Play all audios:
ABSTRACT Hypertension has become a major public health challenge. However, numerous research results reported in the literature focus primarily on risk factors of hypertension, little is
known about how the whole continuum of blood pressure (BP) is associated with risk factors of hypertension. This study aims to reveal quantile-specific associations of BP with its risk
factors. A cross-sectional survey based on a sample of 23,050 adults aged 18 to 79 years was conducted in Jilin Province in 2012, and some subjects were excluded due to missing values in BP
or having BP control according to the purpose of this study. Quantile regression (QR) was employed to investigate the associations between systolic/diastolic blood pressure (SBP/DBP) and the
risk factors. The SBP and DBP in males presented statistically higher than females (_P_ < 0.001). High-salt diet for males manifested a slightly increasing positive association with
higher SBP only for high quantiles (≥70), but with a higher DBP for middle part of the quantiles (30~75), compared with bland diet. High-salt diet, drinking and high-density lipoprotein
cholesterol (HDL-C) were positively associated with BP measures in males. And the coefficient of total cholesterol (TC) in QR increased with BP in females who used to live in town. SIMILAR
CONTENT BEING VIEWED BY OTHERS MIXED EFFECTS LOGISTIC REGRESSION ANALYSIS OF BLOOD PRESSURE AMONG GHANAIANS AND ASSOCIATED RISK FACTORS Article Open access 12 May 2023 HIGH-NORMAL BLOOD
PRESSURE AND RELATED CARDIOVASCULAR RISK FACTORS PREVALENCE IN THE ROMANIAN ADULT POPULATION: INSIGHTS FROM THE SEPHAR III STUDY Article 25 September 2020 ADJUSTMENT FOR BODY MASS INDEX
CHANGES INVERSE ASSOCIATIONS OF HDL-CHOLESTEROL WITH BLOOD PRESSURE AND HYPERTENSION TO POSITIVE ASSOCIATIONS Article 11 May 2021 INTRODUCTION Hypertension is believed as a significant risk
factor for cardiovascular disease (CVD), and has brought heavy economic burden to individuals, families, and society1,2,3,4. It is a great challenge for public health worldwide, because of
its high prevalence, which accounts for nearly half of the cardiovascular morbidity and mortality in the world5,6. In 2010, people died from hypertension approximately 2 million in China,
accounting for about 24.60% of total mortality7. Therefore, hypertension is an important public health problem that are supposed to be addressed urgently. At present, hypertension has become
a hot research spot8,9, where most of studies focused primarily on hypertension, including prevalence, influencing factors, and health problems in cross-sectional and cohort
studies10,11,12,13. Sun _et al_.’s findings suggested that waist circumference (WC) was an independent predictor of hypertension incidence10, and Zhang _et al_.’s prospective study suggested
that body mass index (BMI) dynamic gain may be related to incident hypertension for men of all ages and young and middle-aged women13. Generally, hypertension was viewed as a categorical
variable in these studies, but the incidence of hypertension is a chronic and continuous process. In other words, literatures about risk factors of hypertension have been mounting, yet there
is a little of publications on determinants of the normal parts of blood pressure (BP). Fortunately, quantile regression (QR) is not limited to explain the prevalence risk of hypertension.
What’s more, it could also be used to explain the risk of the BP at any point on its distribution. QR comprehensively shows heterogeneous changes in the dispersion of the relationship of
risk factors with BP continuum across its distribution. In addition, there is no distributional assumptions about the error term in QR model, thus, it enjoys high flexibility for modeling
data with heterogeneous conditional distributions14. In this study, we aimed mainly to investigate how the whole continuum of BP was associated with commonly researched influencing factors
of hypertension using QR model. Jilin Province is situated in the northeast of China (latitude 40°~46°, longitude 121°~131°), with a cold climate and different residential dietary
pattern1,15. Therefore, we could develop more effective prevention strategies for different BP populations, so as to achieve the purpose of “precision prevention”. RESULTS DESCRIPTIVE
CHARACTERISTICS OF PARTICIPANTS BY GENDER Table 1 shows the basic characteristics of the participants, where BMI, SBP, DBP, TG and FPG were all significantly higher in males than those in
females (_P_ < 0.05), but age, TC, LDL-C and HDL-C were just the opposite (_P_ < 0.05). And the proportions of demographics (drinking, smoking, hypertension, dyslipidemia and diabetes,
etc.) were significantly different between genders. As shown in Table 2, the distribution of BP and quantiles between males and females were different. Therefore, we separately identified
the factors for males and females by using QR model. QR STATISTICS BETWEEN THE BP MEASURES IN FEMALES Tables 3~4 show QR coefficients and 95% confidence intervals of the influencing factors
for BP in females. Age was positively associated with both SBP and DBP. Similarly, BMI, TG, TC and family history of CVD showed significantly positive associations with SBP/DBP across the
entire conditional BP distribution. Females who used to live in town were positively associated with a higher DBP/SBP for most of the quantiles (≥10). Undergraduate females were negatively
associated with SBP for most of the quantiles (≥20). Middle school females were negatively associated with SBP for part of the quantiles. Female manual labors and mental labors were
positively associated with a higher DBP for part of the quantiles, compared with unemployed and retired females. QR STATISTICS BETWEEN THE BP MEASURES IN MALES Tables 5~6 provide QR
coefficients and 95% confidence intervals of the influencing factors for BP in males. Similar to females, age, BMI, TG and family history of CVD presented positive associations with both BP
measures across the entire conditional BP distribution. Drinking showed positive associations with SBP/DBP. High-salt diet manifested a slightly increasing positive association with higher
SBP (quantiles ≥ 70), but with a higher DBP for middle part of the quantiles (30~75), compared with the bland diet. Undergraduate males were negatively associated with SBP for most of the
quantiles (≥20). Male manual labors and mental labors were positively associated with a higher DBP across the entire conditional DBP distribution compared with unemployed and retired males.
In addition, HDL-C also showed a positive association with SBP/DBP. In general, the quantiles of HDL-C among participants with hypertension were lower than those with normal BP in males
(Table 7). In contrast, the relationship changed in different BMI groups: the relationship remained the same in normal weight group, however, the quantiles of HDL-C among participants with
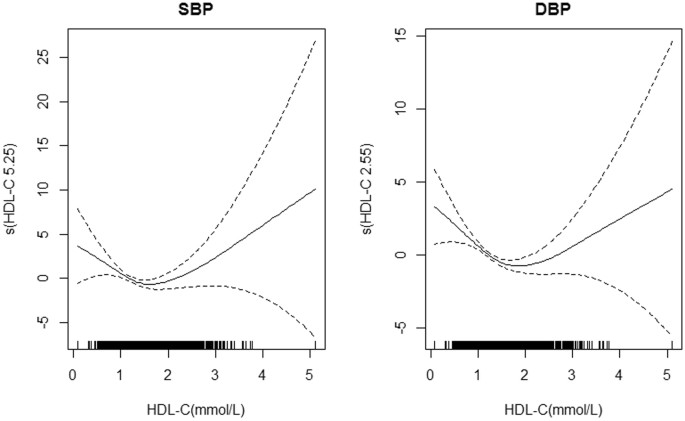
hypertension were higher than those with normal BP in underweight, overweight and obese groups. Further, the results of generalized additive models (GAM) showed that HDL-C performed
non-linear associations with both SBP (_F_ = 3.513, _P_ = 0.012) and DBP (_F_ = 7.388, _P_ < 0.001) (Fig. 1). DISCUSSION Hypertension has become a major public health problem in China7,
and a number of researchers have investigated the risk factors of hypertension5,16, but little is known about how the whole continuum of DBP and SBP is associated with commonly researched
influencing factors of hypertension. Measures in reducing the prevalence of hypertension in Jilin Province could be put forward after knowing the risk factors associated with BP. This study
explored the heterogeneity of the relationship of environmental and individual determinants with hypertension across the entire conditional distribution of BP measures using a QR model. It
was indicated that unhealthy eating habits was a predictor for higher BP measures in males, with a larger extent of the positive association at a higher quantile. Previous studies have
reported that BP was more prone to be elevated by alcohol drinking in males than in females17. In addition, it has been proven that high-salt diet was associated with BP18. Our results
showed that the high-salt was positively associated with BP only for the males, and the mechanism was probably correlated with estrogen and salt sensitivity. Estrogen affects the sodium
reabsorption and excretion via up regulation of NO production and different expression level of angiotensin receptors and ET receptors19. Therefore, males who maintain healthy lifestyle are
also likely to manage their BP better, and thereby have a lower risk of hypertension. Our study also investigated the effects of BMI and serum lipids on BP among adults. BMI showed a
positive association with BP in our study, which was consistent with the literature that obese people were more likely to be hypertensive compared with nonobese people20. Activation of the
renin–angiotensin system as well as physical compression of the kidney might be important factors in linking body weight and elevated BP21. Further, it has been proven that dyslipidemia was
associated with BP22. Our results showed that TG level was positively correlated with BP, and the mechanism was probably related with the insulin resistance23. Elevated TG level could make a
higher level of free fatty acids in serum, which would lead to insulin resistance, then insulin resistance further contributed to hyperinsulinemia, which might directly contribute to
elevation of BP by increasing renal sodium retention24. However, TC and HDL-C showed different associations with BP between males and females, which might be attributed to differences in sex
hormones, where estrogen was commonly believed to play an important role in lipolysis25. Moreover, HDL-C was positively associated with SBP/DBP in males, which was inconsistent with the
results in literature21,26. One possible reason was the nonlinear relationship between HDL-C and SBP/DBP, which showed a “U” shape that both too lower and too higher levels of HDL-C might
increase the risk of hypertension. Further, there might be an interaction between BMI and HDL-C, which showed that the HDL-C was higher among participants with hypertension than those with
normal BP in almost all BMI groups except those with normal BMI. Besides, other confounding risk factors27,28 that were not under our consideration might also have impacts on this
association. Furthermore, it has been proven that education was associated with hypertension29. Our results showed that education negatively associated with SBP. On one hand, the people with
higher level of education would have greater possibilities to engage in healthy lifestyles. On the other hand, older people were expected to have lower level of education than young people,
which might also lead to higher SBP30. In addition, we also found that working people were more likely to have an elevated DBP, and the possible reason might be related to social
engagement. Finally, the regression coefficient of family history of CVD increased with BP among all the research participates, which was consistent with other studies31. Thus, it was
implied that elderly people with family history of CVD, low-literacy and workers should pay more attention to their BP levels. Some limitations of our study should be noted. Firstly, the
results were conducted from a cross-sectional study in Jilin province, which might limit our ability to generalize the results. Secondly, other confounders that might have implications for
hypertension, such as parameters of glucose metabolism, renal function indices and genes, were not under our consideration this time, which might have some slight effects on our results.
CONCLUSIONS This study revealed interesting clues on how the whole continuum of SBP and DBP were associated with commonly researched factors of hypertension. High-salt diet, drinking and
HDL-C were positively associated with BP measures only in males. And the risk of TC had an increased trend with BP in females who used to live in town. The elderly, the obese, workers and
people with lower level of education and family history of CVD were expected to be positively associated with a higher SBP and/or DBP. METHODS STUDY POPULATION The large-scale
cross-sectional survey was conducted among people who aged 18 to79 years old and were living in Jilin Province for over 6 months in 2012. A total of 23,050 participants were selected through
multistage stratified random cluster sampling32 (see details in Part 1 of the Supplementary Material). For the purpose of the present analysis, the subjects who had anti-hypertensive
treatments were excluded, as well as those who had missing values in SBP or DBP. Finally, a total of 16,524 subjects were included in the present analyses. All participants provided written
informed consent, and the study was approved by the Institutional Review Board of the School of Public Health, Jilin University. And all methods were performed in accordance with the
relevant guidelines and regulations. DATA COLLECTION AND MEASUREMENT The data of this study included demographics (e.g., gender, age, etc.), health-related behaviors (e.g., smoking,
drinking, etc.), anthropometric measurements (e.g., height, weight, hypertension, etc.) and laboratory measurements (such as serum cholesterol and triglycerides). All investigation was
trained and followed the same questionnaire instructions. Height and weight were measured according to a standardized protocol and techniques, with the participants wearing clothing but no
shoes. A calibrated mercury sphygmomanometer was used to determine the blood pressure of subjects on the right arm, after at least 5 min of seated rest. The blood sample was obtained in the
morning from subjects after fasting for at least eight hours, and then conserved in tubes which contained ethylene diamine tetra acetic acid (EDTA). Fasting plasma glucose (FPG) and serum
lipids were measured using a Bai Ankang fingertip blood glucose monitor (Bayer, Leverkusen, Germany) and a MODULE P800 biochemical analysis machine (Roche Co., Ltd., Shanghai, China),
respectively33 (see details in Part 2 of the Supplementary Material). ASSESSMENT CRITERIA According to Seventh Joint National Commission Guidelines (JNC7), hypertension was defined as a
resting systolic blood pressure (SBP)/diastolic blood pressure (DBP) ≥ 140/90 mmHg or current use of antihypertensive medication34. Dyslipidemia was defined as the use of lipid-lowering
drugs in the past two weeks and/or meeting one or more of the following criteria: total cholesterol (TC) ≥ 6.22 mmol/L, triglyceride(TG) ≥ 2.26 mmol/L, low density lipoprotein cholesterol
(LDL-C) ≥ 4.14 mmol/L, high density lipoprotein cholesterol (HDL-C) < 1.04 mmol/L35. We defined diabetes as participants who reported diabetes mellitus previously diagnosed by physician
or those who have fasting plasma glucose (FPG) ≥ 7.0 mmol/L or oral glucose tolerance test (OGTT) 2 h plasma glucose (PG) ≥ 11.1 mmol/L36. BMI was defined as weight (kilogram) divided by
height (meter) squared. Drinker was defined as a person who consumed more than one alcoholic drink per week, including any form of alcohol37. High-salt diet was defined as a person who daily
salt intake more than 6 g38. Education stage was classified into compulsory education and lower education, secondary school education, senior school education, college education,
postgraduate education and higher education. STATISTICAL ANALYSIS All questionnaires were coded and double-entered. EpiData (version 3.1) was used for data entry and validation and R version
3.3.3(University of Auckland, Oakland, New Zealand) for data analysis. The data are presented as mean ± standard deviations (SD) or rate. In addition, quantitative variables and categorical
variables were analyzed using _t_ test and Rao-scott-_χ2_ test, respectively. Finally, QR in the quantreg package was used to estimate the conditional quantile of the distribution of SBP
and DBP under the influence of various risk factors. DATA AVAILABILITY The survey was implemented by School of Public Health, Jilin University and Jilin Center for Disease Control and
Prevention in Jilin Province in 2012. According to relevant regulations, we were sorry that the data can’t be shared. ABOUT THE DATA The survey was implemented by School of Public Health,
Jilin University and Jilin Center for Disease Control and Prevention in Jilin Province in 2012. According to relevant regulations, we were sorry that the data can’t be shared. REFERENCES *
Yu, J., Ma, Y., Yang, S., Pang, K., Yu, Y. & Tao, Y. _et al_. Risk Factors for Cardiovascular Disease and Their Clustering among Adults in Jilin (China). _Int J Environ Res Public
Health_ 13, h13010070 (2015). Article Google Scholar * Yu, D., Huang, J., Hu, D., Chen, J., Cao, J. & Li, J. _et al_. Association between prehypertension and clustering of
cardiovascular disease risk factors among Chinese adults. _J Cardiovasc Pharmacol_ 53, 388–400 (2009). Article CAS PubMed Google Scholar * Unal, S., Acar, B., Ertem, A. G. & Sen, F.
Endocan in Hypertension and Cardiovascular Diseases. _ANGIOLOGY_ 68, 85 (2017). Article PubMed Google Scholar * Lu, X., Huang, J., Wang, L., Chen, S., Yang, X. & Li, J. _et al_.
Genetic predisposition to higher blood pressure increases risk of incident hypertension and cardiovascular diseases in Chinese. _HYPERTENSION_ 66, 786–792 (2015). Article CAS PubMed
Google Scholar * Liu, X., Gu, W., Li, Z., Lei, H., Li, G. & Huang, W. Hypertension prevalence, awareness, treatment, control, and associated factors in Southwest China: an update. _J
HYPERTENS_ 35, 637–644 (2017). Article CAS PubMed Google Scholar * Ma, W. J. _et al_. Hypertension prevalence, awareness, treatment, control, and associated factors in adults in southern
China. _AM J HYPERTENS_ 25, 590–596 (2012). Article PubMed Google Scholar * Gao, Y., Chen, G., Tian, H., Lin, L., Lu, J. & Weng, J. _et al_. Prevalence of hypertension in china: a
cross-sectional study. _PLOS ONE_ 8, e65938 (2013). Article ADS CAS PubMed PubMed Central Google Scholar * Shen, X., Li, K., Chen, P., Feng, R., Liang, H. & Tong, G. _et al_.
Associations of Blood Pressure with Common Factors among Left-Behind Farmers in Rural China. _MEDICINE_ 94, e142 (2015). Article PubMed PubMed Central Google Scholar * Aounallah-Skhiri,
H. _et al_. Blood pressure and associated factors in a North African adolescent population. A national cross-sectional study in Tunisia. _BMC Public Health_ 12, 98 (2012). Article PubMed
PubMed Central Google Scholar * Sun, H. _et al_. Waist circumference and incidence of hypertension in Chinese adults: Observations from the Kailuan Study. _HERZ_ (2016). * Diederichs, C.
& Neuhauser, H. The incidence of hypertension and its risk factors in the German adult population: results from the German National Health Interview and Examination Survey 1998 and the
German Health Interview and Examination Survey for Adults 2008–2011. _J HYPERTENS_ 35, 250–258 (2017). Article CAS PubMed Google Scholar * Rautiainen, S. _et al_. Multivitamin use and
the risk of hypertension in a prospective cohort study of women. _J HYPERTENS_ 34, 1513–1519 (2016). Article CAS PubMed PubMed Central Google Scholar * Zhang M _et al_. Effect of
dynamic change in body mass index on the risk of hypertension: Results from the Rural Chinese Cohort Study. _INT J CARDIOL_ (2017). * Wei, Y., Pere, A., Koenker, R. & He, X. Quantile
regression methods for reference growth charts. _STAT MED_ 25, 1369–1382 (2006). Article MathSciNet PubMed Google Scholar * Wei, Q. _et al_. Prevalence of hypertension and associated
risk factors in Dehui City of Jilin Province in China. _J HUM HYPERTENS_ 29, 64–68 (2015). Article CAS PubMed Google Scholar * Olack, B. _et al_. Risk factors of hypertension among
adults aged 35-64 years living in an urban slum Nairobi, Kenya. _BMC PUBLIC HEALTH_ 15, 1251 (2015). Article PubMed PubMed Central Google Scholar * Wakabayashi, I. Influence of gender on
the association of alcohol drinking with blood pressure. _AM J HYPERTENS_ 21, 1310–1317 (2008). Article PubMed Google Scholar * Krupp, D., Shi, L., Egert, S., Wudy, S. A. & Remer, T.
Prospective relevance of fruit and vegetable consumption and salt intake during adolescence for blood pressure in young adulthood. _EUR J NUTR_ 54, 1269–1279 (2015). Article CAS PubMed
Google Scholar * Kim, J. M., Kim, T. H., Lee, H. H., Lee, S. H. & Wang, T. Postmenopausal hypertension and sodium sensitivity. _J Menopausal Med_ 20, 1–6 (2014). Article PubMed PubMed
Central Google Scholar * Czernichow, S., Castetbon, K., Salanave, B., Vernay, M., Barry, Y. & Batty, G. D. _et al_. Determinants of blood pressure treatment and control in obese
people: evidence from the general population. _J HYPERTENS_ 30, 2338–2344 (2012). Article CAS PubMed Google Scholar * Hall, J. E., Brands, M. W., Hildebrandt, D. A., Kuo, J. &
Fitzgerald, S. Role of sympathetic nervous system and neuropeptides in obesity hypertension. _BRAZ J MED BIOL RES_ 33(6), 605–618 (2000). Article CAS PubMed Google Scholar * Bonaa, K. H.
& Thelle, D. S. Association between blood pressure and serum lipids in a population. The Tromso Study. _CIRCULATION_ 83, 1305–1314 (1991). Article CAS PubMed Google Scholar *
Tangvarasittichai, S. Oxidative stress, insulin resistance, dyslipidemia and type 2 diabetes mellitus. _World J Diabetes_ 6, 456–480 (2015). Article PubMed PubMed Central Google Scholar
* Chavez-Canales, M., Arroyo, J. P., Ko, B., Vazquez, N., Bautista, R. & Castaneda-Bueno, M. _et al_. Insulin increases the functional activity of the renal NaCl cotransporter. _J
HYPERTENS_ 31, 303–311 (2013). CAS PubMed PubMed Central Google Scholar * Onat, A., Karadeniz, Y., Tusun, E., Yuksel, H. & Kaya, A. Advances in understanding gender difference in
cardiometabolic disease risk. _Expert Rev Cardiovasc Ther_ 14, 513–523 (2016). Article CAS PubMed Google Scholar * Wakabayashi, I. Associations of Blood Lipid-Related Indices with Blood
Pressure and Pulse Pressure in Middle-Aged Men. _METAB SYNDR RELAT D_ 13, 22–28 (2015). Article CAS Google Scholar * Carroll, D., Phillips, A. C., Gale, C. R. & Batty, G. D.
Generalized anxiety and major depressive disorders, their comorbidity and hypertension in middle-aged men. _PSYCHOSOM MED_ 72, 16–19 (2010). Article PubMed Google Scholar * Fan, W., Qu,
X., Li, J., Wang, X., Bai, Y. & Cao, Q. _et al_. Associations between polymorphisms of the ADIPOQ gene and hypertension risk: a systematic and meta-analysis. _Sci Rep_ 7, 41683 (2017).
Article ADS CAS PubMed PubMed Central Google Scholar * Gupta, R. _et al_. Association of Household Wealth Index, Educational Status, and Social Capital with Hypertension Awareness,
Treatment, and Control in South Asia. _AM J HYPERTENS_ (2017). * Franklin, S. S. _et al_. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study.
_CIRCULATION_ 96, 308–315 (1997). Article CAS PubMed Google Scholar * Williamson, C., Jeemon, P., Hastie, C. E., McCallum, L., Muir, S. & Dawson, J. _et al_. Family history of
premature cardiovascular disease: blood pressure control and long-term mortality outcomes in hypertensive patients. _EUR HEART J_ 35, 563–570 (2014). Article PubMed Google Scholar * Wang,
C., Yu, Y., Zhang, X., Li, Y., Kou, C. & Li, B. _et al_. Awareness, treatment, control of diabetes mellitus and the risk factors: survey results from northeast China. _PLOS ONE_ 9,
e103594 (2014). Article ADS PubMed PubMed Central Google Scholar * Xie, X., Ma, Y. T., Yang, Y. N., Fu, Z. Y., Li, X. M. & Zheng, Y. Y. _et al_. Polymorphisms in the SAA1 gene are
associated with ankle-to-brachial index in Han Chinese healthy subjects. _Blood Press_ 20, 232–238 (2011). Article CAS PubMed Google Scholar * Executive Summary of the Third Report of
the National Cholesterol Education Program (NCEP). Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). _JAMA_ 285, 2486–2497
(2001). Article Google Scholar * Dong, X., Liu, Y., Yang, J., Sun, Y. & Chen, L. Efficiency of anthropometric indicators of obesity for identifying cardiovascular risk factors in a
Chinese population. _POSTGRAD MED J_ 87, 251–256 (2011). Article PubMed Google Scholar * Basevi V, Di Mario S, Morciano C, Nonino F & Magrini N. Comment on: American Diabetes
Association. Standards of medical care in diabetes–2011. Diabetes Care 201134(Suppl. 1):S11-S61. _DIABETES CARE_ 34, e53, e54 (2011). * Zhang P, Wang R, Gao C, Song Y, Lv X & Jiang L _et
al_. Types of Obesity and Its Association with the Clustering of Cardiovascular Disease Risk Factors in Jilin Province of China. _Int J Environ Res Public Health_ 13, (2016). * Lewington,
S., Clarke, R., Qizilbash, N., Peto, R. & Collins, R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in
61 prospective studies. _LANCET_ 360, 1903–1913 (2002). Article PubMed Google Scholar Download references ACKNOWLEDGEMENTS I would like to express my gratitude to all those who have
helped me during the writing of this thesis. This work was supported by the Outstanding Youth Foundation of Science and Technology Department of Jilin Province, China (grant number:
20170520049JH); the National Natural Science Foundation of China (grant number: 11301213, 11571068); and the Scientific Research Foundation of the Health Bureau of Jilin Province, China
(grant number: 2011Z116). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Epidemiology and Biostatistics, School of Public Health, NO. 1163 Xinmin Street, Jilin University, Changchun, Jilin,
China, 130021 Junsen Ye, Zhongmin Li, Yaogai Lv, Lan An, Jianxing Yu, Xin Guo, Yan Yao, Yaqin Yu & Lina Jin Authors * Junsen Ye View author publications You can also search for this
author inPubMed Google Scholar * Zhongmin Li View author publications You can also search for this author inPubMed Google Scholar * Yaogai Lv View author publications You can also search for
this author inPubMed Google Scholar * Lan An View author publications You can also search for this author inPubMed Google Scholar * Jianxing Yu View author publications You can also search
for this author inPubMed Google Scholar * Xin Guo View author publications You can also search for this author inPubMed Google Scholar * Yan Yao View author publications You can also search
for this author inPubMed Google Scholar * Yaqin Yu View author publications You can also search for this author inPubMed Google Scholar * Lina Jin View author publications You can also
search for this author inPubMed Google Scholar CONTRIBUTIONS The authors would like to thank Dr Lina Jin and others who kindly provided their R code for analysis and experience for writing
paper. Junsen Ye and Lina Jin had the original idea for the study and carried out the design. Lina Jin and Zhongmin Li provided valuable insight regarding the methodological approach and
organization of the manuscript. Junsen Ye, Jianxing Yu, Yaogai Lv and Lan An carried out the statistical analysis and reviewed the consistency of data included in the paper. Junsen Ye and
Zhongmin Li drafted the manuscript. Xin Guo, Yan Yao and Yaqin Yu revised the manuscript. All authors read and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Lina Jin.
ETHICS DECLARATIONS COMPETING INTERESTS The authors declare that they have no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard
to jurisdictional claims in published maps and institutional affiliations. ELECTRONIC SUPPLEMENTARY MATERIAL SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is
licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in
this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative
Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a
copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Ye, J., Li, Z., Lv, Y. _et al._ Associations of Blood
Pressure with the Factors among Adults in Jilin Province: A Cross-Sectional Study Using Quantile Regression Analysis. _Sci Rep_ 7, 13613 (2017). https://doi.org/10.1038/s41598-017-14045-0
Download citation * Received: 07 July 2017 * Accepted: 05 October 2017 * Published: 19 October 2017 * DOI: https://doi.org/10.1038/s41598-017-14045-0 SHARE THIS ARTICLE Anyone you share the
following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer
Nature SharedIt content-sharing initiative