Play all audios:
ABSTRACT To investigate the prognostic value of heart-type fatty acid binding protein (H-FABP) in patients with stable coronary heart disease (SCHD). A total of 1,071 patients with SCHD were
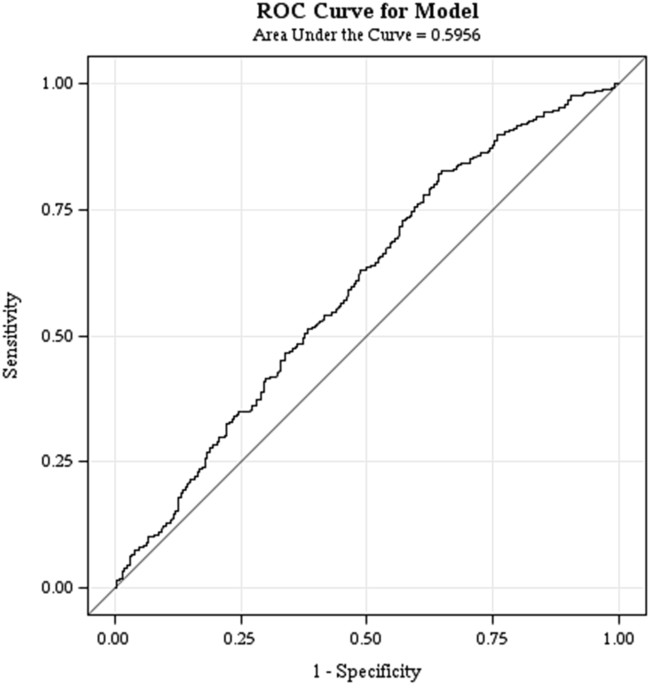
prospectively enrolled in this Taiwan multicenter registry study, followed for 24 months. The cut-off value of H-FABP, 4.143 ng/mL, was determined using receiver operating characteristic
curves. The primary cardiovascular (CV) outcome was composite CV events, defined as cardiovascular or cerebrovascular death, myocardial infarction (MI), stroke, angina
related-hospitalization, PAOD-related hospitalization and heart failure. Secondary outcomes included CV or cerebrovascular death, nonfatal MI, nonfatal stroke, and acute heart
failure-related hospitalization. We found that the high H-FABP group had more than a two-fold higher rate of primary CV outcomes than the low H-FABP group (32.36% vs. 15.78%, _p_ <
0.001). Eleven patients (4.82%) of the high H-FABP group died during the 24 months of follow-up, compared to only one patient (0.12%) in the low H-FABP group. The acute heart failure-related
hospitalization rate was also significantly higher in the high H-FABP group (3.5% vs. 0.95%, _p_ < 0.005). The results remained significant after adjusting for baseline covariates. In
conclusion, H-FABP was an independent predictor for CV outcomes in the patients with SCHD, mainly in CV death and acute heart failure-related hospitalization. SIMILAR CONTENT BEING VIEWED BY
OTHERS THE EFFECT OF HSCRP ON TYG INDEX-ASSOCIATED CARDIOVASCULAR RISK IN PATIENTS WITH ACUTE CORONARY SYNDROME UNDERGOING PCI Article Open access 05 August 2024 NEUTROPHIL TO HIGH-DENSITY
LIPOPROTEIN CHOLESTEROL RATIO AS THE RISK MARK IN PATIENTS WITH TYPE 2 DIABETES COMBINED WITH ACUTE CORONARY SYNDROME: A CROSS-SECTIONAL STUDY Article Open access 15 May 2023 CORRELATION
ANALYSIS BETWEEN EPICARDIAL ADIPOSE TISSUE AND ACUTE CORONARY SYNDROME Article Open access 24 January 2025 INTRODUCTION Ischemic heart disease and stroke have been the leading causes of
death globally in the past decades, and the mortality rate from these diseases is gradually increasing. In addition to traditional cardiovascular (CV) risk factors such as smoking, type 2
diabetes mellitus (T2DM), hypertension (HTN) and dyslipidemia, researchers have investigated potential novel biomarkers, for instance, copeptin1, pentraxin-32 and heart-type fatty acid
binding protein (H-FABP) to predict the clinical course and CV outcomes. In particular, H-FABP has been widely studied in patients with acute coronary syndrome (ACS), and it has been
suggested to increase diagnostic sensitivity and possibly predict long-term survival3. H-FABP is a human protein that is encoded by the fatty acid binding protein 3 (FABP3) gene and is
located on chromosome 1p32-p35. It is a cytoplasmic protein which was first isolated from ischemic rat hearts in 1988, and was identified as being released from injured myocardium4,5.
Associations between H-FABP and ACS6,7,8, acute kidney injury9, post-cardiac surgery10, acute pulmonary embolism11, acute ischemic stroke12, severe sepsis13, acute heart failure14,
hypothyroidism15 and hyperthyroidism16 have been reported over the past decades. On the other hand, H-FABP has also been used to assess perioperative cardiac risk17,18. However, the
prognostic implication of H-FABP in patients with stable coronary heart disease (SCHD) is unknown. The aim of this study was to investigate the prognostic value of H-FABP in CV outcomes in
patients with SCHD. RESULTS PATIENTS A total of 1,072 SCHD patients from the National Taiwan Biosignature Research (NTBR) cohort study were enrolled and followed for 24 months or until a CV
event. At 24 months, 207 cardiovascular events had occurred, including 12 CV deaths, 24 nonfatal myocardial infarction (MI), 6 nonfatal strokes and 16 acute heart failure-related
hospitalizations (Table 1). The cut-off value of H-FABP (4.143 ng/mL) was determined by receiver operating characteristic curves (ROC) curve analysis (Fig. 1) between the patients with and
without CV events from the blood sample obtained at enrollment. The baseline characteristics revealed that the patients with a high level of H-FABP had higher rates of HTN, but lower rate of
family history of premature coronary artery disease (CAD). Except for a lower level of serum high-density lipoprotein cholesterol (HDL-C), patients with a high level of H-FABP had
significantly higher blood glucose, systolic blood pressure (SBP), serum creatinine, high sensitivity C-reactive protein (hs-CRP) and N-terminal pro-brain natriuretic peptide (NT-proBNP)
than those with a low level of H-FABP (Table 2). PRIMARY OUTCOMES After 24 months of follow up, the high H-FABP group had more than a two-fold higher rate of primary CV events than the low
H-FABP group (32.36% vs. 15.78%, _p_ < 0.001) (Table 3). The Kaplan-Meier curves of the two groups were significantly separated from the beginning of the study to 24 months (Fig. 2a).
SECONDARY OUTCOMES A total of 11 deaths (4.82%) occurred in the high H-FABP group, compared with only one (0.12%) in the low H-FABP group (Table 3 and Fig. 2b). In addition, the high H-FABP
group had a significantly higher rate of acute heart failure-related hospitalizations (3.5%) compared to the low H-FABP group (0.95%) (Table 3 and Fig. 2c). Although statistically
non-significant, there was also a trend of higher rate of nonfatal MI and nonfatal stroke in the high H-FABP group (Table 3). There were 80 patients with total CV events except for
“angina-related hospitalization”, 38 patients in H-FABP group, 42 patients in H-FABP group (4.51% vs 32.46%, _p_ < 0.001). The difference between these two groups remained significant
(Fig. 2d). In multivariate Cox proportional hazards analysis adjusted for age, sex, body mass index (BMI), serum creatinine, estimated glomerular filtration rate (eGFR), HDL-C, hemoglobin
(Hb), blood glucose, hs-CRP, NT-proBNP, SBP, smoking, family history of premature CAD, history of hypertension and diabetes mellitus, high H-FABP level was still an independent prognostic
risk factor for CV events (HR 2.93, 95% CI 1.95–4.394, _p_ < 0.001). In addition, a high level of H-FABP also predicted CV death (HR 22.89, 95% CI 2.16–242.55, _p_ = 0.009) and acute
heart failure-related hospitalizations (HR 5.16, 95% CI 1.096–24.324, _p_ = 0.038) in the 24-month follow-up period, even after adjusted for other covariates (Table 4). DISCUSSION This study
is the first prospective cohort study to demonstrate that a higher serum H-FABP level (≧4.143 ng/mL) is an independent predictor for CV events, particularly for cardio- and cerebrovascular
death and acute heart failure-related hospitalizations in patients with SCHD. Our result was concordant with the Takahata study19, which also found that H-FABP level was increased in
association with greater numbers of cardiovascular risk factors. In addition, Takahata study noted higher H-FABP level was an independent risk factor for all-cause and cardiovascular deaths
in 3,503 subjects who participated in a community-based health checkup in a 7-year follow-up. The early diagnosis of acute MI is still challenging for emergency physicians despite the wide
application of myoglobin and high-sensitivity cardiac troponin (cTn) in emergency rooms, because the elevation of most myocardial injury serum markers are delayed by at least 2–4 hours after
an ischemic insult. In 2000, an experimental study of ligation of the left main coronary artery in mice demonstrated that the concentration of H-FABP at 4 hours could be used to stratify MI
compared to cTn at 48 hours20. In addition, Okamoto _et al_. reported that H-FABP is more sensitive than myoglobin and creatinine kinase isoenzyme MB for the diagnosis of acute MI in the
early phase21. In 2006, O’Donoghue _et al_. reported an association between an elevated level of H-FABP and increased risks of death and major cardiac events in patients with ACS22.
Collinson _et al_.23 compared the diagnostic performances of cTn-I, H-FABP and copeptin in low-risk patients presenting with chest pain. The authors concluded that cTn-I remained the best
single test, with the incremental diagnostic sensitivity of serum H-FABP, but not copeptin. Furthermore, a recent dobutamine stress echocardiography (DSE) study reported significantly
increased levels of serum H-FABP at 1 hour in the presence of DSE-induced ischemia, in contrast to DSE negative group, whose serum H-FABP remained unchanged before and 1 hour after the
test24. However, in a study that was expected H-FABP to increase during exercise stress testing (EST), serum H-FABP tended to decline statistically significant from the basal level to 3
hours after the EST25. A recent systemic review of H-FABP in ACS found marked heterogeneity in the prognostic impact of H-FABP between studies, reflecting differences in sampling times and
the population at risk. Hence, it may not be possible to routinely use H-FABP as a prognostic marker in patients with suspected ACS26. Wunderlich _et al_. were the first to report that an
early elevation of serum H-FABP and brain type fatty acid binding protein (B-FABP) concentration were significantly associated with the severity of neurological deficits and functional
outcomes in patients after an acute ischemic stroke12. The peak levels of H-FABP and B-FABP occur 2 to 3 hours after an event and remain elevated for up to 120 hours. In addition, a high
level of H-FABP is associated with large infarctions on brain computed tomography. Another investigation of 41 patients with acute stroke (31 with ischemic stroke, 10 with intracerebral
hemorrhage) demonstrated that serum H-FABP and ischemic-modified albumin (IMA) levels increased within 4.5 hours27. Nonetheless, An _et al_. reported that H-FABP was not an independent
marker in patients with ischemic stroke, and thus that its clinical usefulness is limited28. In the current study, we demonstrated the prognostic value of H-FABP in CV events in patients
with SCHD after successful treatment, but that it had limited value in the prediction of nonfatal MI and ischemic stroke. In this study, although statistically non-significant, there was
also a trend of higher rate of nonfatal MI and nonfatal stroke in the high H-FABP group. The relationship between H-FABP and heart failure was first reported in the early 2000s, when the
concentration of H-FABP was positively correlated with the concentration of BNP in patients with acute deterioration of heart failure29. Later, Setsuka _et al_.30 reported that H-FABP was
present in the activation of tumor necrosis factor (TNF) and the Fas ligand system. This suggested a pathophysiological role of cardiomyocyte necrosis and/or apoptosis in patients with
worsening heart failure. Moreover, Hoffmann _et al_.14 investigated H-FABP in acute heart failure, and found that additional H-FABP measurements improved the diagnostic specificity and
positive predictive value of NT-proBNP tests. In addition, their patients in the highest H-FABP quartile had significantly higher rates of all-cause mortality (HR 2.1–2.5; _p_ = 0.04) and
risk of re-hospitalization for acute heart failure at 5 years (HR 2.8–8.3, _p_ = 0.001). Our study also demonstrated that the SCHD patients with high H-FABP level had a higher risk for acute
heart failure-related hospitalizations at 24 months. There are several limitations of this study. First, even though the criteria for patient enrollment and the protocol for clinical
follow-up were clearly defined, selection bias arising from clinical profiles, investigator participation and treatment adherence by the patients could not be completely excluded31. Second,
this is a hospital based rather than a community-based study, and this design was potentially limited by geographic variations such as environmental exposure to risk factors of CV disease32.
Third, all the patients were stable during enrollment and followed up regularly for clinical events in the out-patient clinics of the medical centers. Their medications may have been
adjusted by the specific cardiologists during follow-up. Thus, the potential effects of different cardiovascular drugs on clinical outcomes could not be well addressed33. Fourth, the very
few cases of the each secondary event category, insufficient statistical power of predictive value of H-FABP could be derived from the multivariate analyses. In conclusion, H-FABP was an
independent predictor for total CV events in the patients with SCHD at 24 months, mainly for CV and cerebrovascular deaths and acute heart failure-related hospitalization. METHODS STUDY
POPULATION This NTBR was a prospective cohort study of patients with SCHD (aged ≧ 20 years) from nine medical centers in Taiwan31. At enrollment, all of the participants had undergone a
percutaneous coronary intervention at least once and had been stable on medical treatment for at least 1 month. The exclusion criteria included hospitalization for any CV event within 3
months, and those unable or unwilling to be followed up during the following 1 year period. Specific clinical outcomes including all-cause, cardiovascular, cerebrovascular mortalities, and
CV-related hospitalizations were confirmed using the Health and Welfare Data Science Center (HWDC) of Taiwan. This study complied with the Declaration of Helsinki and was approved by the
appropriate Health Authorities, independent Ethics Committees, and Institutional Review Boards (IRB) in each hospital as well as the Joint IRB Ethics Committee Review Board in Taiwan. All of
the patients agreed to participate and signed the informed consent form. BASELINE CLINICAL AND BIOMARKER DATA COLLECTION After enrollment, data were prospectively collected by physicians
and nurses whenever feasible. Baseline characteristics included sex, age, HTN, T2DM, hyperlipidemia, smoking, family history of premature CAD, BMI, number of stenotic coronary arteries, and
biochemical data including renal function, lipid profile at enrollment in each hospital were recorded. Hs-CRP was performed automatically with chemiluminescent immunoassay methods, on a
Beckman Coulter DXC 800 immunoassay platform (Beckman Coulter, Inc. CA, USA). NT-pro BNP and H-FABP were measured manually on EMD Millipore’s MILLIPLEX MAP Human CVD 1 Magnetic Bead kit
(Millipore, Inc. MO, USA). CLINICAL FOLLOW-UP Questionnaire and blood samples were obtained from the patients every 3 months in the first year and every 6 months thereafter for a total of 24
months. The primary CV outcome was composite CV events, defined as cardiovascular or cerebrovascular death, MI, stroke, angina-related hospitalization, PAOD-related hospitalization and
heart failure. Heart failure was a composite of acute heart failure-related hospitalization, syncope, cardiopulmonary resuscitation, bradyarrhythmia, supraventricular tachyarrhythmia,
ventricular arrhythmia, permanent pacemaker implantation and aortic dissection. The secondary outcomes included CV or cerebrovascular death, nonfatal MI, nonfatal stroke, and acute heart
failure-related hospitalization. STATISTICAL ANALYSIS The cut-off value of H-FABP was determined using ROC curve analysis between the patients with and without CV events from the blood
sample obtained at enrollment. Baseline characteristics and CV outcomes were compared between the patients with high and low levels of H-FABP. Results are expressed as median (interquartile
ranges [IQRs]) for continuous variables, and qualitative variables are expressed in absolute frequencies (number of patients) and relative frequencies (percentage). Comparisons of continuous
variables between groups were performed using ANOVA or Mann-Whitney _U_ tests. The primary and secondary outcomes were described as overall percentages and expressed as means of proportions
with a 95% confidence interval (CI). The Kaplan-Meier method was used to calculate events and survival rates. Hazard ratios (HRs) for the regression of Cox proportional hazards were used,
along with the corresponding standard error, 95% CI, and _p_ value. Independent baseline variables with a _p_ value < 0.05 in the univariate analysis were included in the multivariate
analysis. In all the tests, the two-tailed alpha significance level was 0.05. In addition, _p_ values were reported up to three decimals, while those below 0.001 were reported as _p_ <
0.001. CHANGE HISTORY * _ 13 MARCH 2019 A correction to this article has been published and is linked from the HTML and PDF versions of this paper. The error has been fixed in the paper. _
REFERENCES * Boeckel, J. N. _et al_. Analyzing the release of copeptin from the heart in acute myocardial infarction using a transcoronary gradient model. _Sci Rep._ 6, 20812 (2016). Article
ADS CAS Google Scholar * Vengen, I. T., Enger, T. B., Videm, V. & Garred, P. Pentraxin 3, ficolin-2 and lectin pathway associated serine protease MASP-3 as early predictors of
myocardial infarction – the HUNT2 study. _Sci Rep._ 7, 43045 (2017). Article ADS CAS Google Scholar * Schoenenberger, A. W. _et al_. Incremental value of heart-type fatty acid-binding
protein in suspected acute myocardial infarction early after symptom onset. _Eur Heart J Acute Cardiovasc Care._ 5, 185–192 (2016). Article Google Scholar * Phelan, C. M. _et al_. The
human mammary-derived growth inhibitor (MDGI) gene: genomic structure and mutation analysis in human breast tumors. _Genomics._ 34, 63–68 (1996). Article CAS Google Scholar * Glatz, J. F.
_et al_. Release of fatty acid-binding protein from isolated rat heart subjected to ischemia and reperfusion or to the calcium paradox. _Biochim Biophys Acta._ 961, 148–152 (1988). Article
CAS Google Scholar * Dupuy, A. M. _et al_. Performances of the heart fatty acid protein assay for the rapid diagnosis of acute myocardial infarction in ED patients. _Am J Emerg Med._ 33,
326–330 (2015). Article Google Scholar * Liebetrau, C. _et al_. Release kinetics of early ischaemic biomarkers in a clinical model of acute myocardial infarction. _Heart._ 100, 652–657
(2014). Article Google Scholar * Uitterdijk, A. _et al_. Serial measurement of hFABP and high-sensitivity troponin I post-PCI in STEMI: how fast and accurate can myocardial infarct size
and no-reflow be predicted? _Am J Physiol Heart Circ Physiol._ 305, 1104–1110 (2013). Article Google Scholar * Shirakabe, A. _et al_. The serum heart-type fatty acid-binding protein
(HFABP) levels can be used to detect the presence of acute kidney injury on admission in patients admitted to the non-surgical intensive care unit. _BMC Cardiovasc Disorders._ 16, 174
(2016). Article Google Scholar * Parikh, C. R. _et al_. Relationship of kidney injury biomarkers with long-term cardiovascular outcomes after cardiac surgery. _J Am Soc Nephrol._ 28,
3699–3707 (2017). Article CAS Google Scholar * Langer, M. _et al_. Heart-type fatty acid-binding protein and myocardial creatine kinase enable rapid risk stratification in normotensive
patients with pulmonary embolism. _J Crit Care._ 35, 174–179 (2016). Article CAS Google Scholar * Wunderlich, M. T. _et al_. Release of brain-type and heart-type fatty acid-binding
proteins in serum after acute ischaemic stroke. _J Neurol._ 252, 718–724 (2005). Article CAS Google Scholar * Zhang, Z. C., Dai, H. W., Yu, Y. H., Yang, J. D. & Hu, C. B. Usefulness
of heart-type fatty acid-binding protein in patients with severe sepsis. _J Crit Care._ 27, 415.e13–415.e18 (2012). Article CAS Google Scholar * Hoffmann, U. _et al_. Ischemic biomarker
heart-type fatty acid binding protein (hFABP) in acute heart failure - diagnostic and prognostic insights compared to NT-proBNP and troponin I. _BMC Cardiovasc Disord._ 15, 50 (2015).
Article Google Scholar * Gunes, F. _et al_. Serum H-FABP levels in patients with hypothyroidism. _Wien Klin Wochenschr._ 126, 727–733 (2014). Article CAS Google Scholar * Ozbek, M. _et
al_. Serum heart type fatty acid binding protein levels are not changed in hyperthyroidism. _Minerva Endocrinol._ 41, 298–301 (2016). PubMed Google Scholar * Marković, D. Z. _et al_.
Addition of biomarker panel improves prediction performance of American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP) calculator for cardiac risk assessment
of elderly patients preparing for major non-cardiac surgery: a pilot study. _Aging Clin Exp Res._ 30, 419–431 (2018). Article Google Scholar * Sari, M., Kilic, H., Ariturk, O. K., Yazihan,
N. & Akdemir, R. Diabetic patients have increased perioperative cardiac risk in heart-type fatty acid-binding protein-based assessment. _Med Princ Pract._ 24, 53–57 (2015). Article
Google Scholar * Otaki, Y. _et al_. Association of heart-type fatty acid-binding protein with cardiovascular risk factors and all-cause mortality in the general population: the Takahata
study. _PLoS One._ 9, e94834 (2014). Article ADS Google Scholar * Aartsen, W. M. _et al_. Heart fatty acid binding protein and cardiac troponin T plasma concentrations as markers for
myocardial infarction after coronary artery ligation in mice. _Pflugers Arch._ 439, 416–422 (2000). Article CAS Google Scholar * Okamoto, F. _et al_. Human heart-type cytoplasmic fatty
acid-binding protein (H-FABP) for the diagnosis of acute myocardial infarction. Clinical evaluation of H-FABP in comparison with myoglobin and creatine kinase isoenzyme MB. _Clin Chem Lab
Med._ 38, 231–238 (2000). Article CAS Google Scholar * O’Donoghue, M. _et al_. Prognostic utility of heart-type fatty acid binding protein in patients with acute coronary syndromes.
_Circulation._ 114, 550–557 (2006). Article Google Scholar * Collinson, P., Gaze, D. & Goodacre, S. Comparison of contemporary troponin assays with the novel biomarkers, heart fatty
acid binding protein and copeptin, for the early confirmation or exclusion of myocardial infarction in patients presenting to the emergency department with chest pain. _Heart._ 100, 140–145
(2014). Article CAS Google Scholar * Akinci, S. _et al_. Effect of dobutamine stress echocardiography on serum heart fatty acid binding protein levels. _Acta Cardiol._ 72, 161–166 (2017).
Article Google Scholar * Arı, H. _et al_. Relationship between heart-type fatty acid-binding protein levels and coronary artery disease in exercise stress testing: an observational study.
_Anadolu Kardiyol Derg._ 11, 685–691 (2011). PubMed Google Scholar * Jones, J. D. _et al_. The Prognostic value of heart type fatty acid binding protein in patients with suspected acute
coronary syndrome: a systematic review. _Curr Cardiol Rev._ 13, 189–198 (2017). Article CAS Google Scholar * Herisson, F., Delaroche, O., Auffray-Calvier, E., Duport, B. D. & Guillon,
B. Ischemia-modified albumin and heart fatty acid-binding protein: could early ischemic cardiac biomarkers be used in acute stroke management? _J Stroke Cerebrovasc Dis._ 19, 279–282
(2010). Article Google Scholar * An, S. A. _et al_. Limited clinical value of multiple blood markers in the diagnosis of ischemic stroke. _ClinBiochem._ 46, 710–715 (2013). CAS Google
Scholar * Goto, T. _et al_. Circulating concentrations of cardiac proteins indicate the severity of congestive heart failure. _Heart_ 89, 1303–1307 (2003). Article CAS Google Scholar *
Setsuta, K. _et al_. Ongoing myocardial damage in chronic heart failure is related to activated tumor necrosis factor and Fas/Fas ligand system. _Circ J_ 68, 747–750 (2004). Article CAS
Google Scholar * Leu, H. B. _et al_. Identification of new biosignatures for clinical outcomes in stable coronary artery disease - The study protocol and initial observations of a
prospective follow-up study in Taiwan. _BMC Cardiovasc Disord._ 17, 42 (2017). Article Google Scholar * Chien, S. C. _et al_. Association of low serum albumin concentration and adverse
cardiovascular events in stable coronary heart disease. _Int J Cardiol_ 241, 1–5 (2017). Article Google Scholar * Huang, C. C. _et al_. Optimal achieved blood pressure for patients with
stable coronary artery disease. _Sci Rep._ 7, 10137 (2017). Article ADS Google Scholar Download references ACKNOWLEDGEMENTS Biosignature project is supported by Academia Sinica (project
number: BM10501010039) and Taiwan Clinical Trial Consortium of Cardiovascular Diseases (TCTC-CVD) (project number: MOST 106-2321-B-002-029-). AUTHOR INFORMATION Author notes * Yen-Wen Wu and
Chau-Chung Wu contributed equally. AUTHORS AND AFFILIATIONS * Cardiology Division of Cardiovascular Medical Center, Far Eastern Memorial Hospital, New Taipei City, Taiwan Sing-Kong Ho &
Yen-Wen Wu * Cardiology Division, Department of Internal Medicine, Miaoli General Hospital, Ministry of Health and Welfare, Miaoli, Taiwan Sing-Kong Ho * National Yang-Ming University
School of Medicine, Taipei, Taiwan Yen-Wen Wu * Department of Medical Imaging and Radiological Sciences, I-Shou University, Kaohsiung, Taiwan Wei-Kung Tseng * Division of Cardiology,
Department of Internal Medicine, E-Da Hospital, Kaohsiung, Taiwan Wei-Kung Tseng * Institute of Clinical Medicine and Cardiovascular Research Center, National Yang-Ming University, Taipei,
Taiwan Hsin-Bang Leu & Jaw-Wen Chen * Divison of Cardiology, Department of Medicine, Taipei Veterans General Hospital, Taipei, Taiwan Hsin-Bang Leu & Jaw-Wen Chen * Division of
Cardiology, Heart Center, Cheng-Hsin General Hospital, and School of Medicine, National Yang-Ming University, Taipei, Taiwan Wei-Hsian Yin * Division of Cardiology, Department of Internal
Medicine, Kaohsiung Medical University Hospital and Kaohsiung Medical University, Kaohsiung, Taiwan Tsung-Hsien Lin * Division of Cardiovascular Medicine, China Medical University Hospital,
Taichung, Taiwan Kuan-Cheng Chang * Graduate Institute of Biomedical Sciences, China Medical University, Taichung, Taiwan Kuan-Cheng Chang * Department of Cardiology, Buddhist Tzu-Chi
General Hospital, Tzu-Chi University, Hualien, Taiwan Ji-Hung Wang * Cardiovascular Division, Department of Internal Medicine, MacKay Memorial Hospital, Mackay Medical College, New Taipei
City, Taiwan Hung-I Yeh * Division of Cardiology, Department of Internal Medicine, National Taiwan University Hospital and National Taiwan University College of Medicine, Taipei, Taiwan
Chau-Chung Wu * Graduate Institute of Medical Education & Bioethics, College of Medicine, National Taiwan University, Taipei, Taiwan Chau-Chung Wu Authors * Sing-Kong Ho View author
publications You can also search for this author inPubMed Google Scholar * Yen-Wen Wu View author publications You can also search for this author inPubMed Google Scholar * Wei-Kung Tseng
View author publications You can also search for this author inPubMed Google Scholar * Hsin-Bang Leu View author publications You can also search for this author inPubMed Google Scholar *
Wei-Hsian Yin View author publications You can also search for this author inPubMed Google Scholar * Tsung-Hsien Lin View author publications You can also search for this author inPubMed
Google Scholar * Kuan-Cheng Chang View author publications You can also search for this author inPubMed Google Scholar * Ji-Hung Wang View author publications You can also search for this
author inPubMed Google Scholar * Hung-I Yeh View author publications You can also search for this author inPubMed Google Scholar * Chau-Chung Wu View author publications You can also search
for this author inPubMed Google Scholar * Jaw-Wen Chen View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS S.K.H., Y.-W.W. and C.-C.W.
conceived and designed the research. Y.-W.W., W.-K.T., H.-B.L., W.-H.Y., T.-H.L., H.-I.Y., K.-C.C., J.-H.W., J.-W.C. and C.-C.W. managed data collection. S.K.H. drafted the manuscript and
designed the figures and tables. Y.-W.W. and C.-C.W. made critical revision of the manuscript. All authors reviewed the manuscript. CORRESPONDING AUTHORS Correspondence to Yen-Wen Wu or
Chau-Chung Wu. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE: Springer Nature remains neutral with regard
to jurisdictional claims in published maps and institutional affiliations. A full list of consortium members appears in the Supplementary Information ELECTRONIC SUPPLEMENTARY MATERIAL
SUPPLEMENTARY INFORMATION RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation,
distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and
indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to
the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will
need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE
CITE THIS ARTICLE Ho, SK., Wu, YW., Tseng, WK. _et al._ The prognostic significance of heart-type fatty acid binding protein in patients with stable coronary heart disease. _Sci Rep_ 8,
14410 (2018). https://doi.org/10.1038/s41598-018-32210-x Download citation * Received: 21 February 2018 * Accepted: 30 August 2018 * Published: 26 September 2018 * DOI:
https://doi.org/10.1038/s41598-018-32210-x SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * Heart-type Fatty Acid-binding Protein (H-FABP) * Stable
Coronary Heart Disease (SCHD) * Cerebrovascular Deaths * Acute Heart Failure * Nonfatal Stroke