Play all audios:
ABSTRACT Although patients who underwent night-time resuscitation for out-of-hospital cardiac arrest (OHCA) had worse clinical outcomes than those who underwent day-time resuscitation, the
differences between the outcomes of patients with OHCA who underwent extracorporeal cardiopulmonary resuscitation (ECPR) in the day-time and night-time remain unclear. We analyzed data from
the Study of Advanced Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan. Patients were categorized according to whether they received treatment during the
day-time or night-time. The primary outcomes were survival to hospital discharge and favorable neurological outcome at discharge, and the secondary outcomes were estimated low-flow time,
implementation time of ECPR, and complications due to ECPR. A multivariate logistic regression model adjusted for confounders was used for comparison. Among the 1644 patients, the night-time
patients had a significantly longer ECMO implementation time and estimated low-flow time than the day-time patients, along with a significantly higher number of complications than the
day-time patients. However, the survival and neurologically favorable survival rates did not differ significantly between the groups. Thus, although patients who underwent ECPR at night had
an increased risk of longer implementation time and complications, their clinical outcomes did not differ from those who underwent day-time ECPR. SIMILAR CONTENT BEING VIEWED BY OTHERS
PROMISING CANDIDATES FOR EXTRACORPOREAL CARDIOPULMONARY RESUSCITATION FOR OUT-OF-HOSPITAL CARDIAC ARREST Article Open access 17 December 2020 EXTRACORPOREAL CARDIOPULMONARY RESUSCITATION FOR
PATIENTS WITH REFRACTORY OUT-OF-HOSPITAL CARDIAC ARREST: A PROPENSITY SCORE MATCHING, OBSERVATIONAL STUDY Article Open access 30 April 2024 IMPACT OF CENTER VOLUME ON IN-HOSPITAL MORTALITY
IN ADULT PATIENTS WITH OUT‑OF‑HOSPITAL CARDIAC ARREST RESUSCITATED USING EXTRACORPOREAL CARDIOPULMONARY RESUSCITATION: A SECONDARY ANALYSIS OF THE SAVE-J II STUDY Article Open access 09
April 2024 INTRODUCTION Out-of-hospital cardiac arrest (OHCA) is a major public health problem worldwide with a high mortality rate1,2. In Japan, emergency medical services attend to >
120,000 patients with OHCA each year, and the 1-month survival rate of patients with OHCA was only 6–7% in recent years3, despite improvements in cardiopulmonary resuscitation (CPR) skills
and widespread availability of automated external defibrillators (AED) among the general population3,4. Patients who underwent night-time resuscitation for OHCA had worse outcomes than those
who underwent day-time resuscitation5,6,7, possibly because of compromised alertness and performance of medical staff during night-time shifts, as well as the reduced number of medical
staff members during night-time compared with day-time shifts8. Extracorporeal cardiopulmonary resuscitation (ECPR) is an advanced emergency rescue therapy for patients with OHCA who do not
achieve a return of spontaneous circulation (ROSC) in the emergency department (ED). Patients with OHCA who underwent ECPR had better outcomes than those who received traditional
resuscitation8,9,10,11,12,13,14. However, considering that ECPR requires many human and healthcare resources, night-time ECPR could lead to worse outcomes, longer ECMO implementation
durations, more complications related to ECMO cannulation, and a lower survival rate than day-time ECPR. Although the differences in the characteristics and clinical outcomes among
in-hospital cardiac arrest (IHCA) patients who underwent ECPR by treatment time have previously been reported15, the differences among OHCA patients remain uninvestigated. Considering that
differences in the quality of resuscitation can be influenced by prehospital circumstances, OHCA patients might have more differences in outcomes based on when the ECPR occurred. Therefore,
we assessed the implementation time-related differences in clinical characteristics and outcomes in patients with OHCA treated with ECPR. METHODS STUDY DESIGN AND SETTING We analyzed data
from the Study of Advanced Life Support for Ventricular Fibrillation with Extracorporeal Circulation in Japan (SAVE-JII study)16, a retrospective large multicenter registry study that
examined the effectiveness of ECPR on clinical outcomes in Japan between January 1, 2013, and December 31, 2018. This study was registered in the University Hospital Medical Information
Network Clinical Trials Registry (UMIN000036490). The study protocol was approved by the ethics committee of Tokyo Medical and Dental University Hospital (M2019-018) and all research was
performed in accordance with relevant regulations. The requirement for informed consent was waived in all the participating institutions by the ethics committee of Tokyo Medical and Dental
University Hospital because of the retrospective nature of the study. Twenty-four hours a day for ECPR were available in all facilities that participated in this study, and over 90% of
facilities had emergency physicians working around the clock. Cardiologists, cardiovascular surgeons, and radiologists were available 24 h a day at 52.8%, 14.7%, and 3.0% of facilities,
respectively16. Regarding ECMO implementation, ultrasonography was used to check the site of ECMO catheter insertion and the position of the guidewire at the inferior vena cava. The
positioning of the ECMO catheter was checked by X-ray before ECMO pump-on and/or CT scan after ECMO pump-on. STUDY POPULATION The inclusion criteria were as follows: (1) patients aged ≥ 18
years and (2) patients with OHCA treated with ECPR. We excluded patients who met at least one of the following criteria: (1) transfer to a participating institution after receiving treatment
in another hospital; (2) denial to participate in the study through their family or other agents; (3) implementation of ECPR after ROSC and/or after intensive care unit (ICU) admission; (4)
the etiology of non-cardiac arrest was aortic dissection, hypothermia, primary cerebral disorder, infection, drug intoxication, trauma, suffocation, or drowning; and, (5) missing data for
survival at hospital discharge or neurological outcomes at hospital discharge. DATA COLLECTION The following data on patient characteristics, prehospital information, time course,
complications, and outcomes were collected from the SAVE-J II study data: age, sex, year of admission, incidence of witnessed cardiac arrest (CA) and bystander CPR, initial cardiac rhythm,
etiology of CA, CA due to acute coronary syndrome (ACS), location of CA, center volume, complications of ECPR implementation, survival rate at hospital discharge, and neurological outcomes
at hospital discharge. Missing data other than for primary outcomes were deleted in each analysis. DEFINITIONS Indications for ECPR followed those established by each institution. Based on
previous studies, day-time was 7:00–22:59, and night-time was defined as 23:00–6:596,7,17. Initial shockable rhythm was defined as ventricular fibrillation and pulseless ventricular
tachycardia. ACS was diagnosed by coronary angiography. With respect to center volume, a high-volume center was defined as an institution performing more than 20 cases of ECPR for OHCA
patients per year, while a low-volume center was defined as performing 19 or fewer cases per year, based on previous studies18,19 Estimated low-flow time was defined as the interval from
emergency medical services (EMS) dispatch to ECMO pump-on in cases with bystander CPR or from EMS arrival to ECMO pump-on in cases without bystander CPR. ECMO implementation time was defined
as the duration from ED arrival to ECMO pump-on. ECMO complications were defined as cannulation site bleeding and/or hematoma, retroperitoneal hematoma due to cannulation failure, and ECMO
catheter malpositioning. ECMO catheter malpositioning was defined as cannulation of the wrong vessel, requiring repositioning or reinsertion of the catheter. Interventions for
cannulation-site bleeding and retroperitoneal hematoma were defined as hemostasis achieved through surgical or endovascular treatment. OUTCOME MEASURES We defined primary outcomes as
survival to hospital discharge and favorable neurological outcomes at discharge. A favorable neurological outcome was defined as a cerebral performance category (CPC) score of 1 or 220.
Secondary outcomes were defined as estimated low-flow time, ECMO implementation time, and complications due to ECMO implementation. STATISTICAL ANALYSIS We divided the enrolled patients into
two groups by time of ECMO implementation: the day-time and night-time groups. In the univariate analysis, we used the Student’s t-test or Mann–Whitney U test to compare continuous
variables and the χ2 or Fisher exact test to compare categorical variables, as appropriate. Categorical variables were reported as numbers and percentages, whereas continuous variables were
reported as medians and interquartile ranges (IQR). Univariable and multivariable logistic regression models were used to assess the primary and secondary outcomes. We incorporated age, sex,
witnessed cardiac arrest, bystander CPR, initial shockable cardiac rhythm, diagnosis of ACS, estimated low-flow time, and night-time occurrence into the multivariate model to assess primary
outcomes. These variables were selected a priori and were clinically plausible and well-known confounders. To assess secondary outcomes in the multivariate model, we incorporated year of
admission, use of ultrasound machines, ECMO implementation in the ER, center volume, and night-time occurrence. These variables were incorporated into the multivariate model of the secondary
outcomes based on the results of the univariate analysis (cutoff: p < 0.05) and the rule of 10 events per variable. Variance inflation factor analysis indicated that there was no
multicollinearity among the variables in this study. To further explore the robustness of our main multivariate analysis, we conducted an additional analysis using propensity score matching
(PSM) followed by univariate analysis. The matching was based on same variables used in the primary multivariate analysis, with a 1:1 ratio using the caliper matching method.Inter-group
comparisons of the outcomes among the propensity score-matched subjects were performed using the χ2 test. All statistical analyses were performed using R software (version 4.2.2; R
Foundation for Statistical Computing, Vienna, Austria). All reported _p_ values were two-sided, and _p_ values < 0.05 were considered statistically significant. The associations between
hospital arrival time of the day, total number of patients with OHCA who underwent ECPR, and patients with OHCA with survival to hospital discharge, and survival and complication rates by
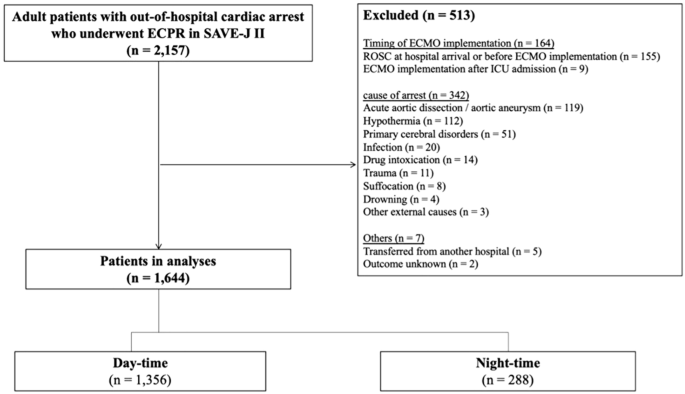
dividing hospital arrival time into 2-h intervals are shown in Figs. 2 and 3. RESULTS Figure 1 shows the patient selection diagram. Among the 2157 potentially eligible patients, we analyzed
1644 patients; 1356 (82.5%) and 288 (17.5%) patients were admitted at the day and night-time, respectively. Table 1 presents the patient characteristics of the two groups. Patients in the
night-time group were older than those in the day-time group (mean (IQR) = 56 [45–66] vs. 61 years [50–69], p < 0.001). Cardiac arrests due to ACS were more common during the daytime
(59.9% vs. 51.7%, p = 0.012). There were no significant differences between the two groups by sex, witnessed OHCA, bystander CPR, initial shockable cardiac rhythm, cardiac etiology, and
center volume. More patients were witnessed in public spaces during the day-time than during the night (57.9% vs. 34.4%, p < 0.001). More than 99% of patients (1630/1644) underwent ECPR
in the ER or catheterization room. ECMO implementation in the catheterization room was more common in the day-time than in the night-time (36.7% vs. 29.2%, p = 0.034). Table 2 shows the
primary and secondary outcomes. Compared to the day-time group, the night-time group had a significantly longer time from hospital arrival to ECMO implementation (median (IQR) = 21 min
[15–31] vs. 26 min [18–39], p < 0.001) and a longer estimated low-flow time (54 min [45–65] vs. 58 min [48–72], p < 0.001). The number of patients who underwent ECMO in the
catheterization room was higher in the day-time group than that in the night-time group. Ultrasound-guided vascular access was performed in 428 patients (26.0%), with no significant
differences between the two groups (day-time: 26.0%, night-time: 26.0%, p = 1.00). Complications associated with ECMO implementation were observed in 346 patients (21.0%) (day-time: 20.1%,
night-time: 25.3%, p = 0.056). The most common complication was cannulation site bleeding in 234 patients (14.2%) (day-time: 14.6%, night-time: 12.5%, p = 0.40), followed by ECMO catheter
malposition in 81 patients (4.9%) (day-time: 4.4%, night-time: 7.6%, p = 0.024). Among the patients with cannulation site bleeding, 43 (2.6%) (day-time: 2.7%, night-time: 2.1%, p = 0.69)
required hemostasis by surgical or endovascular treatment. Figure 2 shows the number of patients with OHCA treated by ECPR and patients who survived to hospital discharge in each 2-h time
period. The highest number of cases of ECPR implementation in patients with OHCA occurred between 9:00 and 11:00 am, whereas the smallest number of cases occurred between 1:00 and 3:00 am.
Figure 3 shows the rate of survival to hospital discharge, neurologically favorable survival, and complications associated with ECMO implementation in each 2-h period. There were no
significant variations in survival or complication rates between the two time periods. The results of the univariate and multivariate analyses are summarized in Table 3. In the multivariate
analysis adjusted for age, sex, witnessed status, bystander CPR status, initial rhythm (shockable or not), diagnosis of ACS, and estimated low-flow time, night-time resuscitation was not an
independent risk factor for survival to hospital discharge or neurologically favorable survival in either outcome (survival: odds ratios [OR] = 0.88 [95% confidence interval (CI) 0.64,
1.21]; neurologically favorable survival: OR = 0.96 [95% CI 0.65, 1.43]). PSM created 147 matched pairs in each night-time and day-time group. Table 4 presents the patient characteristics of
the two groups after PSM. The absolute standardised mean difference values for each variable were < 0.1, which indicated that a well-matched balance had been achieved. As with the
multivariate analysis, there were no significant differences between the groups in the rate of survival to hospital discharge or favorable neurological outcomes at discharge (Tables 3, 5).
Although there were no significant differences in the clinical outcomes, the night-time group had a significantly higher number of complications than the day-time group (OR [95% CI]; 1.40
[1.03–1.89]), as per the multivariate analysis adjusted for year of admission, ECMO implementation in the ER, employment of ultrasound-guided vascular access, and center volume. The
relationships between the number of patients according to the year of admission, along with the outcomes, are shown in Supplementary Table S6. The number of patients increased each year.
DISCUSSION In this retrospective study, we examined the differences in clinical outcomes and complications between day-time and night-time ECMO implementation in 1644 patients with OHCA who
underwent ECPR. Compared with the day-time group, the night-time group had a longer ECMO implementation, estimated low-flow time, and more complications related to ECMO implementation.
However, no differences in the survival rates or neurologically favorable survival rates were observed between the groups. To the best of our knowledge, this is the first multicenter study
to report the differences between the time of day and the clinical and complication-related outcomes in patients with OHCA who underwent ECPR. ECPR requires more medical staff than
conventional CPR (CCPR), including emergency physicians, nurses, and medical engineers, and is a highly invasive treatment with various potential complications21. Consistent with these
facts, in our study, the night-time group had a longer ECMO implementation time and estimated low-flow time compared with the day-time group. Additionally, significantly more complications
due to ECMO implementation were observed in the night-time group than in the day-time group. These results suggest that the speed and accuracy of ECPR implementation could be lower during
the night-time than during the day-time. Although the causal relationship between the lower speed and accuracy of ECPR, as well as the higher incidence of complications in the night-time
group, could not be established because of the study design, the differences in the working styles between the day and night-time could have influenced these results. Medical staff members
have been reported to experience fatigue, loss of concentration, and circadian rhythm disruption during the night-time resuscitation8. These factors could lead to slower and/or inappropriate
ECPR cannulation. In this study, ECMO implementation in the catheterization room was more frequent during the day-time than the night-time. One possible explanation for this difference was
that more staff, including doctors, nurses, and technicians, could be available, and cardiologists were available in the catheterization room in the day-time group. Therefore, the expertise
and experience of the staff who joined ECMO implementation may have varied by the time of day. However, ECPR was available 24 h a day in all the facilities that participated in this study.
This aspect could also affect the quality of ECMO implementation. Although a longer duration of ECMO implementation and higher incidence of complications were observed in the night-time
group, there were no significant differences in the clinical outcomes between the two groups in this study. These results suggest that most complications with ECMO implementation are not
critical enough to affect the survival rate; however, we could not consider the severity of the complications in this study. Additionally, patients who died shortly after hospital arrival
were less likely to undergo examinations for complications; therefore, this study may have had a survivor bias. Although complications with ECMO implementation were reported to be factors
that could lead to hesitation in ECPR administration21, our results indicated that the time of day did not discourage physicians from implementing ECMO. Patients with OHCA who underwent only
CCPR in the night were reported to have a lower survival rate than those who underwent only CCPR in the day5,6,7. Therefore, prompt and reliable initiation of ECMO could be necessary to
ensure a favorable prognosis, with low-flow time having the greatest impact on clinical outcomes22,23. One possible explanation for these discrepancies between previous studies and our
results is that ECPR would be more effective than CCPR in maintaining circulation for neurologically favorable survival12,24,25. Another possible explanation for the differences between
outcomes is body temperature. In patients with OHCA, targeted temperature management (TTM) is recommended for post-cardiac arrest syndrome26,27. In patients treated with ECPR, body
temperature can be strictly controlled using a heat exchanger in the ECMO circuit, and several studies have reported improved outcomes with a combination of ECPR and TTM in patients with
OHCA28,29. Additionally, cooler temperatures at night-time compared to those in the day-time may have had a positive impact on neurological prognosis30. As the relationship between the
prognosis of patients who have undergone ECPR and body temperature has not been directly investigated, large-scale studies focusing on temperature are necessary in the future. The findings
of the present study are strengthened by the fact that we directly assessed 2157 patients receiving ECPR using a large-scale multicenter database from the SAVE-J II study from 36 hospitals.
However, this study had some limitations. First, the retrospective design was prone to residual confounding factors, as we did not have access to OHCA-specific characteristics or detailed
information regarding patient characteristics and comorbidities. Second, the treatment protocol for ECPR implementation, including the patient selection, timing, and location, varied
according to the participating hospitals in this study. Furthermore, we only included the patients who did not achieve ROSC upon hospital arrival and underwent ECPR immediately upon arrival
at the hospital. These factors could also affect the outcomes. Third, detailed information about ECPR implementation (e.g., number of medical staff in each day-time and night-time shift,
details of the physicians who cannulated for ECPR, method of cannulation, availability of the catheterization room at night, physicians’ experience regarding ECPR implementation at each
hospital) and the severity of complications due to ECMO cannulation was not obtained; these factors could have affected outcomes. Fourth, this study only included patients who underwent
ECPR. This criterion might result in selecting the subset of patients with better prehospital care or quicker response times, which could lead to selection bias. Fifth, although head CT
scans were performed for all included patients after ECMO implementation, neurological complications directly related to ECMO cannulation were not evaluated. Sixth, this study only included
patients with OHCA who underwent ECPR; therefore, it is difficult to generalize the findings to actual clinical practice. Seventh, to ensure accuracy, we excluded patients whose primary
outcomes were unknown. Additionally, physicians might select patients who were expected to survive with neurologically favorable outcomes because this study included only patients with OHCA
who underwent ECPR. Although the patient characteristics were not significantly different between the night and day-time groups, these findings are different from those of recent studies6,7.
Therefore, a larger study including patients with OHCA treated with both CCPR and ECPR is required. Despite these limitations, to the best of our knowledge, this is the first study to
evaluate implementation time-related differences in the clinical characteristics and outcomes of patients with OHCA treated with ECPR. CONCLUSION ECPR at night for patients with OHCA
requires a longer ECMO implementation time than that in the day-time, and ECMO implementation at night is associated with more complications than that in the day. However, survival and
neurologically favorable survival rates did not differ between patients who underwent day-time and night-time ECMO implementation. DATA AVAILABILITY The data supporting the findings of this
study are available from the corresponding author on reasonable request. REFERENCES * Merchant, R. M. _et al._ Part 1: Executive summary: 2020 American Heart Association guidelines for
cardiopulmonary resuscitation and emergency cardiovascular care. _Circulation._ 142, S337–S357 (2020). Article PubMed Google Scholar * Perkins, G. D. _et al._ European resuscitation
council Guidelines 2021: Executive summary. _Resuscitation._ 161, 1–60 (2021). Article PubMed Google Scholar * Japan—Ministry of internal affairs and communications; 2022. Current Status
of Emergency and Rescue Services. https://www.fdma.go.jp/publication/rescue/items/kkkg_r04_01_kyukyu.pdf (accessed 14 March 2023). * Japan–Japan Heart Foundation. Prevalence of AED.
https://www.jhf.or.jp/check/aed/spread/ (accessed 14 March 2023). * Lin, P., Shi, F., Wang, L. & Liang, Z.-A. Nighttime is associated with decreased survival for out of hospital cardiac
arrests: A meta-analysis of observational studies. _Am. J. Emerg. Med._ 37, 524–529 (2019). Article PubMed Google Scholar * Kato, K. _et al._ Association between time of out-of-hospital
cardiac arrest and survival: Examination of the all-Japan Utstein registry and comparison with the 2005 and 2010 international resuscitation guidelines. _Int. J. Cardiol._ 324, 214–220
(2021). Article PubMed Google Scholar * Takayama, W., Endo, A., Koguchi, H., Murata, K. & Otomo, Y. Differences in durations, adverse events, and outcomes of in-hospital
cardiopulmonary resuscitation between day-time and night-time: An observational cohort study. _Resuscitation._ 137, 14–20 (2019). Article PubMed Google Scholar * Ganesan, S. _et al._ The
impact of shift work on sleep, alertness and performance in healthcare workers. _Sci. Rep._ 9, 4635 (2019). Article ADS PubMed PubMed Central Google Scholar * Yannopoulos, D. _et al._
Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): A phase 2, single centre, open-label, randomised controlled
trial. _Lancet._ 396, 1807–1816 (2020). Article PubMed PubMed Central Google Scholar * Downing, J. _et al._ How effective is extracorporeal cardiopulmonary resuscitation (ECPR) for
out-of-hospital cardiac arrest? A systematic review and meta-analysis. _Am. J. Emerg. Med._ 51, 127–138 (2022). Article PubMed Google Scholar * Su, J. K., Hyun, J. K., Hee, Y. L., Hyeong,
S. A. & Sung, W. L. Comparing extracorporeal cardiopulmonary resuscitation with conventional cardiac resuscitation: A meta-analysis. _Resuscitation._ 103, 106–116 (2016). Article
Google Scholar * Wang, G. N. _et al._ Comparison of extracorporeal and conventional cardiopulmonary resuscitation: A meta-analysis of 2260 patients with cardiac arrest. _World J. Emerg.
Med._ 8, 5–11 (2017). Article CAS PubMed PubMed Central Google Scholar * Rycus, P. & Stead, C. Extracorporeal life support organization registry report 2022. _J. Cardiac. Crit.
Care._ 6, 100–102 (2022). Article Google Scholar * Henry, B., Verbeek, P. R. & Cheskes, S. Extracorporeal cardiopulmonary resuscitation in out-of-hospital cardiac arrest: Ethical
considerations. _Resuscitation._ 137, 1–6 (2019). Article CAS PubMed Google Scholar * Tonna, J. E., _et al._ Resuscitation using ECPR during in-hospital cardiac arrest (RESCUE-IHCA)
mortality prediction score and external validation. _JACC Cardiovasc. Interv_. 15, 237–247 (2022) * Hifumi, T. _et al._ Variability of extracorporeal cardiopulmonary resuscitation practice
in patients with out-of-hospital cardiac arrest from the emergency department to intensive care unit in Japan. _Acute Med. Surg._ 8, e647 (2021). Article PubMed PubMed Central Google
Scholar * Wolfe, H. A. _et al._ Association between time of day and CPR quality as measured by CPR hemodynamics during pediatric in-hospital CPR. _Resuscitation._ 153, 209–216 (2020).
Article PubMed PubMed Central Google Scholar * Kayo, M., _et al._ Impact of center volume on in-hospital mortality in adult patients with out-of-hospital cardiac arrest resuscitated
using extracorporeal cardiopulmonary resuscitation: A secondary analysis of the SAVE-J II study. _Sci. Rep_. 14. 8309 (2024). * Ng, P. Y., _et al._ Effect of hospital case volume on clinical
outcomes of patients requiring extracorporeal membrane oxygenation: a territory-wide longitudinal observational study. _J. Thorac. Dis_. 14. 1802–1814 (2022). * Cummins RO, _et al._
Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: The Utstein Style. A statement for health professionals from a task force of the American Heart
Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. _Circulation_. 84, 960–975 (1991). * Nguyen, M. L. _et
al._ Traumatic and hemorrhagic complications after extracorporeal cardiopulmonary resuscitation for out-of-hospital cardiac arrest. _Resuscitation._ 157, 225–229 (2020). Article PubMed
PubMed Central Google Scholar * Ko, R. E. _et al._ The differential neurologic prognosis of low-flow time according to the initial rhythm in patients who undergo extracorporeal
cardiopulmonary resuscitation. _Resuscitation._ 148, 121–127 (2020). Article PubMed Google Scholar * Debaty, G. _et al._ Prognostic factors for extracorporeal cardiopulmonary
resuscitation recipients following out-of-hospital refractory cardiac arrest A systematic review and meta-analysis. _Resuscitation._ 112, 1–10 (2017). Article PubMed Google Scholar *
Mandigers L, _et al._ Systematic review and meta-analysis comparing low-flow duration of extracorporeal and conventional cardiopulmonary resuscitation. _Interact Cardiovasc. Thorac. Surg_.
35, ivac219 (2022). * Bartos, J. A. _et al._ Improved survival with extracorporeal cardiopulmonary resuscitation despite progressive metabolic derangement associated with prolonged
resuscitation. _Circulation._ 141, 877–886 (2020). Article CAS PubMed PubMed Central Google Scholar * Panchal, A. R. _et al._ Part 3: Adult basic and advanced life support: 2020
American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. _Circulation._ 142, S366-468 (2020). Article PubMed Google Scholar * Nolan, J.
P. _et al._ European resuscitation council and European society of intensive care medicine guidelines. Post-resuscitation care. _Resuscitation._ 161, 220–269 (2021). Article PubMed Google
Scholar * Nakashima, T. _et al._ Association of intentional cooling, achieved temperature and hypothermia duration with in-hospital mortality in patients treated with extracorporeal
cardiopulmonary resuscitation: An analysis of the ELSO registry. _Resuscitation._ 177, 43–51 (2022). Article PubMed Google Scholar * Sakurai, T., Kaneko, T., Yamada, S. & Takahashi,
T. Extracorporeal cardiopulmonary resuscitation with temperature management could improve the neurological outcomes of out-of-hospital cardiac arrest: A retrospective analysis of a
nationwide multicenter observational study in Japan. _J. Intensive Care._ 10, 30 (2022). Article PubMed PubMed Central Google Scholar * Yoshimura, S. _et al._ Association between initial
body temperature on hospital arrival and neurological outcome among patients with out-of-hospital cardiac arrest: A multicenter cohort study (the CRITICAL study in Osaka, Japan). _BMC
Emerg. Med._ 22, 84 (2022). Article PubMed PubMed Central Google Scholar Download references ACKNOWLEDGEMENTS We thank all the included patients and their families, physicians, nurses,
clinical engineers, paramedics, and staff members. AUTHOR INFORMATION Author notes * A list of authors and their affiliations appears at the end of the paper. AUTHORS AND AFFILIATIONS *
Department of Critical Care Medicine and Trauma, National Hospital Organization Disaster Medical Center, Tokyo, Japan Hazuki Koguchi & Yasuhiro Otomo * Trauma and Acute Critical Care
Center, Tokyo Medical and Dental University Hospital, Tokyo, Japan Hazuki Koguchi, Wataru Takayama, Yasuhiro Otomo & Koji Morishita * Department of Emergency and Critical Care Medicine,
Hyogo Emergency Medical Center, Kobe, Japan Akihiko Inoue * Department of Emergency and Critical Care Medicine, St. Luke’s International Hospital, Tokyo, Japan Toru Hifumi * Department of
Emergency Medicine, Teikyo University School of Medicine, Tokyo, Japan Tetsuya Sakamoto * Department of Emergency Medicine, Kagawa University School of Medicine, Kagawa, Japan Yasuhiro
Kuroda * Osaka Saiseikai Senri Hospital, Suita, Japan Asae Senda * Saitama Red Cross Hospital, Saitama, Japan Hajime Suzuki & Atsunori Tanimoto * Tokyo Metropolitan Bokutoh Hospital,
Tokyo, Japan Kanta Kitagawa * Sapporo Medical University, Sapporo, Japan Yoichi Katayama * Hyogo Emergency Medical Center, Kobe, Japan Nobuaki Igarashi, Masayuki Kawano & Yuji Kuroki *
Teikyo University Hospital, Itabashi, Japan Tadashi Umehara, Yukari Sasaki & Naoki Tominaga * Nippon Medical School, Bunkyo City, Japan Takuro Hamaguchi & Takuma Sakai * Yokohama
City University Medical Center, Yokohama, Japan Takeru Abe, Hiroaki Hanafusa, Yuki Yamaoka & Yumi Kakizaki * Toyooka Public Hospital, Toyooka, Japan Shinya Sakato * Hokkaido University
Hospital, Sapporo, Japan Shiho Kashiwabara, Takashi Kadoya, Kayo Misumi & Takaomi Kobayashi * Imperial Gift Foundation Saiseikai, Utsunomiya Hospital, Utsunomiya, Japan SouYamada &
Masakazu Kobayashi * Tohoku University Graduate School of Medicine, Sendai, Japan Naoko Akashi * Nippon Medical School Tama Nagayama Hospital, Tama, Japan Masamune Kuno * Red Cross Maebashi
Hospital, Maebashi, Japan Jun Maruyama * Osaka Mishima Emergency Critical Care Center, Takatsuki, Japan Hitoshi Kobata, Mitsuhito Soh, Kasumi Shirasaki & Daiki Shiba * St. Luke’s
International Hospital, Chuo City, Japan Shutaro Isokawa * Dokkyo Medical University, Mibu, Japan Masatoshi Uchida * Nihon University Hospital, Chiyoda City, Japan Atsushi Sakurai &
Hirotaka Tatsukawa * Omihachiman Community Medical Center, Omihachiman, Japan Marie Nishikawa & Mitsuaki Kojima * Tokyo Women’s Medical University Medical Center East, Shinjuku City,
Japan Ryohei Kosaki * Kimitsu Chuo Hospital, Kisarazu, Japan Takashi Shimazui * Kobe City Medical Center General Hospital, Kobe, Japan Hiroki Kinoshita * Gunma University Graduate School of
Medicine, Maebashi, Japan Yusuke Sawada, Ryo Yamamoto & Yuya Masuzawa * Keio University School of Medicine, Minato, Japan Kazuki Matsumura * Osaka University Graduate School of Medicine,
Suita, Japan Junya Shimazaki Authors * Hazuki Koguchi View author publications You can also search for this author inPubMed Google Scholar * Wataru Takayama View author publications You can
also search for this author inPubMed Google Scholar * Yasuhiro Otomo View author publications You can also search for this author inPubMed Google Scholar * Koji Morishita View author
publications You can also search for this author inPubMed Google Scholar * Akihiko Inoue View author publications You can also search for this author inPubMed Google Scholar * Toru Hifumi
View author publications You can also search for this author inPubMed Google Scholar * Tetsuya Sakamoto View author publications You can also search for this author inPubMed Google Scholar *
Yasuhiro Kuroda View author publications You can also search for this author inPubMed Google Scholar CONSORTIA THE SAVE-J II STUDY GROUP * Asae Senda * , Hajime Suzuki * , Atsunori Tanimoto
* , Kanta Kitagawa * , Yoichi Katayama * , Nobuaki Igarashi * , Masayuki Kawano * , Yuji Kuroki * , Tadashi Umehara * , Yukari Sasaki * , Naoki Tominaga * , Takuro Hamaguchi * , Takuma
Sakai * , Takeru Abe * , Hiroaki Hanafusa * , Yuki Yamaoka * , Yumi Kakizaki * , Shinya Sakato * , Shiho Kashiwabara * , Takashi Kadoya * , Kayo Misumi * , Takaomi Kobayashi * , SouYamada *
, Masakazu Kobayashi * , Naoko Akashi * , Masamune Kuno * , Jun Maruyama * , Hitoshi Kobata * , Mitsuhito Soh * , Kasumi Shirasaki * , Daiki Shiba * , Shutaro Isokawa * , Masatoshi Uchida *
, Atsushi Sakurai * , Hirotaka Tatsukawa * , Marie Nishikawa * , Mitsuaki Kojima * , Ryohei Kosaki * , Takashi Shimazui * , Hiroki Kinoshita * , Yusuke Sawada * , Ryo Yamamoto * , Yuya
Masuzawa * , Kazuki Matsumura * & Junya Shimazaki CONTRIBUTIONS H.K. and W.T.—study design, analysis, writing—original draft. Y.O., K.M., A.I., T.H., T.S., and Y.K.—conceptualization,
study design, writing—review and editing. All the authors have read and approved the final manuscript. CORRESPONDING AUTHOR Correspondence to Hazuki Koguchi. ETHICS DECLARATIONS COMPETING
INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER'S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and
institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY INFORMATION. RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons
Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give
appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission
under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons
licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by
statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit
http://creativecommons.org/licenses/by-nc-nd/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Koguchi, H., Takayama, W., Otomo, Y. _et al._ Differences in outcomes of
patients with out-of-hospital cardiac arrest treated with extracorporeal cardiopulmonary resuscitation between day-time and night-time. _Sci Rep_ 14, 16950 (2024).
https://doi.org/10.1038/s41598-024-67275-4 Download citation * Received: 17 January 2024 * Accepted: 09 July 2024 * Published: 23 July 2024 * DOI: https://doi.org/10.1038/s41598-024-67275-4
SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to
clipboard Provided by the Springer Nature SharedIt content-sharing initiative