748; 782 cm−1) and phosphate backbone (785; ~1060 cm−1) were variably prominent in the three average spectra. This is in line with many data
demonstrating that EVs contain intact mRNA, long non-coding RNA, miRNA and other forms of RNA loaded into EVs42. The recurrent peaks attributable to proline/hydroxyproline (853; 920; 1206
cm−1) and tryptophan (752–760; 1208; 1360; 1555 cm−1) may be related to differences in cell metabolism and responses to serum-deprived culture conditions. Proline is known to be a signalling
molecule and a sensor of cellular energy status when responding to metabolic stress47, and the kynurenine pathway of tryptophan has been reported as being involved in the immunosuppressive
effects of MSCs48. Comparison of the average spectra revealed many differences between the cytotypes (highlighted in bold characters in Table 1), suggesting discrepancies in the panel of
protein biomarkers and lipid content of vesicles, although it is difficult to attribute divergences in peak intensity to specific molecules. The presence of a 1127 cm−1 peak seemed to
distinguish ASC spectra from those of both BM-MSC and DF EVs. The comparison of ASC and DF data highlighted minor divergences in the spectral range 2600–3200 cm−1, which is greatly
influenced by lipid molecules thus indicating similarities in the lipid content of ASC- and DF-derived vesicles. LIPID MEMBRANE CONSTITUENTS ACCOUNT FOR SPECTRAL DIFFERENCES Principal
Component Analysis (PCA) was used to simplify the original data (n = 198) and all of the spectra were collectively represented by their principal components (PCs). Starting from PC1 (which
accounted for 37.1% of total variance), the subsequent PCs describe differences in the Raman fingerprint that were progressively less prominent (Supplementary Table S1 and Supplementary Fig.
S2). The first 2 PCs (Fig. 3A) were used to build the scatter plot shown in Fig. 3B. Combined analysis of the scatter plot and the PC1 and PC2 spectra revealed that the positive loadings in
the PC1 spectrum mainly describe the biochemical features of ASC-derived EVs, positive peaks in PC2 represent BM-MSC vesicles rather than ASC or DF vesicles. One-way ANOVA performed on PC1
and PC2 scores demonstrated that the means of each group were significantly different (Prob > F < 0.05), despite within-group variance (Supplementary Table S2). Based on the simple
premise that a spectrum from a mixture of chemical ingredients is a mixture of the spectra from the pure ingredients, the PC1 and PC2 loadings were least squares fitted (classical least
square (CLS) fitting) with specific reference spectra to investigate one possible cause of the observed spectral differences, following a previously reported procedure40. As we observed that
the most variable spectral intervals in PC1 and PC2 were related to lipids, the membrane components cholesterol (Chol), ceramide (Cer), sphingomyelin (SM), phosphatidylcholine (PCh),
phosphatidylethanolamine (PE), phosphatidic acid (PA), and monosialotetrahexosylganglioside (GM1, reference molecule for monosialoganglioside family) were used for CLS fitting. Lipid
reference molecules were preferred to protein markers because proteins spectra are dominated by backbone conformation signals, whereas lipids have more specific and defined peaks and can be
more easily distinguished by RS. The resulting CLS fitting scores reported in Table 2 described the relative contribution of each standard molecule to PC1 and PC2 loadings, thus their
contribution to the observed spectral differences between the three cytotypes. Figure 3C depicts the fitting coefficients in a bar graph, making apparent that SM and ganglioside (GM1)
contribute to the shape of PC1 and PC2 loadings more than the other reference molecules. Similarly, PCh is the phospholipid which contributed most to fit the shape of PC1. In particular, the
positive score attributed to SM after PC1 fitting demonstrated that it made a contribution to the spectrum of ASC-derived EVs, and this was further underlined by the negative SM score after
PC2 fitting. On the contrary, GM1 and PCh were assigned a negative CLS fitting score in the case of PC1, suggesting their presence within the membrane of EVs from BM-MSCs and DFs rather
than ASC-derived vesicles. After CLS fitting, the scores assigned to Chol, Cer, PE, and PA suggest their presence in the EVs from all three source cells, although they do not greatly
contribute to the differences between EVs. It has to be noted that the considered lipids are only few of the constituents of vesicles, for this reason our results should be considered as
hints for future studies aimed at verifying the exact membrane composition of vesicles. RAMAN SPECTROSCOPY CAN DISTINGUISH BM-MSC, ASC AND DF EVS WITH 93.7% ACCURACY The first 25 PCs were
used for Linear Discriminant Analysis (LDA), which made possible to verify the ability of the method to identify between-group differences by maximising the variance among classes while
minimising intra-class variability. The results showed that RS clearly distinguished the biochemical fingerprints of the three groups. After leave-one-out cross-validation, the PCA-LDA model
showed that the overall accuracy of the model was 93.7% and that its accuracy in distinguishing DFs from MSCs was 92% (Table 3). The LDA scatter plot (Fig. 4) revealed that the spectra of
the ASC-derived EVs fell into a region that was clearly separated from those of the BM-MSC EVs. Although there was a limited overlap between the DF and ASC derived vesicles, RS distinguished
their sources with a high degree of statistical confidence (Wilks’ Lambda Test, p < 0.001). Details concerning the distribution of the individual donor spectra are shown in Supplementary
Figure S3. DISCUSSION The possibility of using regenerative medicine to treat diseased, damaged or aged tissues and restore organ function without side effects is one of the main challenges
facing modern medical science, and so is no surprise that the discovery of the regenerative potential of EVs released by MSCs has aroused great interest. However, the main obstacle to the
clinical use of vesicles is the lack of a robust and standardised method of characterising them5. In this study, we investigated the biochemical fingerprints of MSC-derived vesicles
originating from different tissues and compared them with those of terminally differentiated dermal fibroblasts. Our findings demonstrate the ability of RS to identify tissue-related
fingerprints for vesicles released by MSCs and fibroblasts without the use of any label. This is the first time that Raman analysis has been used to provide a biochemical overview of
MSC-derived EVs from a limited volume of EV suspensions. As previously reported in relation to other types of vesicles40, 41, 49, our data on MSC-derived EVs confirm the ability of RS to
reveal the presence of the main EV constituents in a single repeatable spectrum. Although we cannot exclude the possible presence of a limited amount of soluble factors other than vesicles
in our suspension, the reproducibility of the results and the main peak attributions suggest the purity of the samples. The main finding of this study is that RS can clearly distinguish not
only vesicles from MSCs and terminally differentiated fibroblasts, but also vesicles of MSCs from bone marrow and adipose tissue. Although there are protein markers that define a stem cell
phenotype exist, a straightforward distinction between bone-marrow and adipose-tissue MSCs, based on biological and functional features, is still difficult to be obtained50. The ability of
RS to highlight unique, tissue-specific features of vesicles should therefore assist scientists working with stem cells. Even if assessing the possible correlation between biochemistry and
function goes beyond the scope of this study, the biochemical variations observed provide suggestions for further investigations into the functional differences of EVs from multiple MSC
types and sources for which there is still not a definite marker51, 52. Analysis of the spectra of MSC- and DF-derived EVs revealed that lipids made a substantial contribution to the Raman
signals, as previously reported40, 41, 49. The prominence of membrane constituents in determining the fingerprints of vesicles is in line with the growing body of evidence demonstrating that
lipids play a crucial role in the formation of EVs1 and the fulfilment of their signalling functions42. It is known that a number of specific lipids are typically associated with lipid
rafts and enriched in vesicles that inherit the plasma membrane composition of their cell of origin. In particular, cholesterol and sphingolipids are preferentially included in EV membranes
and may be involved in the formation of vesicles and in their stability in the extracellular environment42. There is also evidence that lipids are involved in BM-MSC responses to a strongly
pro-inflammatory environment53. Furthermore, it is possible that direct membrane interactions between vesicles and recipient cells is one of the mechanisms of action of EVs, as has already
been demonstrated in the case of whole cells2. On the basis of CLS fitting results, we hypothesised that gangliosides, phosphatidylcholine and sphingomyelin directly contributed to the main
spectral differences between the considered EVs. Our data are in agreement with those of a recent proteomic and lipidomic study demonstrating how sphingomyelins, ceramides, cholesterol and
phosphatidylcoline were enriched in the exosomes of BM-MSCs in comparison with other cell types54, but there is still a lack of data concerning the membrane composition of ASC-derived
exosomes. Our observation that GM1 also contributes to the recorded spectra of BM-MSC vesicles is in line with the reported functional role of gangliosides in regulating the proliferation
and neuronal differentiation of MSCs55, 56. Similarly, it is known that ceramides and ceramide-containing lipids are involved in many of the pathways mediating immune responses, and that
they modulate the adipogenic differentiation of MSCs57. Despite the reported functional significance of PA in the biogenesis and release of exosomes, our data did not reveal any significant
difference of PA content in the EVs derived from the three cell types, as has also been noticed by Haraszti _et al_.54 Further lipidomic studies are needed to verify the exact membrane
composition of MSC-derived vesicles and to establish the role of lipid species in mediating vesicle function. It is important to mention one limitation of our study related to the sex
mismatch of our MSC donors. It is known that MSC activity and recipient responses are influenced by the sex of both donor and recipient because of circulating hormones58, but, to the best of
our knowledge, no specific study has been published concerning sex-related variations in the function of EVs derived from cultured cells. Studies evaluating the efficacy of MSC-derived EVs
_in vitro_ and _in vivo_ rarely refer to the sex of the donors, but this is very useful and should be always clearly indicated together with donor age59. Future in-depth analyses of larger
donor cohorts should evaluate age and sex-related differences in EV function and chemical composition. In conclusion, our findings demonstrate that RS can determine the chemical content of
EVs in a label- and sample processing- free manner. The proposed method can be immediately transferred into laboratory practice as it allows the bulk characterisation of vesicle suspensions
before their use _in vitro_ or _in vivo_. As independent MSC-derived EV preparations can have different therapeutic potentials, the overall characterisation of vesicles offered by Raman
spectroscopy might become a pivotal quality check for comparing data coming from different experiments or research labs, and thus hasten the clinical application of stem cell-derived
products. METHODS All of the relevant experimental data have been submitted to the EV-TRACK knowledgebase (EV-TRACK ID: EV170012)60. CELL CULTURES Human BM-MSCs were isolated from the
residual bone marrow cells of healthy bone marrow (BM) transplantation donors (3 male donors, age range: 17–20 y/o) after approval by the Institutional Review Board of San Raffaele Hospital.
Human ASCs and DFs were isolated from waste materials of abdominoplasty and liposuction procedures performed at IRCCS Galeazzi Orthopaedic Institute (subcutaneous adipose tissue of 4 female
healthy donors - age range: 35–58 y/o - and de-epidermised dermis of 3 female healthy donors – age range: 26–46 y/o-, respectively). Tissues were collected following the procedure PQ
7.5.125 regarding waste materials to be used for research purposes, version 4 dated 22.01.2015, approved by the same institute. Written informed consent was obtained from all of the patients
in accordance with the ethical principles of the Declaration of Helsinki. All of the samples were anonymised and no information or images that could lead to identification of a study
participant might occur. All experiments were performed in accordance with the relevant guidelines and regulations of San Raffaele Hospital and IRCCS Galeazzi Orthopaedic Institute. Cells
were isolated following previously described protocols61,62,63. Briefly, mononuclear cells from BM aspirates were isolated by means of density gradient centrifugation (Ficoll 1.077 g/ml;
Lympholyte, Cedarlane Laboratories Ltd., Burlington, Canada) and plated in non-coated 75–150 cm2 tissue culture flasks (BD Falcon, Franklin Lakes, NJ, USA) at a density of 160,000/cm2 in
complete culture medium: DMEM (Euroclone, Milan, Italy) supplemented with 10% ultracentrifuged foetal bovine serum (Gibco, Life Technologies LTD, Paisley, UK), penicillin 50 U/ml, 50 µg/ml
streptomycin and 2 mM L-glutamine (L-Glu, Euroclone). Cultures were maintained at 37 °C in a humidified atmosphere, containing 5% CO2. After 48-hour culture, non-adherent cells were removed.
The ASCs were isolated from adipose tissue samples following digestion with 0.75 mg/ml type I Collagenase (250 U/mg, Worthington Biochemical Corporation, Lakewood, NJ, USA) and the
filtering of the stromal vascular fraction. The DFs were obtained from de-epidermised dermis fragmented and digested with 0.1% collagenase type I. The ASCs and DFs (plating density: 105
cells/cm2) were cultured (37 °C, 5% CO2) in complete culture medium. The medium was replaced every other day and, at 70–80% confluence, the cells were detached with 0.5% trypsin/0.2% EDTA,
plated (BM-MSC plating density 4,000 cells/cm2; ASC plating density 10,000 cells/cm2; DF plating density 5,000 cells/cm2) and expanded. Once at 80–90% confluence, cells at 3rd–4th passage
were washed twice with DMEM, kept for one hour in serum-free DMEM (phenol-free DMEM supplemented with 2 mM L-glutamine, 50U/ml penicillin, 50 µg/ml streptomycin) and then cultured for 72
hours in serum-free DMEM. EXTRACELLULAR VESICLE ISOLATION In order to avoid the presence of RS-visible isolation reagent residues in the EV suspension, the vesicles were isolated from
cell-conditioned medium (CM) by means of differential centrifugation, as previously described43. Briefly, after 72 hours of starvation, the medium conditioned from approximately 6 × 106
cells was centrifuged at 800 g for 10 min to remove non-adherent cells and then at 2,500 g for 15 min to remove potential apoptotic bodies. CM was then ultracentrifuged for 70 min at 100,000
g (L7–65; Rotor 55.2 Ti; Beckman Coulter, Brea, CA, USA) at 4 °C, and the pellet was re-suspended in sterile saline solution and ultracentrifuged again. The collected EV suspension
(approximately 500 µl) was kept at 4 °C before making Raman and TEM analyses, and then frozen. WESTERN BLOTTING Immunoblotting was performed to characterise the EVs as suggested by ISEV
minimal experimental requirements44. The EV pellets were re-suspended in SDS sample buffer with protease inhibitors64. Electrophoresis was performed under reducing conditions, and then
proteins were transferred to nitrocellulose membrane. The antigens were probed with anti-flotillin-1 (BD Transduction Laboratories™, San Jose, CA, USA), anti-CD63 and anti-CD9 (System
Biosciences, Palo Alto, CA, USA), and anti-calnexin (endoplasmic reticulum protein used as negative control, clone C5C9, Cell Signaling Technology, Danvers, MA, USA). As secondary antibodies
goat anti-mouse (Thermo Fisher Scientific, Waltham, MA, USA) and goat anti-rabbit (System Biosciences) conjugated with HRP were used. Cell lysates were considered as the control for the
specificity and working conditions of the considered antibodies. TRANSMISSION ELECTRON MICROSCOPY AND SIZE MEASUREMENT For the TEM visualisation of EVs, 5 µl of purified exosomes were
absorbed on Formvar carbon-coated grids for 10 min. The drops were then blotted with filter paper and negatively stained with 2% uranyl acetate (5 μl) in aqueous suspension for 10 min.
Excess of uranyl was removed by touching the grid to a filter paper. The grids were dried at room temperature and examined with a transmission electron microscope (Leo 812AB, Zeiss,
Oberkochen, Germany) at 80 kV. The TEM images obtained in order to verify EV ultrastructure were used to assess vesicles’ size using the particle analysis tool of ImageJ software (National
Institutes of Health, Bethesda, MD, USA). At least 30 measurements per sample were done. RAMAN SPECTROSCOPY Freshly isolated EVs were analysed by means of Raman microspectroscopy (LabRAM
Aramis, Horiba Jobin Yvon S.A.S, Lille, France) equipped with a diode-pumped solid-state laser operating at 532 nm and a Peltier-cooled CCD detector. 5–10 µl drops of EV suspension were
deposited on a calcium fluoride slide and allowed to air dry. All of the measurementS were performed with 50× objective (NA 0.75, Olympus, Tokyo, Japan), 1800 grooves/mm diffraction grating,
400 µm entrance slit, and confocal mode (600 µm pinhole) in the spectral ranges 500–1800 cm−1 and 2600–3200 cm−1. Accumulation times were 2 × 10 s per spectrum. The Raman shift was
calibrated automatically using LabSpec 6 software (Horiba) using zero order line and Si line of a Si reference sample. In order to capture the spectra randomly, maps of about 150 µm2 (with
lateral steps of 20–30 µm) were acquired in the centre and at the borders of the air-dried drops. Before analysing the data, a two-class hierarchical clustering analysis (HCA) of the Raman
maps was made in order to distinguish the spectra relating to vesicles from those related to background. At least 10 independent replicates of the Raman spectra were obtained for every donor
of the different cell types. DATA ANALYSIS Baseline correction was made using LabSpec 6 processing tool by fitting all spectra with a sixth order polynomial curve in order to remove
autofluorescence and background before unit vector normalisation. Post-acquisition calibration was carried out on normalised spectra, in order to compensate for possible thermal drifts.
Principal component analysis (PCA) of the normalised and aligned spectra was made in order to reduce the dimension of the data and describe their major trends. The provided principal
components (PCs) represent differences in the spectra of vesicles from the three cytotypes and therefore in their chemical composition. The first 25 PC scores were used in a supervised
classification model, linear discriminant analysis (LDA), in order to discriminate and classify the data by maximizing the variance between groups. Data reduction by PCA before LDA was
essential because LDA requires that the number of variables is smaller than the number of observations. The smallest number of PC scores was selected for the LDA to prevent data overfitting.
A decreased number of PCs reduced the accuracy of the method in distinguishing the EVs, whereas an increased number did not improve the classification, but progressively decreased accuracy.
Leave-one-out cross-validation was used to test the classification sensitivity, specificity, and accuracy of the LDA model. One-way ANOVA was performed on PC scores to verify that the means
of each group were significantly different, despite within-group variance. Data manipulations and statistical analysis were performed using Origin2017 (v. 9.4, OriginLab, Northampton, MA,
USA). CLS FITTING Reference molecules of some of the major known constituents of EV membrane were used to investigate the lipid content of vesicles. Cholesterol (Chol), ceramide
(N-stearoyl-D-erythro-sphingosine; Cer), sphingomyelin (SM), phosphatidylcholine (16:0/22:6; PCh), L-α-phosphatidylethanolamine (PE), phosphatidic acid (PA), and
monosialotetrahexosylganglioside (GM1) were purchased from Avanti Polar Lipids (Alabaster, AL, USA) and used to acquire reference spectra using the same acquisition settings as those used
for the EV analysis. Labspec 6 was used for the Classical Least-Squares (CLS) fitting of the PC1 and PC2 spectra, which allows to calculate the contribution of the reference chemicals to the
PC spectra by evaluating any similarities. The resulting coefficients described the relationships between the PC spectra and the reference molecules. DATA AVAILABILITY The datasets
generated and analysed during the current study are available from the corresponding author on reasonable request. REFERENCES * Raposo, G. & Stoorvogel, W. Extracellular vesicles:
exosomes, microvesicles, and friends. _Journal of Cell Biology_ 200, 373–383, doi:10.1083/jcb.201211138 (2013). Article CAS PubMed PubMed Central Google Scholar * Xie, Y. C. _et al_.
Importance of cell-cell contact in the therapeutic benefits of cardiosphere-derived cells. _Stem Cells_ 32, 2397–2406, doi:10.1002/stem.1736 (2014). Article PubMed PubMed Central Google
Scholar * Teixeira, J. H., Silva, A. M., Almeida, M. I., Barbosa, M. A. & Santos, S. G. Circulating extracellular vesicles: Their role in tissue repair and regeneration. _Transfusion
and Apheresis Science_ 55, 53–61, doi:10.1016/j.transci.2016.07.015 (2016). Article PubMed Google Scholar * Nurkovic, J., Grbovic, V., Nurkovic, S., Vucelj, S. & Dolicanin, Z.
Adipose-derived human mesenchymal stem cells can produce cartilage. _Osteoporosis International_ 27, S116–S116 (2016). Google Scholar * Akyurekli, C. _et al_. A systematic review of
preclinical studies on the therapeutic potential of mesenchymal stromal cell-derived microvesicles. _Stem Cell Reviews and Reports_ 11, 150–160, doi:10.1007/s12015-014-9545-9 (2015). Article
CAS PubMed Google Scholar * Phinney, D. G. & Pittenger, M. F. Concise review: MSC-derived exosomes for cell-free therapy. _Stem Cells_ 35, 851–858, doi:10.1002/stem.2575 (2017).
Article CAS PubMed Google Scholar * Kordelas, L. _et al_. MSC-derived exosomes: a novel tool to treat therapy-refractory graft-versus-host disease. _Leukemia_ 28, 970–973,
doi:10.1038/leu.2014.41 (2014). CAS PubMed Google Scholar * Arslan, F. _et al_. Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate PI3K/Akt
pathway to enhance myocardial viability and prevent adverse remodeling after myocardial ischemia/reperfusion injury. _Stem Cell Research_ 10, 301–312, doi:10.1016/j.scr.2013.01.002 (2013).
Article CAS PubMed Google Scholar * Lai, R. C. _et al_. Exosome secreted by MSC reduces myocardial ischemia/reperfusion injury. _Stem Cell Research_ 4, 214–222,
doi:10.1016/j.scr.2009.12.003 (2010). Article CAS PubMed Google Scholar * Suzuki, E., Fujita, D., Takahashi, M., Oba, S. & Nishimatsu, H. Adipose tissue-derived stem cells as a
therapeutic tool for cardiovascular disease. _World Journal of Cardiology_ 7, 454–465, doi:10.4330/wjc.v7.i8.454 (2015). Article PubMed PubMed Central Google Scholar * Zhou, Y. _et al_.
Exosomes released by human umbilical cord mesenchymal stem cells protect against cisplatin-induced renal oxidative stress and apoptosis _in vivo_ and _in vitro_. _Stem Cell Research &
Therapy_ 4, doi:10.1186/scrt194 (2013). * Eirin, A. _et al_. Mesenchymal stem cell-derived extracellular vesicles attenuate kidney inflammation. _Kidney international_,
doi:10.1016/j.kint.2016.12.023 (2017). * Ranghino, A. _et al_. The effects of glomerular and tubular renal progenitors and derived extracellular vesicles on recovery from acute kidney
injury. _Stem cell research & therapy_ 8, 24–24, doi:10.1186/s13287-017-0478-5 (2017). Article Google Scholar * Li, T. F. _et al_. Exosomes Derived from human umbilical cord
mesenchymal stem cells alleviate liver fibrosis. _Stem Cells and Development_ 22, 845–854, doi:10.1089/scd.2012.0395 (2013). Article ADS CAS PubMed Google Scholar * Haga, H., Yan, I.
K., Takahashi, K., Matsuda, A. & Patel, T. Extracellular vesicles from bone marrow-derived mesenchymal stem cells improve survival from lethal hepatic failure in mice. _Stem cells
translational medicine_, doi:10.1002/sctm.16-0226 (2017). * Narayanan, R., Huang, C. C. & Ravindran, S. Hijacking the cellular mail: exosome mediated differentiation of mesenchymal stem
cells. _Stem Cells International_, doi:10.1155/2016/3808674 (2016). * Toh, W. S., Lai, R. C., Hui, J. H. P. & Lim, S. K. MSC exosome as a cell-free MSC therapy for cartilage
regeneration: Implications for osteoarthritis treatment. _Seminars in cell & developmental biology_, doi:10.1016/j.semcdb.2016.11.008 (2016). * Nakamura, Y. _et al_.
Mesenchymal-stem-cell-derived exosomes accelerate skeletal muscle regeneration. _Febs Letters_ 589, 1257–1265, doi:10.1016/j.febslet.2015.03.031 (2015). Article CAS PubMed Google Scholar
* Hu, L. _et al_. Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. _Scientific Reports_ 6,
doi:10.1038/srep32993 (2016). * Zhang, Y. L. _et al_. Effect of exosomes derived from multipluripotent mesenchyrnal stromal cells on functional recovery and neurovascular plasticity in rats
after traumatic brain injury. _Journal of Neurosurgery_ 122, 856–867, doi:10.3171/2014.11.jns14770 (2015). Article CAS PubMed PubMed Central Google Scholar * Katsuda, T. _et al_. Human
adipose tissue-derived mesenchymal stem cells secrete functional neprilysin-bound exosomes. _Scientific Reports_ 3, doi:10.1038/srep01197 (2013). * Hu, B. _et al_. Effect of extracellular
vesicles on neural functional recovery and immunologic suppression after rat cerebral apoplexy. _Cellular Physiology and Biochemistry_ 40, 155–162, doi:10.1159/000452533 (2016). Article CAS
PubMed Google Scholar * Otero-Ortega, L. _et al_. White Matter Repair After Extracellular vesicles administration in an experimental animal model of subcortical stroke. _Scientific
reports_ 7, 44433–44433, doi:10.1038/srep44433 (2017). Article ADS CAS PubMed PubMed Central Google Scholar * Marote, A., Teixeira, F. G., Mendes-Pinheiro, B. & Salgado, A. J.
MSCs-derived exosomes: cell-secreted nanovesicles with regenerative potential. _Frontiers in Pharmacology_ 7, doi:10.3389/fphar2016.00231 (2016). * De Jong, O. G., Van Balkom, B. W. M.,
Schiffelere, R. M., Bouten, C. V. C. & Verhaar, M. C. Extracellular vesicles: potential roles in regenerative medicine. _Frontiers in Immunology_ 5, 1–13, doi:10.3389/fimmu.2014.00608
(2014). Google Scholar * Lener, T. _et al_. Applying extracellular vesicles based therapeutics in clinical trials - an ISEV position paper. _Journal of Extracellular Vesicles_ 4,
doi:10.3402/jev.v4.30087 (2015). * Wachsmann-Hogiu, S., Weeks, T. & Huser, T. Chemical analysis _in vivo_ and _in vitro_ by Raman spectroscopy-from single cells to humans. _Current
Opinion in Biotechnology_ 20, 63–73, doi:10.1016/j.copbio.2009.02.006 (2009). Article CAS PubMed PubMed Central Google Scholar * Smith, Z. J., Huser, T. R. & Wachsmann-Hogiu, S.
Raman scattering in pathology. _Analytical Cellular Pathology_ 35, 145–163, doi:10.3233/acp-2011-0048 (2012). Article CAS Google Scholar * Krafft, C. & Popp, J. The many facets of
Raman spectroscopy for biomedical analysis. _Analytical and Bioanalytical Chemistry_ 407, 699–717, doi:10.1007/s00216-014-8311-9 (2015). Article CAS PubMed Google Scholar * Moura, C. C.,
Tare, R. S., Oreffo, R. O. C. & Mahajan, S. Raman spectroscopy and coherent anti-Stokes Raman scattering imaging: prospective tools for monitoring skeletal cells and skeletal
regeneration. _Journal of the Royal Society Interface_ 13, doi:10.1098/rsif.2016.0182 (2016). * Wu, Y. _et al_. Evaluation of the Bone-ligament and tendon insertions based on Raman spectrum
and its PCA and CLS analysis. _Sci Rep_ 7, 38706, doi:10.1038/srep38706 (2017). Article ADS CAS PubMed PubMed Central Google Scholar * Vanna, R. _et al_. Label-free imaging and
identification of typical cells of acute myeloid leukaemia and myelodysplastic syndrome by Raman microspectroscopy. _Analyst_ 140, 1054–1064, doi:10.1039/c4an02127d (2015). Article ADS CAS
PubMed Google Scholar * Lui, H., Zhao, J. H., McLean, D. & Zeng, H. S. Real-time Raman spectroscopy for _in vivo_ skin cancer diagnosis. _Cancer Research_ 72, 2491–2500,
doi:10.1158/0008-5472.can-11-4061 (2012). Article CAS PubMed Google Scholar * Santos, I. P. _et al_. Raman spectroscopic characterization of melanoma and benign melanocytic lesions
suspected of melanoma using high-wavenumber raman spectroscopy. _Analytical Chemistry_ 88, 7683–7688, doi:10.1021/acs.analchem.6b01592 (2016). Article CAS PubMed Google Scholar *
Notingher, I. _et al_. _In situ_ spectral monitoring of mRNA translation in embryonic stem cells during differentiation _in vitro_. _Analytical Chemistry_ 76, 3185–3193,
doi:10.1021/ac0498720 (2004). Article CAS PubMed Google Scholar * Chan, J. W., Lieu, D. K., Huser, T. & Li, R. A. Label-free separation of human embryonic stem cells and their
cardiac derivatives using raman spectroscopy. _Analytical Chemistry_ 81, 1324–1331, doi:10.1021/ac801665m (2009). Article CAS PubMed PubMed Central Google Scholar * Downes, A., Mouras,
R., Bagnaninchi, P. & Elfick, A. Raman spectroscopy and CARS microscopy of stem cells and their derivatives. _Journal of Raman Spectroscopy_ 42, 1864–1870, doi:10.1002/jrs.2975 (2011).
Article ADS CAS PubMed PubMed Central Google Scholar * Azrad, E. _et al_. Probing the effect of an extract of elk velvet antler powder on mesenchymal stem cells using Raman
microspectroscopy: enhanced differentiation toward osteogenic fate. _Journal of Raman Spectroscopy_ 37, 480–486, doi:10.1002/jrs.1420 (2006). Article ADS CAS Google Scholar * McManus, L.
L. _et al_. Raman spectroscopic monitoring of the osteogenic differentiation of human mesenchymal stem cells. _Analyst_ 136, 2471–2481, doi:10.1039/c1an15167c (2011). Article ADS CAS
PubMed Google Scholar * Smith, Z. J. _et al_. Single exosome study reveals subpopulations distributed among cell lines with variability related to membrane content. _Journal of
Extracellular Vesicles_ 4, doi:10.3402/jev.v4.28533 (2015). * Krafft, C. _et al_. A specific spectral signature of serum and plasma-derived extracellular vesicles for cancer screening.
_Nanomedicine_, doi:10.1016/j.nano.2016.11.016 (2016). * Yanez-Mo, M. _et al_. Biological properties of extracellular vesicles and their physiological functions. _Journal of Extracellular
Vesicles_ 4, doi:10.3402/jev.v4.27066 (2015). * Thery, C., Amigorena, S., Raposo, G. & Clayton, A. Isolation and characterization of exosomes from cell culture supernatants and
biological fluids. _Current protocols in cell biology_ Chapter 3, Unit 3.22-Unit 23.22, doi:10.1002/0471143030.cb0322s30 (2006). * Lotvall, J. _et al_. Minimal experimental requirements for
definition of extracellular vesicles and their functions: a position statement from the International Society for Extracellular Vesicles. _Journal of extracellular vesicles_ 3, 26913–26913,
doi:10.3402/jev.v3.26913 (2014). Article PubMed Google Scholar * Colombo, M., Raposo, G. & Thery, C. Biogenesis, secretion, and intercellular interactions of exosomes and other
extracellular vesicles. _Annual Review of Cell and Developmental Biology, Vol 30_ 30, 255–289, doi:10.1146/annurev-cellbio-101512-122326 (2014). Article CAS Google Scholar * Lavialle, F.
_et al_. Nanovesicles released by Dictyostelium cells: a potential carrier for drug delivery. _International Journal of Pharmaceutics_ 380, 206–215, doi:10.1016/j.ijpharm.2009.06.039 (2009).
Article CAS PubMed Google Scholar * Phang, J. M., Liu, W. & Zabirnyk, O. _Proline metabolism and microenvironmental stress. Annual Review of Nutrition, Vol 30_ 30, 441–463,
doi:10.1146/annurev.nutr.012809.104638 (2010). CAS Google Scholar * Jones, S. P., Guillemin, G. J. & Brew, B. J. The kynurenine pathway in stem cell biology. _International journal of
tryptophan researc: IJTR_ 6, 57–66, doi:10.4137/ijtr.s12626 (2013). Article CAS Google Scholar * Tatischeff, I., Larquet, E., Falcon-Perez, J. M., Turpin, P.-Y. & Kruglik, S. G. Fast
characterisation of cell-derived extracellular vesicles by nanoparticles tracking analysis, cryo-electron microscopy, and Raman tweezers microspectroscopy. _Journal of extracellular
vesicles_ 1, doi:10.3402/jev.v1i0.19179 (2012). * Dominici, M. _et al_. Minimal criteria for defining multipotent mesenchymal stromal cells. The International Society for Cellular Therapy
position statement. _Cytotherapy_ 8, 315–317, doi:10.1080/14653240600855905 (2006). Article CAS PubMed Google Scholar * Collins, E. _et al_. Differential Efficacy of Human Mesenchymal
Stem Cells Based on Source of Origin. _Journal of Immunology_ 193, 4381–4390, doi:10.4049/jimmunol.1401636 (2014). Article CAS Google Scholar * Rasmussen, J. G. _et al_. Comparison of
human adipose-derived stem cells and bone marrow-derived stem cells in a myocardial infarction model. _Cell Transplantation_ 23, 195–206, doi:10.3727/096368912x659871 (2014). Article PubMed
Google Scholar * Campos, A. M. _et al_. Lipidomics of mesenchymal stromal cells: understanding the adaptation of phospholipid profile in response to pro-inflammatory cytokines. _Journal
of Cellular Physiology_ 231, 1024–1032, doi:10.1002/jcp.25191 (2016). Article CAS PubMed Google Scholar * Haraszti, R. A. _et al_. High-resolution proteomic and lipidomic analysis of
exosomes and microvesicles from different cell sources. _Journal of Extracellular Vesicles_ 5, doi:10.3402/jev.v5.32570 (2016). * Freund, D., Fonseca, A. V., Janich, P., Bornhauser, M. &
Corbeil, D. Differential expression of biofunctional GM1 and GM3 gangliosides within the plastic-adherent multipotent mesenchymal stromal cell population. _Cytotherapy_ 12, 131–142,
doi:10.3109/14653240903476438 (2010). Article CAS PubMed Google Scholar * Moussavou, G. _et al_. Role of gangliosides in the differentiation of human mesenchymal-derived stem cells into
osteoblasts and neuronal cells. _Bmb Reports_ 46, 527–532, doi:10.5483/BMBRep.2013.46.11.179 (2013). Article CAS PubMed PubMed Central Google Scholar * Xu, F., Yang, C. C., Gomillion,
C. & Burg, K. J. L. Effect of ceramide on mesenchymal stem cell differentiation toward adipocytes. _Applied Biochemistry and Biotechnology_ 160, 197–212, doi:10.1007/s12010-008-8505-8
(2010). Article CAS PubMed Google Scholar * Sammour, I. _et al_. The effect of gender on mesenchymal stem cell (MSC) efficacy in neonatal hyperoxia-induced lung injury. _Plos One_ 11,
10, doi:10.1371/journal.pone.0164269 (2016). Article Google Scholar * Shah, K., McCormack, C. E. & Bradbury, N. A. Do you know the sex of your cells? _American Journal of Physiology_
306, C3–C18, doi:10.1152/ajpcell.00281.2013 (2014). Article CAS PubMed Google Scholar * Van Deun, J. _et al_. EV-TRACK: transparent reporting and centralizing knowledge in extracellular
vesicle research. _Nature methods_ 14, 228–32, doi:10.1038/nmeth.4185 (2017). Article PubMed Google Scholar * Conforti, A. _et al_. Biological, functional and genetic characterization of
bone marrow-derived mesenchymal stromal cells from pediatric patients affected by acute lymphoblastic leukemia. _Plos One_ 8, 11, doi:10.1371/journal.pone.0076989 (2013). Article Google
Scholar * Brini, A. T. _et al_. Effect of an activated platelet concentrate on differentiated cells involved in tissue healing. _Journal of Craniofacial Surgery_ 27, 656–661,
doi:10.1097/scs.0000000000002540 (2016). PubMed Google Scholar * Niada, S. _et al_. 17 beta-estradiol differently affects osteogenic differentiation of mesenchymal stem/stromal cells from
adipose tissue and bone marrow. _Differentiation_ 92, 291–297, doi:10.1016/j.diff.2016.04.001 (2016). Article CAS PubMed Google Scholar * Gabrielli, M. _et al_. Active endocannabinoids
are secreted on extracellular membrane vesicles. _Embo Reports_ 16, 213–220 (2015). Article CAS PubMed PubMed Central Google Scholar * Czamara, K. _et al_. Raman spectroscopy of lipids:
a review. _Journal of Raman Spectroscopy_ 46, 4–20, doi:10.1002/jrs.4607 (2015). Article ADS CAS Google Scholar * Movasaghi, Z., Rehman, S. & Rehman, I. U. Raman spectroscopy of
biological tissues. _Applied Spectroscopy Reviews_ 42, 493–541, doi:10.1080/05704920701551530 (2007). Article ADS CAS Google Scholar * Krafft, C., Neudert, L., Simat, T. & Salzer, R.
Near infrared Raman spectra of human brain lipids. _Spectrochimica Acta Part a-Molecular and Biomolecular Spectroscopy_ 61, 1529–1535, doi:10.1016/j.saa.2004.11.017 (2005). Article ADS
Google Scholar Download references ACKNOWLEDGEMENTS This study was supported by the Italian Ministry of Health (Ricerca Corrente 2015, IRCCS Fondazione Don Carlo Gnocchi ONLUS; Ricerca
Corrente RC L1027, IRCCS Galeazzi Orthopaedic Institute) and by the Department of Biomedical, Surgical and Dental Sciences (University of Milan, grant no. 15-63017000-700). AUTHOR
INFORMATION AUTHORS AND AFFILIATIONS * Laboratory of Nanomedicine and Clinical Biophotonics, IRCCS Fondazione Don Carlo Gnocchi ONLUS, Milano, Italy Alice Gualerzi, Silvia Picciolini, Carlo
Morasso, Renzo Vanna, Marzia Bedoni & Furio Gramatica * Dipartimento di Scienze Biomediche, Chirurgiche ed Odontoiatriche, Università degli Studi di Milano, Milano, Italy Stefania Niada,
Chiara Giannasi & Anna Teresa Brini * Laboratorio di Applicazioni Biotecnologiche, IRCCS Istituto Ortopedico Galeazzi, Milano, Italy Stefania Niada, Chiara Giannasi & Anna Teresa
Brini * Nanomedicine Center NANOMIB, School of Medicine and Surgery, University of Milano-Bicocca, Monza, Italy Silvia Picciolini & Massimo Masserini * San Raffaele Telethon Institute
for Gene Therapy (SR-TIGET), Pediatric Immunohematology, San Raffaele Scientific Institute, Milano, Italy Valeria Rossella & Maria Ester Bernardo * Hematology and Bone Marrow
Transplantation Unit, San Raffaele Scientific Institute, Milano, Italy Fabio Ciceri Authors * Alice Gualerzi View author publications You can also search for this author inPubMed Google
Scholar * Stefania Niada View author publications You can also search for this author inPubMed Google Scholar * Chiara Giannasi View author publications You can also search for this author
inPubMed Google Scholar * Silvia Picciolini View author publications You can also search for this author inPubMed Google Scholar * Carlo Morasso View author publications You can also search
for this author inPubMed Google Scholar * Renzo Vanna View author publications You can also search for this author inPubMed Google Scholar * Valeria Rossella View author publications You can
also search for this author inPubMed Google Scholar * Massimo Masserini View author publications You can also search for this author inPubMed Google Scholar * Marzia Bedoni View author
publications You can also search for this author inPubMed Google Scholar * Fabio Ciceri View author publications You can also search for this author inPubMed Google Scholar * Maria Ester
Bernardo View author publications You can also search for this author inPubMed Google Scholar * Anna Teresa Brini View author publications You can also search for this author inPubMed Google
Scholar * Furio Gramatica View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS A.G. performed Raman experiments; A.G., S.N., G.C. and V.R.
conducted EV isolation and characterisation; A.G., S.P., C.M., R.V., and M.B. analysed and interpreted data; M.M., F.C., F.G., M.E.B. and A.T.B. supervised the work; A.G., C.M., S.P. and
R.V. wrote the original draft manuscript; S.N., G.C., M.E.B., A.T.B., M.M., F.C. and F.G. reviewed and edited the final manuscript. CORRESPONDING AUTHOR Correspondence to Alice Gualerzi.
ETHICS DECLARATIONS COMPETING INTERESTS The authors declare that they have no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard
to jurisdictional claims in published maps and institutional affiliations. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is
licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in
this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative
Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a
copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Gualerzi, A., Niada, S., Giannasi, C. _et al._ Raman
spectroscopy uncovers biochemical tissue-related features of extracellular vesicles from mesenchymal stromal cells. _Sci Rep_ 7, 9820 (2017). https://doi.org/10.1038/s41598-017-10448-1
Download citation * Received: 15 May 2017 * Accepted: 08 August 2017 * Published: 29 August 2017 * DOI: https://doi.org/10.1038/s41598-017-10448-1 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative