Play all audios:
ABSTRACT Fluoroscopy-guided injection via the anterior (A), anterolateral (AL), or proximal anterolateral (PAL) approaches are the common hip injection techniques without comparing the
efficacy of the three techniques. The prospective randomized controlled trial was conducted from August 2020 to March 2022. Included patients with intra-articular hip disorders indicated an
intra-articular steroid injection. Excluded significant spine pathology with radiculopathy or significant neurological deficits, previous hip surgery of the injection side, suspected tumor
or infection origins, steroid or contrast media allergy, and body mass index > 35 kg/m2. The primary outcome was the injection attempt defining one attempt and multiple attempts. 90
patients were recruited and allocated to 30 per group. There were no differences between A, AL, and PAL respectively regarding the success in one attempt rate (80%, 80%, 90%; p = 0.533), VAS
during local anesthetic injection (4.33 ± 1.99, 3.70 ± 2.34, 4.27 ± 2.49; p = 0.500), VAS during intra-articular injection (4.27 ± 1.87, 4.70 ± 2.37, 4.13 ± 2.37; p = 0.587), radiation
doses (0.558 ± 0.313, 0.526 ± 0.485, 0.492 ± 0.275 mGy; p = 0.788), radiation time (0.043 ± 0.017, 0.039 ± 0.021, 0.041 ± 0.015 seconds; p = 0.723), and complications. The post-injection
mHHS was improved in all three approaches without significant differences. SIMILAR CONTENT BEING VIEWED BY OTHERS LUMBAR ZYGAPOPHYSEAL JOINTS INJECTIONS UNDER ULTRASOUND GUIDANCE AN
ALTERNATIVE TO FLUOROSCOPY GUIDANCE IN THE MANAGEMENT OF LOW BACK PAIN Article Open access 07 March 2022 CLINICAL EFFICACY OF DIRECT ANTERIOR APPROACH VERSUS POSTERIOR LATERAL APPROACH FOR
TOTAL HIP REPLACEMENT IN MIDDLE-AGED AND ELDERLY PATIENTS OF FEMORAL NECK FRACTURE Article Open access 12 February 2025 COMPARISON OF ULTRASONOGRAPHIC, RADIOGRAPHIC AND INTRA-OPERATIVE
FINDINGS IN SEVERE HIP OSTEOARTHRITIS Article Open access 03 December 2020 INTRODUCTION The use of intra-articular steroid injection of the hip helps differentiate between intra-articular
hip pathologies and extra-articular hip pathologies as the causes of hip pain and for the therapeutic management of hip osteoarthritis or synovitis1,2,3,4,5,6,7. Intra-articular steroid
injection has a sensitivity of 91.5% and specificity of up to 100% to identify intra-articular pathology if the patient experienced improvement of symptoms after the procedures2. Currently,
the intra-articular hip injection has been widely used, with the three common approaches being the anterior approach (A)8, the anterolateral approach (AL)9, and the proximal anterolateral
approach (PAL)10. Despite the large quantities of research surrounding the use of intra-articular steroid injection of the hip, the majority of researchers emphasized the improvement of
symptoms, and in comparing the assistive method such as comparing ultrasound-assisted intra-articular hip injection with fluoroscopic assisted intra-articular hip injection. None of the
studies focus on comparing the accuracy and efficacy of three common fluoroscopic guidance intra-articular hip injection approaches. This study aimed to compare the efficacy of anterior,
anterolateral, and proximal anterolateral approaches of the fluoroscopy-guided intra-articular hip injection. We hypothesized that there would be a significant difference in efficacy between
the three intra-articular steroid injection approaches and that this study would be able to guide the physician in choosing the best approach for their patients. METHODS The patient
recruitment was performed at Thammasat University Hospital in January 2020 after approval by the ethics committee. All procedures performed in studies involving human participants were
approved by the ethics committee of Thammasat University (Registration no. MTU-EC-OT-1-184/62) on 20/01/2020. The study protocol was registered and submitted to the Thai Clinical Trials
Registry (TCTR) with the TCTR identification number TCTR20200722002. The date of the first registration was 22/07/2020. All methods were performed in accordance with the relevant guidelines
and regulations. A prospective randomized controlled trial of hip intra-articular injection was started from 01/08/2020 to 31/03/2022 after the protocol had been registered and approved in
the clinical trial registry. The inclusion criteria included patients with intra-articular hip disorders from osteoarthritis, femoroacetabular impingement (FAI), synovitis, and labral
lesions who indicated an intra-articular steroid injection. The exclusion criteria included significant degenerative spine pathology with radiculopathy or significant neurological deficits,
previous hip surgery of the injection side, presence of an osteolytic or osteoblastic lesion on imaging suspected tumor or infection origins, active infection around the hip, allergic to
steroid or contrast media, and body mass index (BMI) more than 35 kg/m2. The term “efficacy” in this study was primarily defined as the success of “one attempt of fluoroscopy-guided
injection”. The secondary outcomes of efficacy included pain during injection, radiation doses and time, complications, and short-term functional score improvement using the modified Harris
hip score (mHHS)11. From the pilot study, the resulting efficacy defined by “single attempt of injection” for the anterior, anterolateral, and proximal anterolateral approaches in 30
patients were 70%, 70%, and 90% respectively. Based on a non-inferiority trail with a 10% non-inferiority limit, the significance level (alpha) was 0.05, and the power was 90%. The output of
the sample size calculation from n4Studies was 29 samples per group, with a total of 87 patients. After patient screening and recruitment by eligible criteria, all patients were advised of
the procedures, risks, and benefits of the research, thereafter the patients were informed and signed the consent form. The pre-injection mHHS was evaluated on recruitment day. On the
injection day, patients stayed in a supine position and put the pillow underneath the patient’s knees to provide about 20 degrees of hip flexion. The injection site was prepared in a
standard sterile fashion. The approach of injection was random using computerized randomization with the block of 6 and allocated with a sealed opaqued envelope before injection. The
injection was performed by a single fellowship-trained surgeon in hip arthroscopy under fluoroscopic guidance to enhance visual clarity, in the operation room without the pre-medication. The
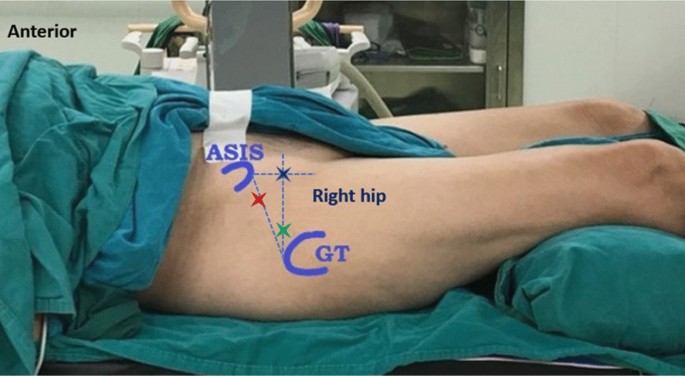
surface landmark of each injection approach on the right hip is shown in Fig. 1. The first line was drawn from ASIS down to the center of the patella (line 1), the second line was drawn
from the superior edge of the greater trochanter (GT) to intersect with line 1 perpendicularly (line 2), and the third line was drawn from the anterosuperior iliac spine (ASIS) directed
inferolateral to the tip of GT (line 3). The entry point for the anterior approach (A) is the intersection between lines 1 and 2 (blue X mark). The entry point for the anterolateral approach
(AL) is about 1 centimeter superior and anterior to the tip of GT (green X mark). The entry point for the proximal anterolateral approach (PAL) is about 1/3 upper portion of line 3 (red X
mark). The intra-articular injection was performed using needle No.25, and a local anesthetic solution of 1% xylocaine without adrenaline 3 mL was injected. The Visual analog scale (VAS)
during local anesthetic injection was evaluated. Then, using spinal needle No. 20 (Length of 90 mm) to inject the hip joint following protocol for each approach, the mixture of
“Triamcinolone acetonide (40 mg) 1 mL plus an OmniplaqueTM (350mg/mL) 1 mL plus the 1% Xylocaine without adrenaline 8 mL” were injected into the hip joint. Fluoroscopic imaging (PHILIPS BV
Pulsera) was used in the anteroposterior (AP) view to identify whether the approach was successful. “Success” is defined by the contrast media filled inside the hip capsule. “Single attempt”
was defined as the single shot in injection without redirection of the spinal needle (redirection was defined by changing the direction by pulling back the needle more than half of the
needle length). “More than one attempt or multiple attempts” was defined as the need for redirection by pulling a spinal needle out for more than 40 mm (half of the needle length). VAS
during intra-articular hip injection was recorded. Radiation exposure was recorded as doses and radiation time. Complication such as infection or vasovagal symptoms was recorded (if
occurred). The patients were made appointments for subsequence follow-ups at 2 weeks intervals and were evaluated for post-injection mHHS. STATISTICAL ANALYSIS Descriptive data were reported
as frequencies (percentage, %) or mean ± standard deviation (SD). The Fisher exact test was used to compare categorical data between groups e.g. gender, and affected side. The Oneway-ANOVA
test was used for comparisons of continuous variables with normal distribution, and the Kruskal-Wallis’s test was used for continuous variables with non-normal distribution including age,
BMI, VAS during local anesthetic injection, VAS during intra-articular injection, radiation exposure, pre-injection mHHS, post-injection mHHS. P < 0.05 was statistically significant. Data
were analyzed using Stata version 14.2 (StataCorp, Lakeway, Texas, USA). RESULTS A total of 90 patients were included with 30 patients in each group. The CONSORT flow diagram is presented
in Fig. 2. Patient characteristics are shown in Table 1. The majority of the study population was female (71%) with a mean age of 54.8 years old. Osteoarthritis of the hip was the most
common pathology in about 82%. There was no significant difference between the patient demographics who received each injection approach. The success in “single attempt” was 80%, 80%, and
90% in A, AL, and PAL approaches respectively. There was no statistically significant difference in single-attempt success between the three injection techniques (p = 0.533). The accuracy
rate of intra-articular injection in the study was 100% in all approaches either single or multiple attempts by the fluoroscopic guidance and controlled injection, confirmed by observing the
contrast media filled within the hip joint capsule in all cases. There were no statistically significant differences in the VAS during local anesthetic injection (p = 0.5), VAS during
intra-articular injection (p = 0.587), radiation doses (p = 0.788), and radiation time (p = 0.723). The results are shown in Table 2. The overall complication was 1 patient of 90 (1%) in the
PAL injection approach, the patient developed vasovagal symptoms after a single attempt of injection which spontaneously resolved after a rest of about 2–3 minutes without the need for
further management. There was no patient with injury of the lateral femoral cutaneous nerve of the thigh or infection after injection. For the post-injection mHHS collected 2 weeks after
injection, there was an improvement from pre-injection in all approaches. DISCUSSION From this study, using the three approaches, namely anterior, anterolateral, and proximal anterolateral
approaches for fluoroscopy-guided intra-articular hip injection, the overall successful intra-articular hip injection in a single attempt is 83%, with the anterior approach in 80%,
anterolateral approach in 80%, and proximal anterolateral approach in 90%, we did not find the statistically significant differences between three approaches. The VAS during local anesthetic
injection, VAS during intra-articular injection, radiation doses, radiation time of exposure, and the post-injection mHHS were similar in all three approaches without significant
differences between groups. The accuracy rate in our study is 100% (including 83% single attempt, and 17% multiple attempts) intra-articular injection in all approaches during the use of
fluoroscopic guidance and controlled injection. After the tip of the needle reached the femoral head-neck area, we found the contrast within the hip joint capsule in all patients, we could
not observe any extra-articular leakage of the radio-opaque media. Compared to the previous study on the accuracy of each approach which reported a 938–96.7%9 accuracy for the anterior
approach, 94–95% accuracy for the proximal anterolateral approach10,12, and 100% accuracy for the anterolateral approach9. Our study had a high accuracy rate, we hypothesized that this might
result from the difference in the experience of performers and the injection techniques in each study. Furthermore, in our injection technique, the hip was about 20 degrees flexion, we
would check the direction of the needle using the fluoroscopic control until reached the desired direction to the anterior or anterolateral site of the femoral head-neck junction and the tip
of the needle always need to touch the bone before we injected. We injected the steroid and the mixtures by slightly pushing and pulling the needle backward-forward around the point of
injection area and controlling with the sequential fluoroscopy. With this technique, we’ve achieved a standardized procedure with reliable results for hip injection. For the secondary
outcome, we report no statistically significant difference in pain using a visual analog scale (VAS), both during local anesthetic injection and intra-articular hip injection between the
three approaches, with the mean VAS of about 4 on both procedures. Even though the data focusing on pain during the procedure have not yet been previously reported, from the result of our
study which showed a similar level of pain in all approaches, we can conclude that pain should not be a factor when considering the intra-articular hip injection approaches. Additionally,
we’ve found no statistically significant difference in radiation exposure between the approaches. The average radiation doses (anterior of 0.56 ± 0.31, anterolateral of 0.53 ± 0.49, and
proximal anterolateral of 0.49 ± 0.28 mGy) were less than another study9 showed anterior and lateral median radiation doses of 1 mGy and 3 mGy, respectively. The radiation doses in our study
are within the standard exposure for radiographs of the pelvis (1.31 mGy)13. Throughout our study, we’ve only experienced one complication from ninety patients, which accounts for 1.1%.
Details on the event were as follows, the patient was 29 years 29-year-old man diagnosed with secondary osteoarthritis of the right hip after trauma, he was allocated to the PAL injection
group, and during the procedure, he experienced lightheadedness with normal vital signs and oxygen saturation. The symptoms recovered spontaneously after resting for 2 minutes, thus the
symptom was considered to be caused by vasovagal symptoms. Following 2 weeks, the patient returned for follow-up with an improvement in mHHS from 58.3 pre-injection to 82.5 post-injection,
no further complication was recorded. There were no serious complications14,15 related to the injection. Comparing the pre-injection mHHS with post-injection mHHS, there was no statistically
significant difference between the three groups. However, comparing the pre-injection score with post-injection mHHS in the same group, we reported a significant improvement in
post-injection mHHS in all three groups. The results represent the improvement in very short-term outcomes of successful intra-articular steroid injection of the hip despite the approach
being used. We did not evaluate the outcomes of longer follow-up because of the natural history of the intra-articular steroid injection that mainly affected only about 6–12 weeks after
injection1,16,17,18 and we aimed to evaluate the short-term efficacy between the three different hip injection approaches. Hip injection using anatomic landmarks without ultrasonographic or
radiographic assistance is useful and provides acceptable accuracy12,19,20. This study used the fluoroscopy-guided hip injection, which is common and standard for the diagnostic and
therapeutic management of hip disorder patients1,7,21,22. Our study is the first study to compare the efficacy between three commonly used techniques for intra-articular hip injection. No
study compared the safety and outcomes of each injection approach. Additionally, all operating procedures were performed by a single fellowship-trained surgeon in hip arthroscopy, and the
operative setting was standardized in every patient therefore the errors and variations in the injection techniques were minimized in our study. Our study is not without limitations,
however. Due to the single well-trained performer in our study, our result may not be generalizable to a general orthopedic surgeon or general practitioners, however in providing detailed
instruction on the operative setting and procedure we used in this study, we believed that similar result could be achieved even with less experienced practitioners. Furthermore, our study
has a small sample size, which might not represent the general population, and has low power to detect the statistical significance. The very short-term outcomes were evaluated that could
not evaluate the effect of each approach in terms of medium- to long-term therapeutic outcomes. Finally, the non-blind nature of our study design could cause bias in the outcome measure.
CONCLUSION Fluoroscopy-guided hip injection via the anterior (A), anterolateral (AL), or proximal anterolateral (PAL) approaches were comparable in efficacy regarding the number of attempts,
VAS during injection, radiation exposure, post-injection mHHS, and complications. The physicians can choose any of their preferred fluoroscopy-guided hip injection approaches. DATA
AVAILABILITY The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request. REFERENCES * Choueiri, M., Chevalier, X. &
Eymard, F. Intraarticular corticosteroids for hip osteoarthritis: A review. _Cartilage_ 13, 122s–131s. https://doi.org/10.1177/1947603520951634 (2021). Article PubMed Google Scholar *
Deshmukh, A. J. _et al._ Accuracy of diagnostic injection in differentiating source of atypical hip pain. _J. Arthroplasty_ 25, 129–133. https://doi.org/10.1016/j.arth.2010.04.015 (2010).
Article PubMed Google Scholar * Kivlan, B. R., Martin, R. L. & Sekiya, J. K. Response to diagnostic injection in patients with femoroacetabular impingement, labral tears, chondral
lesions, and extra-articular pathology. _Arthroscopy_ 27, 619–627. https://doi.org/10.1016/j.arthro.2010.12.009 (2011). Article PubMed Google Scholar * Mujahed, T. _et al._ Preoperative
intra-articular steroid injections as predictors of hip arthroscopy: 2-year outcomes. _Orthop. J. Sports Med._ 9, 23259671211053816. https://doi.org/10.1177/23259671211053817 (2021). Article
PubMed PubMed Central Google Scholar * Ward, D. & Parvizi, J. Management of hip pain in young adults. _Orthop. Clin. N. Am._ 47, 485–496. https://doi.org/10.1016/j.ocl.2016.03.002
(2016). Article Google Scholar * Kanthawang, T. _et al._ Predicting outcomes in patients undergoing intra-articular corticosteroid hip injections. _Skelet. Radiol._ 50, 1347–1357.
https://doi.org/10.1007/s00256-020-03673-9 (2021). Article Google Scholar * Lambert, R. G. _et al._ Steroid injection for osteoarthritis of the hip: A randomized, double-blind,
placebo-controlled trial. _Arthritis Rheum._ 56, 2278–2287. https://doi.org/10.1002/art.22739 (2007). Article CAS PubMed Google Scholar * Mei-Dan, O. _et al._ The anterior approach for a
non-image-guided intra-articular hip injection. _Arthroscopy_ 29, 1025–1033. https://doi.org/10.1016/j.arthro.2013.02.014 (2013). Article PubMed Google Scholar * Wixson, M. C., Jamadar,
D. A., Moser, S. E. & Shuchman, D. N. Fluoroscopically guided lateral approach hip injection. _Fed. Pract._ 36, 300–305 (2019). PubMed PubMed Central Google Scholar * Masoud, M. A.
& Said, H. G. Intra-articular hip injection using anatomic surface landmarks. _Arthrosc. Tech._ 2, e147-149. https://doi.org/10.1016/j.eats.2013.01.004 (2013). Article PubMed PubMed
Central Google Scholar * Byrd, J. W. & Jones, K. S. Prospective analysis of hip arthroscopy with 2-year follow-up. _Arthroscopy_ 16, 578–587. https://doi.org/10.1053/jars.2000.7683
(2000). Article CAS PubMed Google Scholar * Yiannakopoulos, C., Sachinis, N., Oluku, J. & Dellis, S. Intra-articular hip injection using anatomical and radiological landmarks without
the use of ultrasound or radiological guidance. _Cureus_ 14, e23581. https://doi.org/10.7759/cureus.23581 (2022). Article PubMed PubMed Central Google Scholar * Ofori, K., Gordon, S.
W., Akrobortu, E., Ampene, A. A. & Darko, E. O. Estimation of adult patient doses for selected X-ray diagnostic examinations. _J. Radiat. Res. Appl. Sci._ 7, 459–462 (2014). Google
Scholar * Kennedy, D. J. _et al._ Vasovagal rates in flouroscopically guided interventional procedures: A study of over 8000 injections. _Pain Med._ 14, 1854–1859.
https://doi.org/10.1111/pme.12241 (2013). Article PubMed Google Scholar * Okike, K. _et al._ Rapidly destructive hip disease following intra-articular corticosteroid injection of the hip.
_J. Bone Jt. Surg. Am._ 103, 2070–2079. https://doi.org/10.2106/jbjs.20.02155 (2021). Article Google Scholar * Krych, A. J. _et al._ Limited therapeutic benefits of intra-articular
cortisone injection for patients with femoro-acetabular impingement and labral tear. _Knee Surg. Sports Traumatol. Arthrosc._ 22, 750–755. https://doi.org/10.1007/s00167-014-2862-3 (2014).
Article PubMed Google Scholar * Subedi, N., Chew, N. S., Chandramohan, M., Scally, A. J. & Groves, C. Effectiveness of fluoroscopy-guided intra-articular steroid injection for hip
osteoarthritis. _Clin. Radiol._ 70, 1276–1280. https://doi.org/10.1016/j.crad.2015.07.002 (2015). Article CAS PubMed Google Scholar * Zhong, H. M. _et al._ Intra-articular steroid
injection for patients with hip osteoarthritis: A systematic review and meta-analysis. _Biomed. Res. Int._ 2020, 6320154. https://doi.org/10.1155/2020/6320154 (2020). Article PubMed PubMed
Central Google Scholar * Aksoy, A., Gulcu, A., Tuna, M. M. & Aslan, A. Radiologically guided versus blinded intra-articular injection in patients with hip osteoarthritis: A
retrospective comparative study. _Clin. Med. Insights Arthritis Musculoskelet. Disord._ 15, 11795441221118920. https://doi.org/10.1177/11795441221118920 (2022). Article PubMed PubMed
Central Google Scholar * Kurup, H. & Ward, P. Do we need radiological guidance for hip joint injections?. _Acta Orthop. Belg._ 76, 205–207 (2010). PubMed Google Scholar * Graf, D.
N., Thallinger, A., Zubler, V. & Sutter, R. Intraarticular steroid injection in hip and knee with fluoroscopic guidance: Reassessing safety. _Radiology_ 304, 363–369.
https://doi.org/10.1148/radiol.210668 (2022). Article PubMed Google Scholar * Robinson, P., Keenan, A. M. & Conaghan, P. G. Clinical effectiveness and dose response of image-guided
intra-articular corticosteroid injection for hip osteoarthritis. _Rheumatology (Oxford)_ 46, 285–291. https://doi.org/10.1093/rheumatology/kel217 (2007). Article CAS PubMed Google Scholar
Download references ACKNOWLEDGEMENTS We wish to thank the Department of Orthopaedics, Faculty of Medicine, Thammasat University, and Thammasat University Hospital for their kind support.
We also wish to thank you for the assistance from proofreaders and editors. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Orthopaedics, Faculty of Medicine, Thammasat
University, Pathum Thani, Thailand Rakop Taveesuksiri, Chane Jitapunkul & Adinun Apivatgaroon * Department of Clinical Epidemiology, Faculty of Medicine, Thammasat University, Pathum
Thani, Thailand Prapasri Kulalert Authors * Rakop Taveesuksiri View author publications You can also search for this author inPubMed Google Scholar * Prapasri Kulalert View author
publications You can also search for this author inPubMed Google Scholar * Chane Jitapunkul View author publications You can also search for this author inPubMed Google Scholar * Adinun
Apivatgaroon View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS Conception and design R.T., A.A. Analysis and interpretation of the data R.T.,
P.K., A.A. Drafting of the article R.T., C.J., A.A. Critical revision of the article for important intellectual content R.T., P.K., A.A. Final approval of the article R.T., P.K., C.J., A.A.
Provision of study materials or patients A.A. Statistical expertise P.K., A.A. Administrative, technical, or logistic support C.J., A.A. Collection and assembly of data R.T., A.A.
CORRESPONDING AUTHOR Correspondence to Adinun Apivatgaroon. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a
Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit
to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are
included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons
licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of
this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Taveesuksiri, R., Kulalert, P., Jitapunkul, C. _et al._
Efficacy of three different techniques in the fluoroscopy-guided intra-articular steroid injection of the hip: a randomized controlled trial. _Sci Rep_ 13, 17214 (2023).
https://doi.org/10.1038/s41598-023-44595-5 Download citation * Received: 06 March 2023 * Accepted: 10 October 2023 * Published: 11 October 2023 * DOI:
https://doi.org/10.1038/s41598-023-44595-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative