Play all audios:
ABSTRACT 234 diagnostic formalin-fixed paraffin-embedded (FFPE) blocks from homogeneously treated patients with locally advanced head and neck squamous cell carcinoma (HNSCC) within a
multicentre phase III clinical trial were characterised. The mutational spectrum was examined by next generation sequencing in the 26 most frequent oncogenic drivers in cancer and correlated
with treatment response and survival. Human papillomavirus (HPV) status was measured by p16INK4a immunohistochemistry in oropharyngeal tumours. Clinicopathological features and response to
treatment were measured and compared with the sequencing results. The results indicated _TP53_ as the most mutated gene in locally advanced HNSCC. HPV-positive oropharyngeal tumours were
less mutated than HPV-negative tumours in _TP53_ (p < 0.01). Mutational and HPV status influences patient survival, being mutated or HPV-negative tumours associated with poor overall
survival (p < 0.05). No association was found between mutations and clinicopathological features. This study confirmed and expanded previously published genomic characterization data in
HNSCC. Survival analysis showed that non-mutated HNSCC tumours associated with better prognosis and lack of mutations can be identified as an important biomarker in HNSCC. Frequent
alterations in PI3K pathway in HPV-positive HNSCC could define a promising pathway for pharmacological intervention in this group of tumours. SIMILAR CONTENT BEING VIEWED BY OTHERS TEMPORAL
EVOLUTION AND INTER-PATIENT HETEROGENEITY IN PRIMARY AND RECURRENT HEAD AND NECK SQUAMOUS CELL CARCINOMA Article Open access 29 August 2024 HALLMARKS OF A GENOMICALLY DISTINCT SUBCLASS OF
HEAD AND NECK CANCER Article Open access 20 October 2024 COMPUTATIONAL ANALYSIS OF TP53 MUTATIONAL LANDSCAPE UNVEILS KEY PROGNOSTIC SIGNATURES AND DISTINCT PATHOBIOLOGICAL PATHWAYS IN HEAD
AND NECK SQUAMOUS CELL CANCER Article Open access 20 July 2020 INTRODUCTION Head and neck squamous cell carcinoma (HNSCC) is the sixth most common neoplasia in the developed world1. It
constitutes a heterogeneous disease of tumours of the upper aerodigestive tract with different pathogenic origins and clinical prognosis. Tobacco smoking and alcohol consumption are still
the most classical risk factors2 followed by viral infection3,4. Most HNSCC are diagnosed as locally advanced disease (stage III or IV) and therefore multidisciplinary treatment strategies
include surgery, radiotherapy (RT), chemotherapy (CT) and targeted therapy. However, treatment with chemoradiotherapy (CTRT) has become the standard of care after the publication of a large
pool analysis5. With the aim of improving the clinical benefit, the addition of cetuximab, an IgG1 chimeric monoclonal antibody against epidermal growth factor receptor (EGFR), concomitant
with RT was explored, resulting in longer progression-free survival (PFS) and overall survival (OS) compared to RT alone, although a direct comparison with CTRT has not been evaluated yet6.
The role of induction chemotherapy has remained a subject of controversy. The combination of docetaxel-cisplatin and 5-fluorouracil (TPF) has emerged as the most active regimen in locally
advanced disease, showing better results than PF, although it did not show a convincing survival benefit in induction regimens compared with historical data of treatment with concomitant
chemoradiotherapy alone7,8,9. Induction chemotherapy to improve organ preservation and survival may be an alternative to CTRT. The addition of cetuximab to radiation therapy in patients with
laryngeal cancer stage III and IVA that respond to TPF could improve functional laryngeal preservation10, although randomized phase III trials did not find that induction chemotherapy
provided benefit in time-to-treatment failure or OS11,12,13,14. On the other hand, a randomized phase II–III study suggested that adding TPF induction chemotherapy to CTRT resulted in a
higher rate of radiological complete response compared with concurrent CTRT alone, improving PFS and OS by induction TPF15. The fact that patient populations in these trials were very
heterogeneous, questions induction chemotherapy’s benefit thus, subgroups that will have a benefit from it need to be identified. Next-generation sequencing (NGS) has helped to identify
genetic alterations that could be used as a molecular vulnerability for therapeutic discovery and target optimization. In addition, they could have a prognosis utility as biomarkers of
response in different tumour types including head and neck squamous cell carcinomas16,17. For instance, the analysis of _The Cancer Genome Atlas_ (TCGA) described the molecular landscape of
HPV-positive and HPV-negative HNSCC as having molecular alterations not reported before18. Since the first description of the recurrently mutated genes in HNSCC19, additional studies have
included other genes such as _TP53, NOTCH1, PIK3CA, CDKN2A, CCDN1, HRAS, FAT1, FBXW7_ and _FGFR3,_ among others20,21. For this reason, targeted sequencing has become a flexible tool to study
those genes previously reported as mutated in HNSCC21. To contribute to the understanding of how somatic mutations influence the outcome of HNSCC treatment, we have studied a panel of 26
genes (Table S1) by next-generation sequencing in a homogenously treated locally advanced HNSCC Spanish cohort. In this study we report some mutations linked with detrimental outcome and
their presence in relation to HPV presence. RESULTS COHORT CHARACTERISTICS 234 FFPE blocks with diagnostic biopsies from HNSCC patients within a multicentre phase III clinical trial were
incorporated in this study (Fig. S1). Clinical demographic factors such as age, gender, disease site and tumour stage are consistent between the whole cohort within the clinical trial and
the subsequent random selection due to FFPE block availability in this study. Overall, most were from men (89.7%), with pharyngeal carcinoma (65.4%) and diagnosed in tumour stage IV-A
(71.4%) with an average of 57 years old (Table 1). Clinicopathologic features by locations are shown in Table 1. Considering only oropharyngeal tumours (see “Methods” section), 13 samples
(17.1%) were HPV-positive based on p16 immunohistochemistry (IHC). According to its grade, HPV-positive samples were statistically associated with poorly differentiated (p = 0.016) and
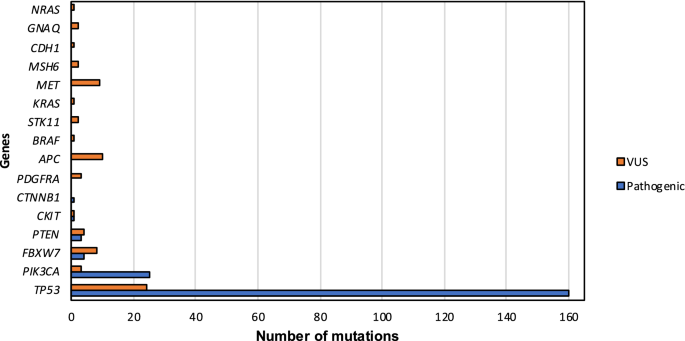
_TP53_ wild-type (p = 0.009) tumours (Table 2). Targeted panel sequencing in HNSCC FFPE blocks identified 162 samples (69.23%) with previously described pathogenic mutations whereas 46
(19.66%) did not carry any mutation and 26 (11.11%) showed variants of uncertain clinical significance (VUS). 194 pathogenic mutations and 72 VUS were found in the sequencing of the 234 FFPE
blocks. All samples were sequenced > 5000 × (7074 ± 10,516). Globally, the most mutated gene was _TP53_ (61.1%) followed by _PIK3CA_ (10.3%), _FBXW7_ (1.7%), _PTEN_ (1.3%) and _CKIT_ and
_CTNNB1_ (both with 0.43%) (Fig. 1). 144 out of 162 (88.89%) mutated tumours had _TP53_ mutations either alone or with others. Most of the pathogenic variants were missense (55.67%),
followed by stop-gained (18.04%), frameshift (14.95%), splice-donor (8.76%) and in-frame deletions (2.58%) (Table S2). ASSOCIATION OF MUTATIONS WITH CLINICAL VARIABLES General comparison of
the mutational status and tumour characteristics such as location, grade and histology, did not show any significant difference (p > 0.05) (Table 3). However, considering variants of
uncertain significance, women were associated with a lower percentage of mutation than men in our cohort (p = 0.002) (Table 3). MUTATIONAL PROFILE AND HPV PRESENCE IN OROPHARYNGEAL TUMOURS
HPV mutational profile in oropharyngeal tumours is shown in Fig. 2. HPV-positive samples presented slightly more pathogenic mutations than HPV-negative (76.2% versus 69.2%, p = 0.762) (Table
2). Despite the fact that _TP53_ was the most frequently mutated gene in both groups, these mutations were more recurrent in HPV-negative tumours (71.4% in HPV-negative and 30.8% in
HPV-positive), difference statistically significant (p = 0.009). Conversely, the second most mutated gene, _PIK3CA,_ although more represented in HPV-positive tumours (9.5% in HPV-negative
versus 23.1% in HPV-positive), did not show any statistically significant difference (p = 0.178). While HPV-negative tumours did not present pathogenic mutations in other genes, _PTEN_ was
the third most commonly mutated in HPV-positive tumours (15.4%), followed by _FBXW7_ (7.7%). MUTATIONAL STATUS AND RESPONSE TO TREATMENT After induction chemotherapy, 188 (80.34%) patients
were similarly randomized: 95 (50.53%) to conventional treatment and 93 (49.47%) to the experimental arm. Preliminary data indicated that the two regimens showed similar survival, response
rates, toxicity and locoregional control22. For that reason, both arms were evaluated within the same group as final response (or response after randomization). Evaluation of the two
time-point responses according to the mutational profile did not show any statistical difference (Table 4). There was, however, a tendency between mutated tumours and complete response at
the end of the treatment taking VUS into consideration, p = 0.096 (Table S3). Considering only HPV profile in oropharyngeal tumours, there were no differences between HPV-positive and
HPV-negative individuals either after induction chemotherapy (p = 0.396) or randomization (p = 0.914) (Table 5). Finally, an exploratory analysis was performed using the two most mutated
genes in the study: _TP53_ and _PIK3CA_ (Table S4). Analysing patients with mutations in those genes alone or within other genes and the clinical response, indicated that none of the _TP53_
subgroups were associated in any of the clinical trial treatment timepoints (p > 0.05). By contrast, considering only _PIK3CA_ mutations, a statistically positive association was found in
the complete response group after induction chemotherapy (p = 0.024). However, this finding was not corroborated in final response group (p = 0.235) (Table S4) what could suggest that this
could be a false positive result taken into consideration multiple testing and sample size bias. Poeta’s23 and Neskey’s24 classification in patients harbouring _TP53_ mutations in relation
with clinical response before and after randomization did not show any statistically significant association (p > 0.05, Table S5). HPV, MUTATIONAL STATUS AND CLINICAL OUTCOME HPV-positive
oropharyngeal tumours showed higher OS compared with HPV-negative (p = 0.044). This tendency was also shown in PFS, however, without statistically significant results (p = 0.148, HR = 0.498
(0.194–1.280)) (Fig. 3A,B). Moreover, OS was correlated with the mutational status. Patients without mutations in the selected genes had a better OS than patients with mutated tumours (p =
0.011, HR = 1.672 (1.123–2.491)) (Fig. 3C). This difference was also observed in PFS without statistically significant results (p = 0.135, HR = 1.349 (0.911–1.999)) (Fig. 3D). A correlation
with the number of mutations also showed that tumours with one mutation had lower OS (p = 0.038, HR = 1.544 (1.025–2.327)) than non-mutated patients, with the exception of PFS (p = 0.259, HR
= 1.264 (0.842–1.898)) (Fig. 3E,F). Equally, tumours with more than one mutation showed lower OS (p = 0.001, HR = 2.524 (1.441–4.422)) and PFS (p = 0.036, HR = 1.824 (1.039–3.203)) than
non-mutated samples. Conversely, the differences between tumours with one or more mutations were not statistically significant (p > 0.05). Finally, we compared _TP53_ mutations based on
Poeta’s23 and Neskey’s24 stratification models with OS and PFS (Fig. S2). No association was observed between low-risk/high risk mutations or non-disruptive/disruptive mutations and survival
in these patients (Fig. S2). DISCUSSION As most of the head and neck cancers are diagnosed at a locally advanced stage the identification of biomarkers of response is a main goal to
optimize treatment and reduce side effects. In recent years, induction chemotherapy has been shown to produce a benefit in organ preservation without a clear improvement in survival. In
addition, this approach led to a high toxicity, particularly when concurrent radiotherapy was given with high doses of cisplatin. At present, very few predictive biomarkers of response have
been described. For this reason, we proposed a study of the mutational status in 26 of the most common altered genes in cancer with next-generation sequencing in a homogeneously treated
representative Spanish cohort of HNSCC from the phase III clinical trial TTCC-2007-0122. The epidemiology characteristics of the HNSCC patients included in our study were similar to other
series reported from the same region: the ratio between sexes is 9:1 in detriment of men, and most of the patients were diagnosed at stage IV25. p16 IHC, a surrogate of HPV infection in
oropharyngeal tumours, showed that HPV was present in 17.1% of samples, a lower percentage than previously reported in Europe26 but with similar location to other Southern European countries
in oropharynx27. Globally, the most mutated gene in our series was _TP53_ (61.1%). We observed a statistically significant lower percentage of mutated _TP53_ in HPV-positive oropharyngeal
tumours (71.4%) than in HPV-negative (30.8%) as has been previously reported in HNSCC28,29. These results could be explained if _TP53_ sequestration by the viral oncoprotein E6 prevents
gaining mutations in this gene under selective pressure of30,31. Comparing to other series, there was a higher percentage of _TP53_ mutations in HPV-positive tumours29. This fact could be
explained by the coexistence of viral infection and other aetiological factors such as tobacco smoking and alcohol consumption during tumourigenesis32; these data were not collected in this
study. TCGA data described 85% of _TP53_ mutation in HPV-negative tumours and only 3% in HPV-positive ones18. However, the sample population was very different with a high predominance of
oral cavity tumours (62%) and mainly heavy smokers. _PI3K/AKT/mTOR_ has been reported as the most mutated pathway in HNSCC (13% to 56%), regardless of the HPV status18. _PIK3CA_ gene, that
encodes the catalytic subunit of the family, has been reported with an average mutational rate of 10.53% in HNSCC33, similar to the 10.25% found in this cohort, and with a higher frequency
in laryngeal tumours34. Mutations in this gene have also been related to HPV-positive tumours4. Our results corroborate this fact, being _PIK3CA_ more frequently mutated in HPV-positive
tumours (23.1% versus 9.5% in HPV-negative oropharyngeal tumours), similar to previously described data35. We did not, however, see an increased percentage in laryngeal carcinoma. 73% of the
mutations in _PIK3CA_ are commonly located in 3 hotspots (E542K, E545K and H1047R/L)36, result also found in 76% of _PIK3CA_ mutated samples in our study, emphasising the accuracy of using
the targeted panel in HNSCC. Mutations in _FBXW7_: an E3 ubiquitin ligase member of the F-box protein family, have been previously observed in HNSCC19. This tumour suppressor gene targets
_NOTCH1_, being an important protein in cell proliferation control. Previous studies found _FBXW7_ mutated in 5% of HNSCC37,38 and a higher percentage of mutations was previously considered
as a prevalent event in HPV-positive tumours39. Our cohort confirmed these results in _FBXW7_ with a similar percentage only found in HPV-positive tumours (7.7%). _PTEN_ was the third most
mutated gene in 15.4% of the HPV-positive oropharyngeal tumours while not mutations were found in HPV-negative ones. Contrary to our results, TCGA study showed _PTEN_ mutated in 12% of
HPV-negative tumours and 6% of HPV-positive18. Apart from _PTEN_, there were other genes which mutated at a lower percentage in our series, such as _CKIT_ or _CTNNB1_ (both mutated at less
than 1% and only in non-oropharyngeal HPV-negative tumours)_,_ have been reported in HNSCC in varied percentages30,38,40. Together with _PIK3CA_, our result enhances the hypothesis of higher
prevalence of PI3K pathway activated mutations in HPV-positive tumours41. Overall, excluding _TP53_ mutations, recurrent alterations in _PIK3CA, PTEN_ and _FBXW7_ genes, all belonging to
the _PI3K/AKT/mTOR_ pathway, could define a potential new target for pharmacological intervention in HNSCC, as it has been suggested in other publications42. In terms of survival,
HPV-positive oropharyngeal tumours were associated with better prognosis, showing an increased OS and PFS compared to HPV-negative tumours as it was previously defined26,43,44,45,46,47.
Secondly, the presence of mutation in the targeted genes was associated with inferior outcome demonstrated by the presence of detrimental OS. These results could be an indirect measure of
tumour aggressiveness, as has been reported in other series43,47. Moreover, the fact that carriers of tumours with more than one mutation have lower OS than those with non-mutated tumours
reinforces this concept. Lastly, there was a lack of association between mutational status and response after treatment. This can indicate that, excluding genetic-driven druggable targets,
HNSCC mutational profile is not related to any clinical response but is a matter of mutational burden as is shown in the survival analyses. Similarly, there was no association between _TP53_
mutations stratified by Poeta’s23 and Neskey’s models24 and response to treatment or survival. These classification systems can serve as an important tool in individualizing and improving
treatment for high TP53 mutated tumours, as it was previously identified in a subset of high-risk patients with a decreased response to platinum-based therapies48. Nevertheless, these
classification models did not have any implication on outcome in our cohort. Overall, our data strongly support and expand previously published studies exploring the presence and prognosis
of mutations in this population. We have characterized the mutational profile of HPV-positive/HPV-negative oropharyngeal HNSCC in a representative cohort of patients. In this context apart
from _TP53_ mutations, frequent alterations in _PIK3CA, PTEN_ and _FBXW7_ genes, define possible pathways for pharmacological intervention. Finally, survival analysis showed that mutational
status in the tumour could define patient prognosis, and may potentially be used as biomarkers to stratify patients for more intensive treatment. However, larger studies should be performed
to confirm these results aiming at stratifying patients to different therapeutic interventions. METHODS SAMPLES 234 FFPE blocks with diagnostic biopsies from HNSCC patients were included in
this study. A consort diagram reporting the dropout is shown in Fig. S1. All samples belong to the clinical trial TTCC-2007-01 entitled: “Open label randomized, multi-centre phase III trial
of TPF plus concomitant treatment with cisplatin and radiotherapy versus concomitant cetuximab and radiotherapy in locally advanced, unresectable head and neck cancer”, ClinicalTrials.gov
identifier: NCT0071639122. TTCC-2007-01 TRIAL DESIGN AND DATA COLLECTION It was a non-inferiority, randomized and controlled study with a parallel assignment intervention model and an
endpoint of safety/efficacy, carried out between 2008 and 2013. The follow-up of the clinical trial finished in November 2016. According to protocol, written informed consent was obtained
from living subjects and the protocol was approved by the University Hospital of Salamanca and the ethical committees of each hospital in accordance with the 1964 Helsinki declaration and
its later amendments. Eligible patients: histologically or cytologically confirmed, previously untreated unresectable locally advanced (Stage III–IV) tumours (from oral cavity, oropharynx,
larynx, hypopharynx), ECOG performance status 0–1. Unresectable disease was determined by Northern California Oncology Group in measurable disease. Treatment: docetaxel, cisplatin,
5-fluorouracil (TPF)-based induction chemotherapy (T 75 mg/m2 d1, P 75 mg/m2 d1, F 750 mg/m2 CI d 1–5 q 21 d + G-CSF & ciprofloxacin, by 3 cycles; then, if objective response achieved,
they were randomized to: conventional radiotherapy (RT) up to 70 Gy + P 100 mg/m2 d 1–22–43 vs conventional RT up to 70 Gy + cetuximab 400/250 mg/m2 weekly until the completion of RT, and
they were stratified by primary tumour site. Surgery after RT (neck dissection) was allowed. The primary endpoint was non-inferiority of cetuximab-radiotherapy versus cisplatin-radiotherapy
in terms of overall survival. Response rate, loco-regional control and toxicity in both arms were considered secondary objectives. Preliminary data of this trial did not show any difference
in terms of survival or response rates, toxicity and loco-regional control as secondary end points in the two regimens22. Clinical data were compiled in a case report form by medical
oncologists involved in the clinical trial. All data were treated with the security measures established in compliance with the Protection of Personal Data Organic Law 15/1999, 13th
December, and safe-keeping at the University Hospital of Salamanca in its specific server. DNA EXTRACTION Percentage of tumour cells was measured in haematoxylin–eosin tissue sections by
central pathologist. Between four and ten 10 µm FFPE sections from diagnosis blocks were treated with deparaffinization solution (Qiagen, Hilden, Germany) and DNA extraction was done using
QIAamp DNA FFPE Tissue kit (Qiagen, Hilden, Germany). DNA QUALITY EVALUATION AND TARGETED NGS Following TruSight Tumor 26 Reference Guide (Illumina, San Diego, USA), DNA quality was measured
by qPCR. Comparing FFPE-gDNA amplification potential with a reference non-FFPE gDNA (QCT), delta Cq value was used to predict the dilution required for each sample. TruSight Tumor 26 panel
includes a set of 174 amplicons in complete exons of 26 cancer-associated genes (Table S1). This panel was selected due to its exceptional success rate using minimal DNA input even from FFPE
samples where genetic material is often degraded. Following steps of hybridization with the oligo pool, removing unbound oligos and extension and ligation with bound oligos, an
amplification of the libraries were performed. PCR products were checked on a 4% TBE agarose gel and finally the libraries were cleaned up by AMPure XP magnetic beads (Beckman Coulter, Brea,
CA, USA). PCR products were quantified using Qubit Fluorometer (Invitrogen, Carlsbad, CA, USA) and libraries were normalized at 4 nM in a final pool. Sequencing was performed in a NextSeq
500 System (Illumina, San Diego, USA). Data were transformed in BaseSpace platform and the VCF file format were read in the Variant Studio Software (Illumina, San Diego, USA). Following
Illumina recommendations, somatic variants over 5% of frequency, with yields at least 1000 × cumulative coverage between the 2 strands and considered from the software of PASS filter were
reported. Those variants of uncertain significance were considered pathogenic if at least two in silico prediction tools (SIFT and PolyPhen) classified them as deleterious/probably
damaging49, and they were defined as likely pathogenic in the Catalogue Of Somatic Mutations in Cancer (COSMIC; https://cancer.sanger.ac.uk/cosmic) or the National Center for Biotechnology
Information (NCBI; https://www.ncbi.nlm.nih.gov/clinvar) databases. ASSESSMENT OF HPV STATUS In the original study protocol, the assessment of HPV status was carried out by p16
immunohistochemistry (IHC), a surrogate marker for HPV infection50 as the gold-standard technique. FFPE sections were deparaffinized and exposed to 10 mM citrate buffer antigen retrieval at
92 °C for 30 min and then they were stained using a p16INK4a mouse monoclonal antibody (Cell Marque, Rocklin, CA, USA). Percentage of p16 staining was measured and only those tumours >
70% nuclear and cytoplasmic p16+ were considered positive. 33 samples were considered HPV-positive following this methodology: 13 oropharyngeal, 4 hypopharyngeal, 2 laryngeal and 9 oral
cavity tumours. However, after the publication of the guidelines from the college of American pathologists, p16 IHC is only recommended in oropharyngeal tumours but other locations, where
DNA/RNA viral determination should be performed as a confirmatory test51. Since there was not more DNA from all the samples after the library preparation, only oropharyngeal tumours with
> 70% p16 positive staining were considered HPV-positive. STATISTICAL ANALYSES Statistical analysis compared categorical parameters and mutational status by the Chi-square or Fisher’s
exact tests; while in continuous nonparametric variables, the Mann–Whitney U or Kruskal–Wallis H tests were used. p-values were calculated excluding missing values and they were considered
statistically significant when p < 0.05. Significant variables were included in the logistic regression analysis and size effects were indicated by odds ratio (OR) with their 95%
confidence interval (95% CI). Mutational status was classified as presence or absence of mutations, number of mutations (none, one or more than one) and the status of _TP53_ and _PIK3CA_
(mutant or wild-type). Response was divided in two groups of treatment: after induction chemotherapy and after chemo/cetuximab plus radiotherapy (final response) due to the similar outcome
in both arms22. Response was classified in both groups as complete response versus partial response/stabilization. No progressions were shown in the cohort. Survival analysis was done
according to the overall survival (OS) and progression-free survival (PFS) by Kaplan–Meier plots and log-rank test p-values were calculated in all the curves. Median was indicated in those
plots in which it was achieved. Hazard-ratio was calculated to measure the risk of the event with its 95% confidence interval (95% CI) by Cox regression. Median follow-up in OS was 32.23
months while in PFS it was 15.31 months. Due to high prevalence in _TP53_ mutations, we applied Poeta’s and Neskey’s classifications stratifying the mutations according to its change and
functional effect, allowing a better comprehensive understanding on their relevance in clinical outcome. Following Poeta’s classification23, _TP53_ mutations were divided in two categories:
disruptive and non-disruptive according to their functional effects on the p53 protein. Additionally, according to Neskey’s model24, also named as Evolutionary Action score of _TP53_-coding
variants (EAp53), missense mutations were stratified into high-risk and low-risk through an _in-silico_ scoring (https://mammoth.bcm.tmc.edu/EAp53/). Then, comparative analysis was performed
in response to treatment, OS and PFS. All these tests were conducted using SPSS software version 21.0 (SPSS Inc., Chicago) and GraphPad Prism software version 6.0 (GraphPad Software Inc.,
California). REFERENCES * Siegel, R. L., Miller, K. D. & Jemal, A. Cancer Statistics, 2019. _CA Cancer J. Clin._ https://doi.org/10.3322/caac.21551 (2019). Article PubMed Google
Scholar * Sturgis, E. M., Wei, Q. & Spitz, M. R. Descriptive epidemiology and risk factors for head and neck cancer. _Semin. Oncol._ 31, 726–733 (2004). Article PubMed Google Scholar
* Leemans, C. R., Braakhuis, B. J. M. & Brakenhoff, R. H. The molecular biology of head and neck cancer. _Nat. Rev. Cancer_ 11, 9–22 (2011). Article CAS PubMed Google Scholar *
Lechner, M. _et al._ Targeted next-generation sequencing of head and neck squamous cell carcinoma identifies novel genetic alterations in HPV+ and HPV-tumors. _Genome Med._ 5, 49 (2013).
Article PubMed PubMed Central Google Scholar * Pignon, J. P., le Maître, A., Maillard, E., Bourhis, J. & MACH-NC Collaborative Group. Meta-analysis of chemotherapy in head and neck
cancer (MACH-NC): An update on 93 randomised trials and 17,346 patients. _Radiother. Oncol._ 92(1), 4–14 (2009). Article PubMed Google Scholar * Bonner, J. A. _et al._ Radiotherapy plus
cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. _Lancet Oncol._
11, 21–28 (2010). Article CAS PubMed Google Scholar * Blanchard, P. _et al._ Taxane-cisplatin-fluorouracil as induction chemotherapy in locally advanced head and neck cancers: An
individual patient data meta-analysis of the meta-analysis of chemotherapy in head and neck cancer group. _J. Clin. Oncol._ 31, 2854–2860 (2013). Article CAS PubMed Google Scholar *
Posner, M. R. M. D. _et al._ Cisplatin and fluorouracil alone or with docetaxel in head and neck cancer. _N. Engl. J. Med._ 357, 1705–1715 (2007). Article ADS CAS PubMed Google Scholar
* Lorch, J. H. _et al._ Induction chemotherapy with cisplatin and fluorouracil alone or in combination with docetaxel in locally advanced squamous-cell cancer of the head and neck: Long-term
results of the TAX 324 randomised phase 3 trial. _Lancet Oncol._ 12, 153–159 (2011). Article CAS PubMed PubMed Central Google Scholar * Mesía, R. _et al._ Could the addition of
cetuximab to conventional radiation therapy improve organ preservation in those patients with locally advanced larynx cancer who respond to induction chemotherapy? An organ preservation
Spanish head and neck cancer cooperative group. _Int. J. Radiat. Oncol._ 97, 473–480 (2016). Article CAS Google Scholar * Cohen, E. E. W. _et al._ Phase III randomized trial of induction
chemotherapy in patients with N2 or N3 locally advanced head and neck cancer. _J. Clin. Oncol._ 32, 2735–2743 (2014). Article CAS PubMed PubMed Central Google Scholar * Hitt, R. _et
al._ A randomized phase III trial comparing induction chemotherapy followed by chemoradiotherapy versus chemoradiotherapy alone as treatment of unresectable head and neck cancer. _Ann.
Oncol._ 25, 216–225 (2014). Article CAS PubMed Google Scholar * Haddad, R. _et al._ Induction chemotherapy followed by concurrent chemoradiotherapy (sequential chemoradiotherapy) versus
concurrent chemoradiotherapy alone in locally advanced head and neck cancer (PARADIGM): A randomised phase 3 trial. _Lancet Oncol._ 14, 257–264 (2013). Article CAS PubMed Google Scholar
* Geoffrois, L. _et al._ Induction docetaxel platinum 5-FU (TPF) followed by cetuximab-radiotherapy (cetux-RT) versus concurrent chemo-radiotherapy (CT/RT) in patients with N2b/c-N3 non
operated stage III-IV squamous cell cancer of the head and neck (SCCHN): Results of the GORTEC 2007–02 phase III randomized trial. _J. Clin. Oncol._ 34(Suppl), 6000 (2016). Article Google
Scholar * Ghi, M. G. _et al._ Concomitant chemoradiation (CRT) or cetuximab/RT (CET/RT) versus induction Docetaxel/ Cisplatin/5-Fluorouracil (TPF) followed by CRT or CET/RT in patients with
locally advanced squamous cell carcinoma of head and neck (LASCCHN). A randomized phase III fac. _J. Clin. Oncol._ 32, 6004–6004 (2014). Article Google Scholar * Rizzo, G., Black, M.,
Mymryk, J. S., Barrett, J. W. & Nichols, A. C. Defining the genomic landscape of head and neck cancers through next-generation sequencing. _Oral Dis._ 21, e11–e24 (2015). Article CAS
PubMed Google Scholar * Stransky, N. _et al._ The mutational landscape of head and neck squamous cell carcinoma. _Science_ 333, 1157–1160 (2011). Article ADS CAS PubMed PubMed Central
Google Scholar * Network, T. C. G. A. Comprehensive genomic characterization of head and neck squamous cell carcinomas. _Nature_ 517, 576–582 (2015). Article ADS CAS Google Scholar *
Agrawal, N. _et al._ Exome sequencing of head and neck squamous cell carcinoma reveals inactivating mutations in NOTCH1. _Science_ 333, 1154–1157 (2011). Article ADS CAS PubMed PubMed
Central Google Scholar * Sun, W. & Califano, J. A. Sequencing the head and neck cancer genome: Implications for therapy. _Ann. N. Y. Acad. Sci._ 1333, 33–42 (2014). Article ADS CAS
PubMed PubMed Central Google Scholar * Tabatabaeifar, S., Kruse, T. A., Thomassen, M., Larsen, M. J. & Sørensen, J. A. Use of next generation sequencing in head and neck squamous cell
carcinomas: A review. _Oral Oncol._ 11, 1035–1040 (2014). Article CAS Google Scholar * Hitt, R., Mesia, R. & Grau, J. Randomized phase III trial of induction chemotherapy (ICT) with
docetaxel-cisplatin-5fluorouracil (DCF) followed by cisplatin-radiotherapy (CRT) or cetuximab-radiotherapy (CetRT) in patients (pts) with locally advanced unresectable head and neck cancer.
_J. Clin. Oncol._ 34, 6001 (2016). Article Google Scholar * Luana Poeta, M. _et al._ TP53 mutations and survival in squamous-cell carcinoma of the head and neck. _N. Engl. J. Med._ 25,
2552–2561 (2007). Article Google Scholar * Neskey, D. M. _et al._ Evolutionary action score of TP53 identifies high-risk mutations associated with decreased survival and increased distant
metastases in head and neck cancer. _Cancer Res._ 7, 1527–1536 (2015). Article CAS Google Scholar * Seijas-Tamayo, R. _et al._ Epidemiological characteristics of a Spanish cohort of
patients diagnosed with squamous cell carcinoma of head and neck: Distribution of risk factors by tumor location. _Clin. Transl. Oncol._ 18, 1114–1122 (2016). Article CAS PubMed Google
Scholar * D’Souza, G. _et al._ Effect of HPV on head and neck cancer patient survival, by region and tumor site: A comparison of 1362 cases across three continents. _Oral Oncol._ 62, 20–27
(2016). Article PubMed PubMed Central Google Scholar * Baboci, L. _et al._ Low prevalence of HPV-driven head and neck squamous cell carcinoma in North-East Italy. _Papillomavirus Res._
2, 133–140 (2016). Article PubMed PubMed Central Google Scholar * Gaykalova, D. A. _et al._ Novel insight into mutational landscape of head and neck squamous cell carcinoma. _PLoS ONE_
9, 1–9 (2014). Article CAS Google Scholar * Westra, W. H. _et al._ Inverse relationship between human papillomavirus-16 infection and disruptive p53 gene mutations in squamous cell
carcinoma of the head and neck. _Clin. Cancer Res._ 14, 366–369 (2008). Article CAS PubMed Google Scholar * Chung, C. H. _et al._ Genomic alterations in head and neck squamous cell
carcinoma determined by cancer gene-targeted sequencing. _Ann. Oncol._ 26, 1216–1223 (2015). Article CAS PubMed PubMed Central Google Scholar * Chung, C. H. & Gillison, M. L. Human
papillomavirus in head and neck cancer: Its role in pathogenesis and clinical implications. _Clin. Cancer Res._ 15, 6758–6762 (2009). Article CAS PubMed Google Scholar * Zevallos, J. P.
_et al._ Molecular profile of human papillomavirus positive oropharyngeal squamous cell carcinoma stratified by smoking status. _Int. J. Radiat. Oncol. Biol. Phys._ 94, 864 (2016). Article
Google Scholar * Mountzios, G., Rampias, T. & Psyrri, A. The mutational spectrum of squamous-cell carcinoma of the head and neck: Targetable genetic events and clinical impact. _Ann.
Oncol._ 25, 1889–1900 (2014). Article CAS PubMed Google Scholar * Tabatabaeifar, S., Kruse, T. A., Thomassen, M., Larsen, M. J. & Sørensen, J. A. Use of next generation sequencing in
head and neck squamous cell carcinomas: A review. _Oral Oncol._ 50, 1035–1040 (2014). Article CAS PubMed Google Scholar * Seiwert, T. Y. _et al._ Integrative and comparative genomic
analysis of HPV-positive and HPV-negative head and neck squamous cell carcinomas. _Clin. Cancer Res._ 21, 632–641 (2015). Article CAS PubMed Google Scholar * Lui, V. W. _et al._ Frequent
mutation of the PI3K pathway in head and neck cancer defines predictive biomarkers. _Cancer Discov._ 3, 761–769 (2013). Article CAS PubMed PubMed Central Google Scholar * van Ginkel,
J. H., de Leng, W. W. J., de Bree, R., van Es, R. J. J. & Willems, S. M. Targeted sequencing reveals TP53 as a potential diagnostic biomarker in the post-treatment surveillance of head
and neck cancer. _Oncotarget_ 7, 61575 (2016). Article PubMed PubMed Central Google Scholar * Er, T.-K. _et al._ Molecular characterization of oral squamous cell carcinoma using targeted
next generation sequencing. _Oral Dis._ 7, 872–878 (2015). Article Google Scholar * Rusan, M., Li, Y. Y. & Hammerman, P. S. Genomic landscape of human papillomavirus-associated
cancers. _Clin. Cancer Res._ 21, 2009–2019 (2015). Article CAS PubMed PubMed Central Google Scholar * Saba, N. F. _et al._ Mutation and transcriptional profiling of formalin-fixed
paraffin embedded specimens as companion methods to immunohistochemistry for determining therapeutic targets in oropharyngeal squamous cell carcinoma (OPSCC): A pilot of proof of principle.
_Head Neck Pathol._ 9, 223–235 (2015). Article PubMed Google Scholar * Simon, C. _et al._ PIK3CA, HRAS and PTEN in human papillomavirus positive oropharyngeal squamous cell carcinoma.
_BMC Cancer_ 13, 602 (2013). Article CAS Google Scholar * Saada-Bouzid, E. & Le Tourneau, C. Beyond EGFR targeting in SCCHN: Angiogenesis, PI3K, and other molecular targets. _Front.
Oncol._ 9, 74 (2019). Article PubMed PubMed Central Google Scholar * Verri, C. _et al._ Mutational profile from targeted NGS predicts survival in LDCT screening-detected lung cancers.
_J. Thorac. Oncol._ 6, 922–931 (2017). Article Google Scholar * Coordes, A. _et al._ Meta-analysis of survival in patients with HNSCC discriminates risk depending on combined HPV and p16
status. _Eur. Arch. Oto-Rhino-Laryngol._ 273, 2157–2169 (2016). Article Google Scholar * Dayyani, F. _et al._ Meta-analysis of the impact of human papillomavirus (HPV) on cancer risk and
overall survival in head and neck squamous cell carcinomas (HNSCC). _Head Neck Oncol._ 2, 15 (2010). Article PubMed PubMed Central Google Scholar * Ragin, C. C. R. & Taioli, E.
Survival of squamous cell carcinoma of the head and neck in relation to human papillomavirus infection: Review and meta-analysis. _Int. J. Cancer_ 121, 1813–1820 (2007). Article CAS PubMed
Google Scholar * Dubot, C. _et al._ Comprehensive genomic profiling of head and neck squamous cell carcinoma reveals FGFR1 amplifications and tumour genomic alterations burden as
prognostic biomarkers of survival. _Eur. J. Cancer_ 91, 47–55 (2018). Article ADS CAS PubMed Google Scholar * Osman, A. _et al._ Evolutionary action score of TP53 coding variants is
predictive of platinum response in head and neck cancer patients. _Cancer Res._ 7, 1205–1215 (2015). Article CAS Google Scholar * Tavtigian, S. V., Greenblatt, M. S., Lesueur, F. &
Byrnes, G. B. In silico analysis of missense substitutions using sequence-alignment based methods. _Hum. Mutat._ 29, 1327–1336 (2008). Article CAS PubMed PubMed Central Google Scholar *
Thomas, J. & Primeaux, T. Is p16 immunohistochemistry a more cost-effective method for identification of human papilloma virus-associated head and neck squamous cell carcinoma?. _Ann.
Diagn. Pathol._ 16, 91–99 (2012). Article PubMed Google Scholar * Lewis, J. S. _et al._ Human papillomavirus testing in head and neck carcinomas: Guideline from the College of American
Pathologists. _Arch. Pathol. Lab. Med._ 142, 559–597 (2018). Article PubMed Google Scholar Download references ACKNOWLEDGEMENTS Authors would like to thank the individuals who consented
to participate in this study and their relatives, and all their colleagues from the Spanish Group of Treatment of Head and Neck Cancer (TTCC) who have participated in this study and are not
included in the list of authors. We would also like to thank the pathologist technician María del Carmen Rodríguez for its implication in the study, Dr Eva Maria Sánchez Tapia and Dr Elena
Bueno-Martínez for technical support; and Roger Townsend for English editing. FUNDING This research was funded by the health research program of the “Instituto de Salud Carlos III”
(PI14/00071) co financed with FEDER founds and for the Health Regional Management of the Junta de Castilla y León (GRS1385/A/16). J. Fernández-Mateos was partially supported by a predoctoral
research grant from the Consejería de Educación—Junta de Castilla y León and the European Social Fund to CC-B (EDU/1084/2012). AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Medical Oncology
Service, University Hospital of Salamanca-IBSAL, 37007, Salamanca, Spain Javier Fernández-Mateos, Raquel Seijas-Tamayo, Juan Carlos Adansa Klain, Edel del Barco & Juan Jesús
Cruz-Hernández * Biomedical Research Institute of Salamanca (IBSAL), SACYL-University of Salamanca-CSIC, 37007, Salamanca, Spain Javier Fernández-Mateos, Raquel Seijas-Tamayo, Juan Carlos
Adansa Klain, Edel del Barco, Rogelio González-Sarmiento & Juan Jesús Cruz-Hernández * Molecular Medicine Unit-IBSAL, Department of Medicine, University of Salamanca, 37007, Salamanca,
Spain Javier Fernández-Mateos, Jéssica Pérez-García, Rogelio González-Sarmiento & Juan Jesús Cruz-Hernández * Institute of Molecular and Cellular Biology of Cancer (IBMCC), University of
Salamanca-CSIC, 37007, Salamanca, Spain Javier Fernández-Mateos, Jéssica Pérez-García, Rogelio González-Sarmiento & Juan Jesús Cruz-Hernández * Medical Oncology Department, Institut
Català d’Oncologia, L’Hospitalet de Llobregat, Universitat de Barcelona, IDIBELL, 08908, Barcelona, Spain Ricard Mesía, Miren Taberna & Silvia Vazquez * Medical Oncology Service,
Institut Català d’Oncologia, 17007, Gerona, Spain Jordi Rubió-Casadevall * Medical Oncology Service, Hospital Universitario de Burgos, 09006, Burgos, Spain Carlos García-Girón * Medical
Oncology Service, Hospital Universitario 12 de Octubre, 28041, Madrid, Spain Lara Iglesias * Medical Oncology Service, Hospital Universitario Lucus Augusti, 27003, Lugo, Spain Alberto Carral
Maseda * Pathologist Service, University Hospital of Salamanca, 37007, Salamanca, Spain María Asunción Gómez * Hospital Clínico San Carlos, IdISSC, CIBERONC, 28040, Madrid, Spain Alberto
Ocana * Centro Regional de Investigaciones Biomédicas, Universidad de Castilla La Mancha, 13071, Albacete, Spain Alberto Ocana Authors * Javier Fernández-Mateos View author publications You
can also search for this author inPubMed Google Scholar * Jéssica Pérez-García View author publications You can also search for this author inPubMed Google Scholar * Raquel Seijas-Tamayo
View author publications You can also search for this author inPubMed Google Scholar * Ricard Mesía View author publications You can also search for this author inPubMed Google Scholar *
Jordi Rubió-Casadevall View author publications You can also search for this author inPubMed Google Scholar * Carlos García-Girón View author publications You can also search for this author
inPubMed Google Scholar * Lara Iglesias View author publications You can also search for this author inPubMed Google Scholar * Alberto Carral Maseda View author publications You can also
search for this author inPubMed Google Scholar * Juan Carlos Adansa Klain View author publications You can also search for this author inPubMed Google Scholar * Miren Taberna View author
publications You can also search for this author inPubMed Google Scholar * Silvia Vazquez View author publications You can also search for this author inPubMed Google Scholar * María
Asunción Gómez View author publications You can also search for this author inPubMed Google Scholar * Edel del Barco View author publications You can also search for this author inPubMed
Google Scholar * Alberto Ocana View author publications You can also search for this author inPubMed Google Scholar * Rogelio González-Sarmiento View author publications You can also search
for this author inPubMed Google Scholar * Juan Jesús Cruz-Hernández View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS All authors have read
and agree to the published version of the manuscript. Conceptualization, R.S.T., R.G.S. and J.J.C.H.; methodology, J.F.M. and J.P.G.; validation, J.F.M. and J.P.G.; formal analysis, J.F.M.
and A.O.; investigation, J.F.M., J.P.G., R.S.T, R.M., J.R.C., C.G.G., L.I., A.C.M., J.C.A.K., M.T., S.V., M.A.G. and E.D.B. ;resources, J.F.M., J.P.G, R.S.T, R.M., J.R.C., C.G.G., L.I.,
A.C.M., J.C.A.K., M.T., S.V., M.A.G., E.D.B., J.J.C.H. and R.G.S.; data curation, J.F.M., J.P.G. and R.S.T.; writing—original draft preparation, J.F.M., A.O., R.G.S. and J.J.C.H.;
writing—review and editing, all authors; visualization, J.F.M., A.O., R.G.S. and J.J.C.H.; supervision, R.G.S. and J.J.C.H.; project administration, .G.S. and J.J.C.H.; funding acquisition,
.G.S. and J.J.C.H. CORRESPONDING AUTHORS Correspondence to Rogelio González-Sarmiento or Juan Jesús Cruz-Hernández. ETHICS DECLARATIONS COMPETING INTERESTS J.J.C.H. declares conflict of
interest in advisory role: Merck, MSD, BMS, Novartis and conferences with fee: Merck, BMS, MSD, Roche, Astra Zeneca, Novartis. However, the funders had no role in the design of the study; in
the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results. The rest of the authors declare no competing interest.
ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION
SUPPLEMENTARY INFORMATION 1. SUPPLEMENTARY INFORMATION 2. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which
permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to
the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless
indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory
regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Fernández-Mateos, J., Pérez-García, J., Seijas-Tamayo, R. _et al._ Oncogenic driver
mutations predict outcome in a cohort of head and neck squamous cell carcinoma (HNSCC) patients within a clinical trial. _Sci Rep_ 10, 16634 (2020).
https://doi.org/10.1038/s41598-020-72927-2 Download citation * Received: 05 April 2020 * Accepted: 13 August 2020 * Published: 06 October 2020 * DOI:
https://doi.org/10.1038/s41598-020-72927-2 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative