Play all audios:
ABSTRACT This study aimed to assess the diagnostic accuracy and safety of CT-guided percutaneous core needle biopsy (PCNB) with a coaxial needle for the diagnosis of lung cancer in patients
with an usual interstitial pneumonia (UIP) pattern of interstitial lung disease. This study included 70 patients with UIP and suspected to have lung cancer. CT-guided PCNB was performed
using a 20-gauge coaxial cutting needle. The diagnostic accuracy, sensitivity, specificity, and percentage of nondiagnostic results for PCNB were determined in comparison with the final
diagnosis. PCNB-related complications were evaluated. Additionally, the risk factors for nondiagnostic results and pneumothorax were analyzed. The overall diagnostic accuracy, sensitivity,
and specificity were 85.7%, 85.5%, and 87.5%, respectively. The percentage of nondiagnostic results was 18.6% (13/70). Two or less biopsy sampling was a risk factor for nondiagnostic results
(_p_ = 0.003). The overall complication rate was 35.7% (25/70), and pneumothorax developed in 22 patients (31.4%). A long transpulmonary needle path was a risk factor for the development of
pneumothorax (_p_ = 0.007). CT-guided PCNB using a coaxial needle is an effective method with reasonable accuracy and an acceptable complication rate for the diagnosis of lung cancer, even
in patients with UIP. SIMILAR CONTENT BEING VIEWED BY OTHERS FEASIBILITY AND SAFETY OF FINE POSITIONING NEEDLE-MEDIATED BREATHING CONTROL IN CT-GUIDED PERCUTANEOUS PUNCTURE OF SMALL
LUNG/LIVER NODULES ADJACENT TO DIAPHRAGM Article Open access 09 February 2021 IMPACT OF QUANTITATIVE PULMONARY EMPHYSEMA SCORE ON THE RATE OF PNEUMOTHORAX AND CHEST TUBE INSERTION IN
CT-GUIDED LUNG BIOPSIES Article Open access 03 July 2020 INCIDENCE AND RISK FACTORS FOR PULMONARY HEMORRHAGE AFTER PERCUTANEOUS CT-GUIDED PULMONARY NODULE BIOPSY: AN OBSERVATIONAL STUDY
Article Open access 28 March 2024 INTRODUCTION Usual interstitial pneumonia (UIP) is a histological and radiological pattern of interstitial lung disease (ILD). Although a UIP pattern is a
hallmark of idiopathic pulmonary fibrosis (IPF), it can appear not only in IPF but also in other ILDs (e.g., ILD caused by collagen vascular disease, hypersensitivity pneumonitis, and
asbestosis)1. The prognosis of IPF is notably poor, and the overall median survival has been estimated as 3 years. Also, in patients with fibrosing ILDs other than IPF, UIP pattern is
associated with more rapid disease progression and poorer prognosis2,3,4,5. This condition is also reportedly associated with a high risk of lung cancer; the incidence of lung cancer among
patients with IPF is approximately 22.9 per 10,000 person-years6. Furthermore, patients with both lung cancer and IPF have poor prognosis and difficulty in proper management due to surgical
morbidity and respiratory complication such as drug induced pneumonitis and acute exacerbation of IPF7,8. Patients with IPF regularly undergo chest CT for evaluation of disease progression
and for the risk of developing lung cancer. In patients suspected of having lung cancer, histological confirmation is needed for accurate diagnosis and proper management. Percutaneous
CT-guided lung biopsy is a well-established technique for the diagnosis of lung cancer with a high diagnostic accuracy (83%–97%) and an acceptable complication rate
(22%–51%)9,10,11,12,13,14,15. However, CT-guided lung biopsy in patients with UIP is challenging because of the patients’ impaired pulmonary function and high risk of pneumothorax16. Owing
to the underlying lung fibrosis in patients with UIP, re-expansion of the lung is limited and may require chest tube drainage more frequently and for longer duration than for patients
without UIP16. A recent study evaluated the diagnostic accuracy of CT-guided percutaneous lung biopsy (fine-needle aspiration and core needle biopsy) in patients with a UIP/IPF pattern. The
authors reported that CT-guided percutaneous lung biopsy had a reasonable accuracy, but showed a relatively high complication rate (51%) in patients with a UIP/IPF pattern17. Compared with
fine-needle aspiration, percutaneous core needle biopsy (PCNB) achieves a comparably high diagnostic accuracy for the diagnosis of lung cancer18. In addition, several studies have reported
that using a coaxial cutting needle could improve diagnostic accuracy15,19 and reduce the pneumothorax rate20. As the use of a coaxial needle can avoid repeated traversal of the pleura, a
coaxial needle would be a better choice in patients with IPF who are at high risk for pneumothorax. However, no previous study has described the diagnostic performance of CT-guided PCNB
using a coaxial cutting needle in patients with UIP. Thus, the purpose of our study was to assess the diagnostic accuracy and safety of CT-guided PCNB in patients with a fibrosing ILD with a
UIP pattern by using a coaxial cutting needle system and to identify the predictive factors for nondiagnostic results and pneumothorax. METHODS All procedures were performed in accordance
with the relevant guidelines and regulations14,21. This clinical observational study was approved by our institutional ethics committee and the need for informed consent was waived (Ajou
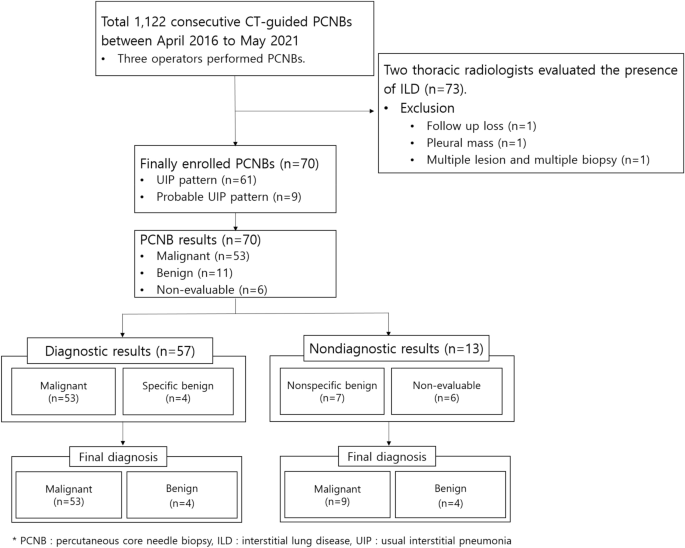
institutional review board). STUDY DESIGN AND PATIENTS A total of 1,122 consecutive CT-guided PCNBs for the diagnosis of lung cancer were performed between April 2016 and May 2021 at a
tertiary referral hospital. Two board-certified radiologists (19 and 3 years of experience in chest radiology) reviewed all diagnostic chest CT images taken before PCNBs and evaluated the
presence of ILD. The diagnostic chest CT scans were performed on various scanners with 16- to 320- channel multidetector CT (Brilliance 16–64, Philips Medical Systems; SOMATOM
Drive/Force/Definition Edge/Definition Flash, Siemens Healthcare; Aquilion ONE, Canon Medical Systems). The scanning parameters were as follow: 0.5-s tube rotation time, collimation:16
\(\times\) 75 mm, pitch: 0.938, 120 kVp, 200 mAs with automatic tube current modulation, 1- and 3-mm slice thickness, and post-processing with high-spatial-frequency algorithm. The
radiologists analyzed the ILD patterns and included patients who had typical UIP CT patterns (honeycombing and reticular pattern with or without traction bronchiectasis) and probable UIP CT
patterns (basal/subpleural predominant reticular pattern and traction bronchiectasis) according to guidelines released in 201822,23. In case of discordance, the same two radiologists had a
discussion until they reached a consensus diagnosis. Accordingly, 73 patients were diagnosed with a UIP pattern of ILD and possible malignant lesions. Of these patients, three were excluded
from this study (follow-up loss [n = 1], pleural mass [n = 1], and multiple biopsies for multiple lesions on one day [n = 1]). Finally, 70 patients (61 patients with typical UIP pattern and
9 patients with probable UIP pattern) who underwent CT-guided PCNB were included in this study. BIOPSY PROTOCOL All patients were admitted prior to biopsy and underwent laboratory tests,
including measurement of platelet count, prothrombin time, and activated prothrombin time as per the institutional protocol. In cases showing abnormalities, a biopsy was performed after
appropriate correction and consultation with a hematologist. One of three board-certified thoracic radiologists (19, 7, and 3 years of experience) performed CT-guided PCNB as a routine daily
procedure. Earlier diagnostic chest CT images were reviewed to determine the optimal biopsy needle path and patient position and predict biopsy-related risks. Before the procedure, written
informed consent was obtained from each patient. CT-guided PCNB was performed using a 16- or 320-channel scanner (Brilliance 16, Philips Healthcare or Aquilion ONE, Canon Medical Systems). A
preliminary CT scan of the area of interest was taken to locate the puncture site, and the needle trajectory was planned to avoid the ribs and traverse the pleural surface/lung tissue
minimally. Local anesthetic (1% lidocaine) was injected subcutaneously at the needle puncture site. The needle was inserted and advanced close to the target lesion. Intermittent CT scans
were taken to examine the needle path during the procedure. After reaching the target lesion, specimens were obtained using a 20-gauge coaxial cutting needle system (Mission, Bard). For
histopathological examination, specimens were immediately immersed in a 10% formalin solution. POST-PROCEDURE IMAGING AND PATIENT CARE After the biopsy, the patients were observed in the
ward and positioned with the puncture side down. Immediate post-procedure CT images were obtained in selected cases according to the operator’s preference. In accordance with the protocol,
chest radiography was performed 4 h after the biopsy to rule out complications such as pneumothorax and hemorrhage. In cases showing pneumothorax development, conservative treatment was
administered with supplemental oxygen and monitoring of vital signs. In patients who showed signs of respiratory distress or a large amount of pneumothorax, a chest tube was inserted.
Patients who did not have complications or had minimal pneumothorax were discharged the following day. DATA COLLECTION One board-certified radiologist (3 years of experience in chest
radiology) collected data from the electronic medical record system and reviewed CT images. PATIENT AND LESION-RELATED INFORMATION Patient-related variables such as age, sex, smoking history
(never smoker, ex-smoker, or current smoker), and results of the pulmonary function test (forced vital capacity [FVC] and diffusing capacity of the lungs for carbon monoxide [DLCO]) were
recorded. The lesion-related information included the location (upper, middle, and/or lower lobe), size (long-axis diameter on axial CT images) and nodule density (solid or subsolid). In
addition, the presence of emphysema was evaluated. PROCEDURE-RELATED INFORMATION The procedure-related variables included the patient’s position, number of core biopsies, length of the
needle path (distance from the pleura to the target), penetration of honeycombing, needle tip within the target, and procedure time. PCNB-related complications were assessed and categorized
(minor vs. major) in accordance with the guidelines of the Society of Interventional Radiology24,25. Minor complications included pneumothorax, transient hemoptysis, and pulmonary alveolar
hemorrhage. Pneumothorax necessitating chest tube insertion, hemoptysis requiring embolization, air embolism, acute exacerbation of ILD, and death were classified as major complications.
PATHOLOGICAL RESULTS Original pathological reports were recorded. The PCNB results were categorized as malignant (including atypical adenomatous hyperplasia), benign (specific benign or
nonspecific benign), or non-evaluable due to insufficient specimens, while the reference standard results were blinded. Specific benign was defined as a specific benign tumor or infection
with an identified pathogen26. Nonspecific benign results were defined as the presence of benign features such as inflammatory cells or fibrosis that were insufficient to establish a
specific diagnosis27. Non-evaluable results were defined as cases in which the obtained specimens were insufficient or inadequate for establishing a pathologic diagnosis. To identify the
proportion of nondiagnostic results, we categorized the PCNB results as diagnostic results (malignancy and specific benign) and nondiagnostic results (nonspecific benign and non-evaluable)
according to the categorization described in previous studies28,29. REFERENCE STANDARDS The reference standard was established as follows15,30. First, if the lesion was surgically resected,
a surgical pathology report was used to establish the diagnosis. Second, if the biopsy result revealed malignant or specific benign lesions, it was based on pathologic analysis27. Third, the
lesion was considered benign if it remained stable for at least 2 years for solid nodules and 5 years for subsolid nodule according to the Fleischner Society guideline31 or decreased in
size with conservative treatment. Fourth, when the clinical behavior revealed an obvious malignant process such as metastasis or rapid tumor progression, the lesion was considered malignant.
STATISTICAL ANALYSIS The overall diagnostic accuracy, sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were evaluated. We calculated the
overall diagnostic accuracy, including the non-evaluable results. Based on the intention-to-diagnose principle, non-evaluable results were considered false negatives when calculating
sensitivity and false positives when calculating specificity32. The proportion of nondiagnostic results was calculated and the overall complication rate was then determined. The risk factors
for nondiagnostic results and pneumothorax were identified using Pearson χ2 or Fisher’s exact test for categorical variables and unpaired Student’s t-test for continuous variables. A p
value < 0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 25.0 software (IBM Corp.). CONSENT FOR PUBLICATION The content has not been
published nor submitted for publication elsewhere. RESULTS Of the 70 patients, 61 showed a UIP pattern with honeycombing and 9 showed a probable UIP pattern without honeycombing. Table 1
shows the patient demographics and lesion characteristics. There were 63 men (90.0%) and 7 women (10.0%), with a mean patient age of 73.5 years. Sixteen patients were nonsmokers, 34 were
current smokers, and 20 were ex-smokers. Of the 70 procedures, 53 (75.7%) showed malignant results, 11 (15.7%) showed benign results, and 6 (8.6%) showed non-evaluable results. The final
diagnosis was malignant lesions in 62 patients and benign lesions in 8 patients (Table 2). Malignant lesions were confirmed by biopsy or surgical resection (n = 55), biopsy of another organ
(n = 3), or post-procedural malignant process (n = 4). A final diagnosis of benign disease was confirmed based on microbiological confirmation (n = 4), decrease of lesion size with
conservative treatment (n = 3), and stable lesion size for at least 2 years (n = 1). The overall diagnostic accuracy, sensitivity, specificity, PPV, and NPV for the diagnosis of lung cancer
were 85.7% (60/70), 85.5% (53/62), 87.5% (7/8), 100.0% (53/53), and 63.6% (7/11), respectively. The proportion of nondiagnostic results was 18.6% (13/70). The nondiagnostic results consisted
of seven nonspecific benign results (three true-negative and four false-negative) and six non-evaluable results (Fig. 1). Table 3 shows the identified risk factors for nondiagnostic
results. Two or less core biopsy sampling was related to nondiagnostic results (_p_ = 0.002). FVC, DLCO, and penetration of honeycombing were not related to the nondiagnostic results.
Furthermore, the presence of the needle tip within the target was not related to the nondiagnostic results in this study (_p_ = 0.416) (Table 3). The overall complication rate was 35.7%
(25/70). The minor complication rate was 31.4% (22/70), and the major complication rate was 4.3% (3/70). Pneumothorax developed in 22 patients (31.4%), and subsequent chest tube insertion
was needed in three patients (4.3%). Pulmonary alveolar hemorrhage without symptoms developed in three patients (4.3%), and mild hemoptysis developed in two patients (2.9%). Neither
condition required any intervention. Two patients showed bilateral pneumothorax and pulmonary alveolar hemorrhage. All cases of major complications involved pneumothorax requiring chest tube
drainage. No major complications, including PCNB-related air embolism, acute exacerbation of ILD, and death occurred. Table 4 shows the identified risk factors for pneumothorax. The needle
path was significantly longer in patients with pneumothorax (_p_ = 0.007) (Fig. 2, Table 4). Similarly, non-subpleural lesions showed a higher incidence of pneumothorax than subpleural
lesions (_p_ = 0.002) (Table 4). FVC, DLCO, and penetration of honeycombing were not related to the incidence of pneumothorax (_p_ = 0.713, 1.000, and 0.760, respectively) (Fig. 3).
DISCUSSION We assessed the diagnostic performance and complication rate of CT-guided PCNB by using a coaxial needle in patients with a UIP pattern of ILD and evaluated the risk factors for
nondiagnostic results and pneumothorax. Although PCNB has been established as a safe diagnostic procedure, only one study has evaluated the diagnostic accuracy of percutaneous lung biopsy in
patients with UIP17. That study used both fine-needle aspiration and core biopsy results and included only a few cases using a coaxial needle. To our knowledge, this is the first study to
analyze the diagnostic accuracy and safety of CT-guided PCNB with a coaxial needle in patients with UIP. We found that the overall diagnostic accuracy, sensitivity, and specificity of
CT-guided PCNB with a coaxial needle in patients with UIP were 85.7%, 85.5%, and 87.5%, respectively. These results are slightly lower than those reported in previous studies11,30,33,34.
However, those studies excluded non-evaluable results for calculating diagnostic accuracy, sensitivity, and specificity. As we considered non-evaluable results as false-negative or
false-positive while calculating diagnostic accuracy, sensitivity, and specificity, the diagnostic value was lower than that reported in the aforementioned studies. Furthermore, the
reduction in diagnostic accuracy was relatively large due to the small number of cases. Shin et al. reported that CT-guided lung biopsy had an 89% diagnostic accuracy in patients with a
UIP/IPF pattern17; our result is slightly lower, but comparable. They reported that the presence of the needle tip outside the target and a small lesion size were risk factors for
nondiagnostic results. In contrast to their findings, these factors were not significantly related to the nondiagnostic results in our study. Our study revealed that the availability of
three or more core biopsy samples significantly increased the diagnostic results. This may be due to the reduced sampling error. These findings are consistent with those of previous studies
using a coaxial needle system, which documented that the availability of three or more specimens was associated with a higher diagnostic accuracy15,35. Pulmonary function (FVC and DLCO) was
not related to nondiagnostic results. The overall complication rate and major complication rate were 35.7% (25/70) and 4.3% (3/70), respectively. These rates were much lower than those
reported in a previous study that reported an overall complication rate of 51% and a major complication rate of 38% in patients with a UIP/IPF pattern17. However, the two studies had many
differences in patient group and procedure technique, so an exact comparison of both studies is difficult. However, we conjectured that one of the possible causes of the difference in
complication rates is the use of coaxial needles. The coaxial technique allows for much easier sampling repetition without increasing the number of pleural passages19,20. In theory, the
complication rate is thought to be low because of the smaller pleural injury as a result of avoiding repeated pleural punctures. However, a comparative study between the coaxial needle group
and the non-coaxial needle group in patients with a UIP pattern of ILD is needed for verification. Pneumothorax is the most common complication of CT-guided PCNB, and the reported incidence
after lung biopsy ranges between 17 and 60%10,36,37,38. In our study, pneumothorax occurred in 22 of 70 patients (31.4%). This rate was within the range of values reported in previous
studies. In our study, a higher rate of pneumothorax was associated with a deeper location of the lesion from the pleural surface. Several studies reported comparable results to
ours12,37,39,40,41. It would be reasonable to assume that the longer the needle remains in the lung parenchyma, the greater the risk of tearing the pleura as the patient breathes during the
procedure37,42. Furthermore, needle redirection may be more frequently required with a longer needle path, which could result in pleural injury39. In contrast, Yeow et al.43 reported that
subpleural location was a risk factor for pneumothorax because insufficient anchoring caused the needle to dislodge into the pleural space easily, resulting in air ingress. However, in our
study, non-subpleural lesions presented with a higher incidence of pneumothorax than subpleural lesions. Pneumothorax itself is an occasional complication of UIP16,44. Therefore, we
predicted that patients with UIP would show a higher incidence of pneumothorax after PCNB. However, the incidence was within a reasonable range in comparison with previous studies that were
not limited to patients with UIP10,36,37,38. Shin et al. reported that penetration of honeycomb cysts was a risk factor for major complications after lung biopsy in patients with a UIP/IPF
pattern17. However, the penetration of honeycomb cysts was not associated with pneumothorax or complications in our study. This study had several limitations. First, this study was a
retrospective study that included a small sample. The retrospective design of this study might have resulted in selection bias. In addition, owing to the small sample size, some risk factors
for nondiagnostic results and pneumothorax might have failed to exhibit statistical significance. Second, the differences in diagnostic accuracy and complication rates between the groups
with and without UIP were not compared. Third, we included patients with a UIP pattern ILD based on CT findings using updated guidelines22,23. The UIP pattern is observed not only in IPF but
also in collagen vascular disease associated ILD, hypersensitivity pneumonitis, and asbestosis. Since it includes heterogeneous disease entities, the clinical characteristics of each
disease cannot be reflected. Fourth, at the time of biopsy, the majority of patients in our study had relatively good pulmonary function. It is possible that only patients who were
considered clinically capable of PCNB were included, implying that our study cohort might not be representative of all patients with UIP. Finally, the number of occasions in which the
pleural surface was repeatedly penetrated was not recorded in detail, although it was very low. In conclusion, CT-guided PCNB with a coaxial cutting needle is a useful diagnostic technique
for the diagnosis of lung cancer, even in patients with UIP. It yields reasonable diagnostic accuracy and an acceptable complication rate. DATA AVAILABILITY The datasets generated during
and/or analyzed during the current study are available from the corresponding author on reasonable request. REFERENCES * Lynch, D. A. _et al._ Idiopathic interstitial pneumonias: CT
features. _Radiology_ 236, 10–21. https://doi.org/10.1148/radiol.2361031674 (2005). Article PubMed Google Scholar * Adegunsoye, A. _et al._ Computed tomography honeycombing identifies a
progressive fibrotic phenotype with increased mortality across diverse interstitial lung diseases. _Ann. Am. Thorac. Soc._ 16, 580–588. https://doi.org/10.1513/AnnalsATS.201807-443OC (2019).
Article PubMed PubMed Central Google Scholar * Salisbury, M. L. _et al._ Hypersensitivity pneumonitis: Radiologic phenotypes are associated with distinct survival time and pulmonary
function trajectory. _Chest_ 155, 699–711. https://doi.org/10.1016/j.chest.2018.08.1076 (2019). Article PubMed Google Scholar * Zamora-Legoff, J. A., Krause, M. L., Crowson, C. S., Ryu,
J. H. & Matteson, E. L. Progressive decline of lung function in rheumatoid arthritis-associated interstitial lung disease. _Arthrit. Rheumatol._ 69, 542–549.
https://doi.org/10.1002/art.39971 (2017). Article CAS Google Scholar * Walsh, S. L. _et al._ Connective tissue disease related fibrotic lung disease: high resolution computed tomographic
and pulmonary function indices as prognostic determinants. _Thorax_ 69, 216–222. https://doi.org/10.1136/thoraxjnl-2013-203843 (2014). Article PubMed Google Scholar * Le Jeune, I. _et
al._ The incidence of cancer in patients with idiopathic pulmonary fibrosis and sarcoidosis in the UK. _Respir. Med._ 101, 2534–2540. https://doi.org/10.1016/j.rmed.2007.07.012 (2007).
Article PubMed Google Scholar * Naccache, J. M. _et al._ Lung cancer and interstitial lung disease: A literature review. _J. Thorac. Dis._ 10, 3829–3844.
https://doi.org/10.21037/jtd.2018.05.75 (2018). Article PubMed PubMed Central Google Scholar * Xiaohong, X. _et al._ Management and prognosis of interstitial lung disease with lung
cancer (ILD-LC): A real-world cohort from three medical centers in China. _Front. Mol. Biosci._ 8, 660800. https://doi.org/10.3389/fmolb.2021.660800 (2021). Article PubMed PubMed Central
Google Scholar * Lee, K. H. _et al._ Diagnostic accuracy of percutaneous transthoracic needle lung biopsies: a multicenter study. _Korean J. Radiol._ 20, 1300–1310.
https://doi.org/10.3348/kjr.2019.0189 (2019). Article PubMed PubMed Central Google Scholar * Yoon, S. H. _et al._ Analysis of complications of percutaneous transthoracic needle biopsy
using CT-Guidance modalities in a multicenter cohort of 10568 biopsies. _Korean J. Radiol._ 20, 323–331. https://doi.org/10.3348/kjr.2018.0064 (2019). Article PubMed Google Scholar * Kim,
T. J. _et al._ Diagnostic accuracy of CT-guided core biopsy of ground-glass opacity pulmonary lesions. _AJR Am. J. Roentgenol._ 190, 234–239. https://doi.org/10.2214/AJR.07.2441 (2008).
Article PubMed Google Scholar * Laurent, F., Michel, P., Latrabe, V., Tunon de Lara, M. & Marthan, R. Pneumothoraces and chest tube placement after CT-guided transthoracic lung biopsy
using a coaxial technique: Incidence and risk factors. _AJR Am. J. Roentgenol._ 172, 1049–1053https://doi.org/10.2214/ajr.172.4.10587145 * Laurent, F., Montaudon, M., Latrabe, V. &
Begueret, H. Percutaneous biopsy in lung cancer. _Eur. J. Radiol._ 45, 60–68. https://doi.org/10.1016/s0720-048x(02)00286-3 (2003). Article PubMed Google Scholar * Manhire, A. _et al._
Guidelines for radiologically guided lung biopsy. _Thorax_ 58, 920–936. https://doi.org/10.1136/thorax.58.11.920 (2003). Article CAS PubMed PubMed Central Google Scholar * Hiraki, T.
_et al._ CT fluoroscopy-guided biopsy of 1,000 pulmonary lesions performed with 20-gauge coaxial cutting needles: Diagnostic yield and risk factors for diagnostic failure. _Chest_ 136,
1612–1617. https://doi.org/10.1378/chest.09-0370 (2009). Article PubMed Google Scholar * Yamazaki, R. _et al._ Pneumothorax in patients with idiopathic pulmonary fibrosis: A real-world
experience. _BMC Pulm. Med._ 21, 5. https://doi.org/10.1186/s12890-020-01370-w (2021). Article PubMed PubMed Central Google Scholar * Shin, Y. J. _et al._ Accuracy and complications of
percutaneous transthoracic needle lung biopsy for the diagnosis of malignancy in patients with idiopathic pulmonary fibrosis. _Eur. Radiol._ 31, 9000–9011.
https://doi.org/10.1007/s00330-021-08038-x (2021). Article PubMed Google Scholar * Laurent, F., Latrabe, V., Vergier, B. & Michel, P. Percutaneous CT-guided biopsy of the lung:
Comparison between aspiration and automated cutting needles using a coaxial technique. _Cardiovasc. Interv. Radiol._ 23, 266–272. https://doi.org/10.1007/s002700010067 (2000). Article CAS
Google Scholar * Zhang, L. _et al._ Coaxial technique-promoted diagnostic accuracy of CT-guided percutaneous cutting needle biopsy for small and deep lung lesions. _PLoS ONE_ 13, e0192920.
https://doi.org/10.1371/journal.pone.0192920 (2018). Article CAS PubMed PubMed Central Google Scholar * Nour-Eldin, N. E. _et al._ Pneumothorax Complicating Coaxial and Non-coaxial
CT-Guided Lung Biopsy: Comparative analysis of determining risk factors and management of pneumothorax in a retrospective review of 650 patients. _Cardiovasc. Interv. Radiol._ 39, 261–270.
https://doi.org/10.1007/s00270-015-1167-3 (2016). Article Google Scholar * Yoon, S. H. _et al._ 2020 Clinical Practice Guideline for Percutaneous Transthoracic Needle Biopsy of Pulmonary
Lesions: A consensus statement and recommendations of the korean society of thoracic radiology. _Korean J. Radiol._ 22, 263–280. https://doi.org/10.3348/kjr.2020.0137 (2021). Article PubMed
Google Scholar * Raghu, G. _et al._ Diagnosis of Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT clinical practice guideline. _Am. J. Respir. Crit. Care Med._ 198, e44–e68.
https://doi.org/10.1164/rccm.201807-1255ST (2018). Article PubMed Google Scholar * Lynch, D. A. _et al._ Diagnostic criteria for idiopathic pulmonary fibrosis: A Fleischner Society White
Paper. _Lancet Respir. Med._ 6, 138–153. https://doi.org/10.1016/S2213-2600(17)30433-2 (2018). Article PubMed Google Scholar * Veltri, A., Bargellini, I., Giorgi, L., Almeida, P. &
Akhan, O. CIRSE guidelines on percutaneous needle biopsy (PNB). _Cardiovasc. Interv. Radiol._ 40, 1501–1513. https://doi.org/10.1007/s00270-017-1658-5 (2017). Article Google Scholar *
Sacks, D., McClenny, T. E., Cardella, J. F. & Lewis, C. A. Society of interventional radiology clinical practice guidelines. _J. Vasc. Interv. Radiol._ 14, S199-202.
https://doi.org/10.1097/01.rvi.0000094584.83406.3e (2003). Article PubMed Google Scholar * Gelbman, B. D. _et al._ Radiographic and clinical characterization of false negative results
from CT-guided needle biopsies of lung nodules. _J. Thorac. Oncol._ 7, 815–820. https://doi.org/10.1097/JTO.0b013e31824abd9c (2012). Article PubMed Google Scholar * Kim, J. I., Park, C.
M., Kim, H., Lee, J. H. & Goo, J. M. Non-specific benign pathological results on transthoracic core-needle biopsy: how to differentiate false-negatives?. _Eur. Radiol._ 27, 3888–3895.
https://doi.org/10.1007/s00330-017-4766-3 (2017). Article PubMed Google Scholar * Haas, B. M. _et al._ Nondiagnostic computed tomography-guided percutaneous lung biopsies are more likely
when infection is suspected. _J. Thorac. Imag._ 31, 151–155. https://doi.org/10.1097/RTI.0000000000000207 (2016). Article Google Scholar * Lee, K. H. _et al._ Nondiagnostic percutaneous
transthoracic needle biopsy of lung lesions: A multicenter study of malignancy risk. _Radiology_ 290, 814–823. https://doi.org/10.1148/radiol.2018181482 (2019). Article PubMed Google
Scholar * Lee, S. M. _et al._ C-arm cone-beam CT-guided percutaneous transthoracic needle biopsy of lung nodules: Clinical experience in 1108 patients. _Radiology_ 271, 291–300.
https://doi.org/10.1148/radiol.13131265 (2014). Article PubMed Google Scholar * MacMahon, H. _et al._ Guidelines for management of incidental pulmonary nodules detected on CT images: From
the Fleischner Society 2017. _Radiology_ 284, 228–243. https://doi.org/10.1148/radiol.2017161659 (2017). Article PubMed Google Scholar * Schuetz, G. M., Schlattmann, P. & Dewey, M.
Use of 3x2 tables with an intention to diagnose approach to assess clinical performance of diagnostic tests: Meta-analytical evaluation of coronary CT angiography studies. _BMJ_ 345, e6717.
https://doi.org/10.1136/bmj.e6717 (2012). Article PubMed PubMed Central Google Scholar * Choi, S. H. _et al._ Percutaneous CT-guided aspiration and core biopsy of pulmonary nodules
smaller than 1 cm: Analysis of outcomes of 305 procedures from a tertiary referral center. _AJR Am. J. Roentgenol._ 201, 964–970. https://doi.org/10.2214/AJR.12.10156 (2013). Article PubMed
Google Scholar * Hur, J. _et al._ Diagnostic accuracy of CT fluoroscopy-guided needle aspiration biopsy of ground-glass opacity pulmonary lesions. _AJR Am. J. Roentgenol._ 192, 629–634.
https://doi.org/10.2214/AJR.08.1366 (2009). Article PubMed Google Scholar * Lim, C., Lee, K. Y., Kim, Y. K., Ko, J. M. & Han, D. H. CT-guided core biopsy of malignant lung lesions:
How many needle passes are needed?. _J. Med. Imag. Radiat. Oncol._ 57, 652–656. https://doi.org/10.1111/1754-9485.12054 (2013). Article Google Scholar * Otto, S. _et al._ Predictors of
technical success and rate of complications of image-guided percutaneous transthoracic lung needle biopsy of pulmonary tumors. _PLoS ONE_ 10, e0124947.
https://doi.org/10.1371/journal.pone.0124947 (2015). Article CAS PubMed PubMed Central Google Scholar * Khan, M. F. _et al._ Variables affecting the risk of pneumothorax and
intrapulmonal hemorrhage in CT-guided transthoracic biopsy. _Eur. Radiol._ 18, 1356–1363. https://doi.org/10.1007/s00330-008-0893-1 (2008). Article CAS PubMed Google Scholar * Maxwell,
A. W. _et al._ CT-guided transthoracic needle aspiration biopsy of subsolid lung lesions. _J. Vasc. Interv. Radiol._ 25, 340–346. https://doi.org/10.1016/j.jvir.2013.11.037 (2014). Article
PubMed Google Scholar * Cox, J. E., Chiles, C., McManus, C. M., Aquino, S. L. & Choplin, R. H. Transthoracic needle aspiration biopsy: Variables that affect risk of pneumothorax.
_Radiology_ 212, 165–168. https://doi.org/10.1148/radiology.212.1.r99jl33165 (1999). Article CAS PubMed Google Scholar * Topal, U. & Ediz, B. Transthoracic needle biopsy: Factors
effecting risk of pneumothorax. _Eur. J. Radiol._ 48, 263–267. https://doi.org/10.1016/s0720-048x(03)00058-5 (2003). Article PubMed Google Scholar * Chami, H. A. _et al._ Predictors of
pneumothorax after CT-guided transthoracic needle lung biopsy: The role of quantitative CT. _Clin. Radiol._ 70, 1382–1387. https://doi.org/10.1016/j.crad.2015.08.003 (2015). Article CAS
PubMed Google Scholar * Kinoshita, F. _et al._ CT-guided transthoracic needle biopsy using a puncture site-down positioning technique. _AJR Am. J. Roentgenol._ 187, 926–932.
https://doi.org/10.2214/AJR.05.0226 (2006). Article PubMed Google Scholar * Yeow, K. M. _et al._ Risk factors for pneumothorax and bleeding after CT-guided percutaneous coaxial cutting
needle biopsy of lung lesions. _J. Vasc. Interv. Radiol._ 12, 1305–1312. https://doi.org/10.1016/s1051-0443(07)61556-5 (2001). Article CAS PubMed Google Scholar * Franquet, T., Gimenez,
A., Torrubia, S., Sabate, J. M. & Rodriguez-Arias, J. M. Spontaneous pneumothorax and pneumomediastinum in IPF. _Eur. Radiol._ 10, 108–113. https://doi.org/10.1007/s003300050014 (2000).
Article CAS PubMed Google Scholar Download references AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Radiology, Ajou University School of Medicine, 164 Worldcup Road,
Yeongtong-gu, Suwon, 16499, Republic of Korea Da Young Kim, Joo Sung Sun, Kyung Joo Park & Seulgi You * Department of Radiology, Hankook Hospital, Cheongju, Republic of Korea Eun Young
Kim Authors * Da Young Kim View author publications You can also search for this author inPubMed Google Scholar * Joo Sung Sun View author publications You can also search for this author
inPubMed Google Scholar * Eun Young Kim View author publications You can also search for this author inPubMed Google Scholar * Kyung Joo Park View author publications You can also search for
this author inPubMed Google Scholar * Seulgi You View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS S.Y. and J.S.S. conceived the original
idea and aims of the project. K.J.P. supervised the project. S.Y., J.S.S. and E.Y.K. participated as operators. D.Y.K. and S.Y. collected and analyzed the patient data and wrote manuscript.
All authors reviewed and approved the manuscript. CORRESPONDING AUTHOR Correspondence to Seulgi You. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests.
ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS
OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or
format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or
other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not
included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission
directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Kim,
D.Y., Sun, J.S., Kim, E.Y. _et al._ Diagnostic accuracy and safety of CT-guided percutaneous lung biopsy with a coaxial cutting needle for the diagnosis of lung cancer in patients with UIP
pattern. _Sci Rep_ 12, 15682 (2022). https://doi.org/10.1038/s41598-022-20030-z Download citation * Received: 07 February 2022 * Accepted: 07 September 2022 * Published: 20 September 2022 *
DOI: https://doi.org/10.1038/s41598-022-20030-z SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is
not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative