Play all audios:
ABSTRACT The high mutation rate of RNA viruses provides viral populations with the ability to adapt to new environments but also makes them vulnerable to extinction due to the deleterious
effects of mutations, which is the conceptual basis for the antiviral activity of RNA mutagens. However, there are still gaps in the quantitative understanding of the dynamics between the
mutations induced by an RNA mutagen and its effects on viral fitness. To address this, we used Venezuelan Equine Encephalitis Virus (VEEV) and the potent RNA mutagen β-d-N4-hydroxycytidine
(NHC) as a model to analyze virus replication competency and mutation frequency following treatment in the total and replication-competent viral populations separately. We found that NHC
induced transition mutations in a concentration dependent manner in the total population, while the replication-competent population maintained itself within an increased, yet narrow,
mutation spectrum. The incorporation of NHC mainly happened during the positive sense RNA synthesis of VEEV. A growth kinetic analysis of VEEV population treated with NHC pointed to a lower
but more diverse distribution in mutational fitness, demonstrating that NHC-induced mutations negatively and broadly affect the fitness of the virus. Together, our study provides mechanistic
insight into how RNA mutagens affect viral population landscape and the potential of RNA mutagens as an antiviral strategy for alphaviruses. SIMILAR CONTENT BEING VIEWED BY OTHERS DEFECTIVE
VIRAL GENOMES AS THERAPEUTIC INTERFERING PARTICLES AGAINST FLAVIVIRUS INFECTION IN MAMMALIAN AND MOSQUITO HOSTS Article Open access 16 April 2021 A SINGLE AMINO ACID SUBSTITUTION IN THE
CAPSID PROTEIN OF ZIKA VIRUS CONTRIBUTES TO A NEUROVIRULENT PHENOTYPE Article Open access 26 October 2023 VENEZUELAN EQUINE ENCEPHALITIS VIRUS NON-STRUCTURAL PROTEIN 3 DICTATES
SUPERINFECTION EXCLUSION IN MAMMALIAN CELLS Article Open access 13 September 2024 INTRODUCTION Encephalitic alphaviruses including Venezuelan, eastern, and western equine encephalitis virus
(VEEV, EEEV and WEEV, respectively) are members of the family _Togaviridae_, which have an approximately 11 kb positive sense RNA genome and replicate at high titers in multiple cell types.
They are mosquito-borne, neuroinvasive, emerging RNA viruses for which no FDA-approved therapeutic exists. Since RNA viruses inherently replicate with a high mutation rate, a well-received
broad-spectrum antiviral approach has been to further increase the number of mutations within the viral genome by treatment with an RNA mutagen (reviews in1,2,3). Historically, several
antivirals, whose mechanisms were to induce mutations during replication, have been developed, including ribavirin4,5,6,7 and T-705 (also known as Favipiravir)8,9, and demonstrated an
antiviral activity against many viruses including hepatitis C virus, foot-and-mouth disease virus, lymphocytic choriomeningitis virus, and West Nile virus2,4,9,10,11,12,13,14,15. With these
broad-spectrum antiviral effects, the concept of using a RNA mutagen as an antiviral approach, which is commonly referred to as lethal mutagenesis, has been of special interest for emerging
RNA viruses, such as encephalitic alphaviruses, that often lack specific treatment options. Previous studies, however, demonstrated that well-known RNA mutagens such as ribavirin and T-705
either showed no or marginal antiviral effects against alphaviruses at a non-cytotoxic concentration16,17,18. Additionally, they exhibit a high degree of pleiotropic activities in the cells
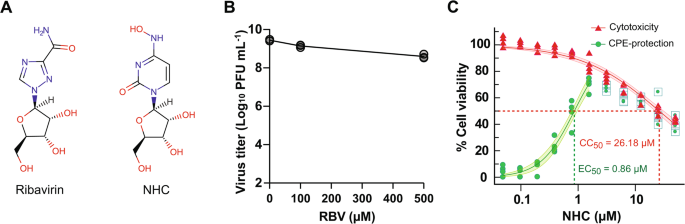
that can contribute to the antiviral effects, which would make pinpointing the activity that ultimately leads to the observed antiviral effects difficult16,19,20. Compared to ribavirin or
T-705, β-d-N4-hydroxycytidine (NHC, initial metabolite of molnupiravir, Fig. 1) exhibited potent antiviral activity against a broad-spectrum of RNA viruses including alphaviruses at a lower
range of concentrations21,22. NHC is converted to its active form (NHC-TP), and incorporated into RNA by the RNA-dependent RNA polymerase (RdRP) without causing stalling23. NHC-MP
incorporated into viral RNA induces transition mutations (preferentially C-to-U) into the nascent RNA strand by tautomerization. Molnupiravir, the metabolic prodrug form of NHC, has been
recently authorized under an emergency use authorization for the treatment of adults with mild-to-moderate COVID-19 by the Food and Drug Administration, which highlights the potential of
NHC-induced lethal mutagenesis as an effective antiviral approach for alphavirus-induced disease as well. Previous studies8,9,24,25,26 have clearly revealed that RNA mutagens induce an
increase in mutations in viral genomes and seemingly display antiviral effects. However, the mechanism by which RNA mutagen-induced viral mutations result in antiviral effects remains
unclear. For example, the relationship between mutagen concentration and mutation accumulation and the mutational threshold that viruses can endure before mutation-induced population
collapse is not known. To obtain a mechanistic insight into how RNA mutagen treatment leads to antiviral effects against alphaviruses, we studied the genetic and phenotypic changes of the
VEEV TC-83 strain with a focus on NHC-treated, replication-competent populations following a single round of replication. The potent antiviral activity of NHC against alphaviruses, seemingly
few off-target effects resulting from NHC treatment, and well-defined genetic systems of alphaviruses provide a unique platform27 to study the mechanism and potential risks of lethal
mutagenesis. In our study, we observed that NHC effectively induces mutations in the VEEV genome during replication and leads to population collapse when VEEV is serially passaged in the
presence of NHC, largely supporting lethal mutagenesis as its mechanism of antiviral action. Interestingly, however, we also found that at a single cycle period, mutation profiles of the
infectious, replication-competent population differed from those of the total population with respect to mutation frequency and response to RNA mutagen. Even at a high exposure NHC
treatment, the mutation frequency of the infectious populations did not surpass approximately 6.5 substitution per genome, while their fitness was negatively skewed. Our study demonstrates a
mutational threshold for VEEV survival and how RNA mutagens can function as an antiviral against alphaviruses. RESULTS ANTIVIRAL EFFECT OF NHC AGAINST VEEV TC-83 To study lethal
mutagenesis, we first tested the antiviral effect of two well-known RNA mutagens, ribavirin and NHC in Vero 76 cells (Fig. 1), against VEEV TC-83. The antiviral effect of ribavirin was
minimally detected as described by others28 (Fig. 1B); NHC showed a dose-dependent antiviral response in our assay with an EC50 of 0.86 µM and CC50 of 26.2 µM (Fig. 1C), which confirms data
published by others . COLLAPSE OF THE INFECTIOUS POPULATION BY NHC To see if NHC induces a collapse of the infectious population as its antiviral mechanism, we passaged VEEV TC-83 in the
presence of NHC. As a control, brequinar was used, which shows antiviral effect (EC50 = 0.16 µM, See Supplementary data for detail) by interfering with host metabolism (i.e., the pyrimidine
synthesis pathway)29. We found that NHC-treated population experienced a collapse after 4 passages in the presence of 10 µM NHC (Fig. 2A). However, virus population exposed to 1 µM NHC or
brequinar did not experience such a collapse at the end of the experiment (10 passages). Our results indicate that NHC can induce a population crash; however, a higher concentration than its
EC50 might be needed to achieve this effect. NHC REQUIRES MULTIPLE ROUNDS OF REPLICATION FOR ITS EFFICACY Next, we further sought to understand how induction of mutations by NHC results in
replication incompetent progeny virus, ultimately leading to the NHC-mediated population crash. To see if NHC’s antiviral effect requires successive rounds of viral replication, as the
mechanism suggests, we tested two MOIs, MOI = 10 for single round of replication and MOI = 0.1 for multiple rounds of replication. We used EGFP expression from a recombinant VEEV TC-83
double reporter strain27 (rVEEV TC-83-dR) as a surrogate for virus replication to evaluate the antiviral effect of NHC following treatment. The EC50 of NHC for rVEEV TC-83-dR, using EGFP
expression as the readout, was determined to be 0.52 µM, which is similar to that for non-reporter VEEV TC-83. We found that while 10 µM NHC showed only a 43.0% reduction in reporter signal
compared to the control in the single round of replication condition (i.e., high MOI.), the antiviral effect for the second round of replication observed in the low MOI condition was
significantly higher (97.9% reduction, _n_ = 6, Fig. 2B). This phenomenon was not detected with ML336, a direct antiviral against VEEV viral RNA synthesis (structure is shown Fig. 1A)30.
This result implies that the primary antiviral activity of NHC on VEEV impacts progeny virus more in subsequent rounds of replication than during the replication of the first exposed
population, which is consistent with the concept of lethal mutagenesis. NHC SHOWS A TWO-PHASE DOSE-RESPONSIVE VIRUS YIELD REDUCTION EFFICACY, LEAVING A REPLICATION-COMPETENT PROGENY VIRUS
POPULATION AT A HIGH CONCENTRATION Next, we measured the antiviral activity of NHC in a virus yield reduction assay with a broad range of NHC concentrations, ranging from 1 to 50 µM, against
TC-83 virus in Vero 76 cells. Overall, NHC treatment yielded a significant reduction in virus titer compared to the mock-treated group, (Fig. 2C) as previously reported by others21.
However, interestingly, we found that the antiviral effect did not further increase at concentrations greater than 10 µM, resulting in a similar amount of replication-competent progeny virus
titer even at 50 µM. In other words, the antiviral effect of NHC was saturated at approximately 10 µM and some fractions of the populations were still able to maintain their infectivity
when exposed to higher NHC concentrations. We detected a similar effect when we determined the relative infectivity (RNA copy number / pfu). RNA copy/pfu ratio of virus produced in the
presence of NHC increased marginally above 10 µM (Fig. 2D). This result indicates that NHC has a potent anti-VEEV effect, and the overall quality of viral genomic RNA decreases. However, NHC
treatment during a single passage was not able to abrogate replication-competent progeny virus populations even at high concentrations. NHC might need multiple rounds of replication cycles
to achieve its full antiviral effect. CONCENTRATION-DEPENDENT INCREASE OF MUTATIONS IN NHC-TREATED VIRUS POPULATION To understand how NHC-induced mutations may lead to decreased viral titers
in NHC-treated viral populations, we first determined the genomic sequences of the viral genome from the total population using a long-read bulk sequencing of PCR-amplicons covering nsP2-4
region, approximately 6 kb or 50% of the total genome (Fig. 3A. See Methods section for detail). This method allows us to analyze genomic sequences at a single molecule level with greater
accuracy (Q43, > 99.99%) and phasing than conventional short-read bulk sequencing (e.g., Illumina-based sequencing) without additional methodological needs. The analysis showed a
significant increase in mutation frequency due to NHC treatment. The mock-treated group (DMSO-treated) was determined to have a mutation-frequency of 1.30 × 10−4 s/n (_n_ = 3). The increase
in mutation frequency due to NHC treatment was concentration dependent. The mutation frequencies increased to 5.60 and 26.06 (10−4 s/n) for 1 and 10 µM NHC-treated populations, respectively,
which is an approximately 4 and 20-fold increase compared to the DMSO control. The mutation frequency increased further in the 50 µM NHC treated population with 32.65 (10−4 s/n, or
32.65-fold increase compared to the DMSO control (Fig. 3B). Our data showed that NHC is an effective RNA mutagen for VEEV and induces ~ 8-fold increase during a single passage at a
concentration that induced a population collapse in subsequent passages (i.e., 10 µM). NHC REVEALED A MUTATIONAL THRESHOLD FOR THE REPLICATION-COMPETENT VEEV POPULATION Interestingly, the
virus yield reduction experiment (Figs. 2C and 3C) indicated the presence of a residual population in the progeny virus that is replication-competent (evidenced by plaque formation) after a
single passage. We sought to better characterize the genetic landscape within this replication-competent population, apart from the total population, as the replication-competent population
establishes the progeny virus in the next round of replication under the treatment of NHC. To address this, we developed a consensus sequence-based sequencing approach using a limiting
dilution of virus in cell plates (Single Infectious Unit or SIU sequencing hereafter). Our SIU approach only determines viral sequences of populations that can replicate at the individual
infectious unit level (Fig. 3A). Because the final sequences are deduced from the consensus sequences in the clone, errors during sequencing processes can be minimized for analysis. We found
that the mutation frequency profile of replication-competent populations (Fig. 3B) differed from that of the total population. The maximum mutation frequency of the replication-competent
populations reached approximately 6.3 × 10−4 s/n, plateauing at around 10 µM of NHC, without a significant increase beyond 20 µM. This is a striking difference from the total population,
which displayed a concentration-dependent increase in mutation frequency. (_p_ < 0.0001, Two-way ANOVA test). This may indicate that VEEV population could not tolerate mutation frequency
higher than 6.3 × 10−4 s/n, and this threshold can be reached following a single round of replication with 10 µM NHC treatment. CHARACTERIZATION OF MUTATIONS INDUCED BY NHC IN THE
REPLICATION-COMPETENT POPULATION To understand more precisely how the mutations are distributed within the replication-competent population, we analyzed the mutations in each isolate (Fig.
4, and Table 1). The median number of mutations within the 5.9 kb amplicon examined from the 1 µM NHC-treated infectious population increased to 2, compared to 0 for the DMSO-treated group.
When treated with at least 10 µM of NHC, the change in the distribution of the number of mutations in the amplicon was more obvious, especially for the strands with higher number of
mutations within the amplicon. For example, while only 6.8% of the 1 µM-NHC treated SIUs had more than 5 mutations, more than 30% of the 10 µM NHC-treated SIUs had more than 5 mutations in
the same region. We also found that significant fractions of replication-competent viruses had a low number of mutations, even when treated with a high concentration of NHC. Within the 1,
10, and 50µM-treated groups, we found that 63.6%, 44.3%, and 45.5% of SIUs in those groups, respectively, contained fewer than 2 mutations within the sequenced amplicon. Particularly, more
than 12.5% of the replication-competent population was mutation-free within the amplicon in all NHC-treated groups (Table 1). This may indicate that progeny virus with a lower number of
mutations, albeit a small fraction of the population, can be produced even at a high NHC concentration, supporting the need for multiple rounds of replication to reach a population collapse
(Fig. 2A). An analysis of mutations identified in the infectious population (Fig. 4) showed all four types of mutations that can be induced by NHC24, indicating the incorporation of NHC into
viral RNA might have happened during both (-)-sense RNA and progeny genomic RNA synthesis. Unlike the study using MERS-CoV, which found an equal preference of A-to-G or U-to-C mutations
incorporated into in the viral genome by NHC24, the majority of mutations induced by NHC in VEEV were T-to-C (U-to-C in the viral genome), indicating the incorporation of the NHC occurred
during the synthesis of genomic RNA across adenosine (Fig. 4B). We did not find any specific mutational hot spots within the amplicon (Fig. 4C), which indicates that (1) the incorporation of
NHC occurred randomly, and (2) no NHC-resistant populations with mutations within nsP4, the viral RdRP gene, were selected during the treatment. NHC-TREATMENT RESULTED IN A POPULATION WITH
A NEGATIVELY-SKEWED, DIVERSIFIED FITNESS Based on our finding that NHC-treated VEEV has a minor replication-competent population with increased sequence diversity, we sought to measure the
extent of growth defects resulting from those mutations. To test this, we established a viral growth kinetic assay for single infectious units using rVEEV TC-83-dR, which, as stated
previously, allows us to use the expression of the EGFP as a surrogate for viral replication. To evaluate growth variations, we determined the maximum growth rate (_gr_, the maximum slope of
EGFP expression) and the Area Under the Curve (AUC) of the EGFP expression from individual wells (Fig. 5A) infected with virus at 0.5 TCID50/well. Under this condition, approximately 20–30%
of wells were positive for viral infection, implying that most virus-positive wells began with a single infectious unit. We found that NHC-treated TC-83 virus population showed a
significant decrease in viral replication with a negative skewing with respect to _gr_ and AUC in the histogram analysis (Fig. 5B and C). For example, the growth rate and AUC of the NHC 10
µM-treated group was reduced by 20% compared to the mock group. Inversely, other time-associated kinetic parameters such as the lag time (the time intercept between the regression line
associated with the gr calculation and the baseline defined by the first point in the calculation zone, defined as ‘LagC’) and time at maximum growth rate (t_gr) were increased, indicating a
delayed replication of the NHC-treated populations compared to the mock-treated group (Supportive Fig. 2). At the individual level, however, approximately 44–55% of the single isolates from
NHC-conditioned virus exhibited growth rates similar to the untreated group (mean ± 1 x S.D.). These results demonstrate that even though NHC treatment did not result in an extinction of
virus within a single round of treatment, the minor replication-competent population produced from treatment with NHC has a negatively skewed, yet diversified growth rate. DISCUSSION RNA
mutagens have gained attention as an antiviral against a broad-spectrum of RNA viruses, including VEEV and coronaviruses21,24,26,31,32,33. The primary mechanism of RNA mutagens is understood
to induce mutations within RNA genome, resulting in overall fitness defects. In this study, we examined the genetic landscape of VEEV TC-83 after NHC treatment and evaluated its effects on
the fitness with a systematic approach. ANTIVIRAL AND MUTAGENIC ACTIVITY OF NHC AGAINST VEEV TC-83 Our results demonstrated NHC’s strong antiviral activity against VEEV through a reduction
of virus titer > 106-fold and a lower specific infectivity than the mock-treated group, which is consistent with findings by others21. In our study, however, we further sought to
understand the dynamics between NHC concentration and its mutagenic activity, particularly on the infectious virus population because this population can provide insight into how an increase
in the number mutations affects the overall fitness. Our study demonstrated that after 4 passages under 10 µM NHC treatment the VEEV TC-83 population experienced a population crash, which
supports the overall concept of the RNA mutagen as an antiviral that has not been previously shown. NHC induced mutations in the viral genome in a concentration-dependent manner at the total
virus level within the tested range (Fig. 3B). In our study, the mock-treated group (DMSO-treated) showed a mutation-frequency of 1.30 × 10−4 s/n (_n_ = 3), which is consistent with what
others have reported for alphaviruses34, and the NHC-treated group showed a significantly increased mutation frequency in their progeny virus population. However, we found that the degree by
which mutations increased did not correlate with anti-viral activity at higher concentrations. The lethal mutagenesis effect of NHC was saturated between 10 and 20 µM, indicating no further
benefit in inhibiting viral replication beyond these concentrations. MUTATION FREQUENCY THRESHOLD FOR THE VIABLE VIRUS POPULATION While the total population sequencing showed a continuous
increase in mutation frequency as a function of NHC concentration, we observed two interesting outcomes from the replication-competent minor populations. First, a single round treatment of
NHC did not result in the complete extinction of the population even in the presence of higher NHC concentrations, indicating that multiple rounds of NHC incorporation are necessary (Fig. 2B
and C). Secondly, the mutation frequency of the replication-competent viruses did not surpass 6.3 × 10−4 s/n, roughly 6.5 mutations per genome, with NHC treatment of 10µM or higher. This
strongly suggests that VEEV cannot withstand a mutation frequency higher than an average of 6.5 mutations per genome, which is a 4-fold increase compared to the 1.4 mutations per genome
observed in the untreated population in the cell culture model. The mutational threshold in natural environments remains to be determined. SINGLE MOLECULAR SEQUENCING FOR VIRAL MUTAGENESIS
STUDY We employed a single molecular sequencing approach (i.e., SMRT sequencing also known as PacBio sequencing) of a 5.9 kb amplicon (~ 50% of the VEEV genome) instead of the conventional
Next-Generation sequencing of small fragments. As the single molecular sequencing can provide sequences in phase35,36,37, we believe this approach may be more appropriate for the
reconstruction of genomes sequences to understand the mutagen-induced mutations. The power of our approach was highlighted by finding that 12.5% of the replication-competent population
showed no mutations within the amplicon (approximately 50% of the total genome, Table 1), which otherwise would not be able to be identified. MUTATIONAL FITNESS EFFECTS Our work further
demonstrates the mutational fitness effects (MFE) at the level of individual viruses that were generated with increased mutation rates. In general, mutations are perceived to negatively
affect viral replication38,39. In our study we sought to determine the precise relationship between accumulation of mutations and virus growth profile as the concentration of NHC is
increased. By utilizing EGFP expression as a surrogate marker for viral replication in infected cells27, we were able to analyze the growth profile of viruses in a real-time, high-throughput
manner40. Our approach clearly displayed viral growth defects with an increase in lagC and a decrease in gr and AUC by approximately 20% for NHC-treated population compared to the untreated
population (Fig. 5B, and C). Considering that the mutation frequencies of these groups were ~ 20-fold higher than the untreated group (6.3 × 10−4 vs. 0.18–0.3 × 10−4 s/n, respectively), the
growth was considerably less prominent than expected. More interestingly, a significant number of viral isolates within the NHC-treated group displayed a growth profile equivalent to the
mock treated group (Fig. 5B and C). This finding agrees with our mutational analyses, showing ≥ 30% of mutation-free populations within the nsP2-4 amplicon (Fig. 4A). However, this
observation could be explained as viral clones within a population that are not equally affected by mutagen treatment could be deemed as ‘survivors’ from the treatment. We believe that these
replication-competent viruses with a negatively skewed distribution of fitness serve as founders for the next round of replication, eventually reaching the maximum tolerable mutation
frequency, (i.e., 6.3 × 10−4 s/n) during successive passages. Our result is largely consistent with a recent study on the effect of NHC on La Crosse virus in vivo demonstrating various
smaller sizes of plaques after NHC treatment41. Together we showed that serial NHC treatment effectively resulted in an extinction of replication-competent population of VEEV. Within a
single replication cycle, NHC induced concentration-dependent, transition mutations during the synthesis of genomic RNA of VEEV TC-83 at random locations, leaving the overall population with
a more diverse genetic landscape. While the majority of the diversified population became non-replicable, we also found that NHC treatment during a single passage was not able to induce a
complete inhibition, leaving a minor replication-competent VEEV RNA virus population with a diversified, yet negatively skewed fitness. Our study provides a detailed insight into the
dynamics between an expanded genetic landscape and antiviral activity induced by NHC. METHOD AND MATERIALS CELL CULTURE AND VIRAL STRAINS BHK-21 clone 13 (ATCC CCL-10) and Vero 76 (ATCC®
CRL-1587™) were maintained in Modified Eagle’s Medium with Earle’s Balanced Salt Solution and L-glutamine (MEM-E) supplemented with 10% fetal bovine serum (FBS) (Corning CellGro). Cells were
maintained at 37 ℃ in humidified incubators with 5% CO2. VEEV TC-83 was derived from a lyophilized vaccine stock (USAMRIID, gift from Dr. Connie Schmaljohn). Reconstituted virus underwent a
single round of replication in BHK-21 clone 13, prior to storage at -80 ℃ until use. VEEV TC-83 with dual reporters (rVEEV TC83-dR) were constructed with a plasmid backbone of pTC83-eGFP
(gift from Dr. Kevin Sokoloski). In this construct, the entire cDNA of the TC-8327 genome is under an SP6 promoter and eGFP is controlled under the double subgenomic promoter. The NanoLuc
luciferase gene was inserted at FseI site using the Gibson cloning method (pTC83-dR). Specific mutant viruses were generated using Quick-change mutagenesis with the pTC83-dR template (See
Supportive Method 1 for the primer sequences). The full sequence of the resultant clone was validated prior to rescuing the virus. Virus rescue was performed as described previously42.
ANTIVIRAL ASSAYS Anti-VEEV activity of NHC (Cayman Chemical) was measured using a cell-based CPE assay previously described29. Compounds were dissolved in DMSO at 20 mM and stored at -20 ℃.
Briefly, Vero 76 cells seeded in a 96 well plate one day prior were infected with virus at an MOI of 0.05 in the presence of test compounds, which were serially diluted to 8 different
concentrations. The final concentration of DMSO was maintained at 0.25%. Infected cells were incubated for 48 h (hrs) prior to measuring cell viability with CellTiter-Glo (Promega) to assess
protection from VEEV-induced CPE. For phenotypic resistance, the EC50s of ML336 (Cayman Chemical), an anti-VEEV direct acting antiviral compound inhibiting viral RNA synthesis30, against
various strains were determined by using EGFP fluorescence signal (RFU) expressed from infected cells as a surrogate readout for virus replication. Vero 76 cells plated on solid black
96-well plates were treated with serially diluted ML336 as above and then infected with mutant rVEEV TC83-dR strains at an MOI of 0.05. Following a 24-hour incubation at 37 ℃ with 5% CO2,
cell culture media was replaced with 70 µL of PBS, followed by EGFP signal detection measured with the Synergy 4 (BioTek). EC50s were calculated with a 4-parameter logistic model using XLfit
software (IBDS). GENERATION OF NHC-TREATED VEEV TC-83 STOCKS Vero 76 cells grown in T-25 flasks or 6-well plates were infected by incubating the cells with TC-83 at MOI of 1 for one hour at
37 ℃. The cells were washed with PBS twice and replenished with virus growth media containing NHC. After 24 h of incubation, the cell supernatant was collected and centrifuged to remove the
cell debris. Virus was aliquoted and stored at -80 ℃ until needed. SERIAL PASSAGING OF NHC-TREATED VEEV TC-83 For the initial passage, Vero 76 cells grown in 6-well plates were infected by
incubating the cells with TC-83 at MOI of 0.2 for one hour at 37 ℃. The cells were washed with PBS twice and replenished with virus growth media containing either NHC, Brequinar, or DMSO.
The cell supernatant was harvested as before, and cells were resuspended in 1mL TRI reagent (Zymo) and stored at -80 ℃. For subsequent passages, 0.125mL from the previous passage was used to
blindly inoculate the next round of infection. The remainder of the infection followed the procedure described previously. CLONAL ISOLATION BY LIMITING DILUTION Vero cells were seeded in
384-wells at a density of 4000 cells/well in a volume of 15 µL and cultured overnight. Cells were infected with 0.1 pfu/well for normal population studies. Three days later wells with
productive infection were identified by evaluating CPE using alamarBlue (BioRad). Cell supernatants of wells in which alamarBlue fluorescence signal was less than 4×standard deviation (sdev)
of signal from uninfected cell controls were consolidated with a unique ID and then the virus clones were amplified once by infecting 96-well plates seeded with fresh Vero 76 cells for 18
h. BULK SEQUENCING RNA was isolated from infected cell supernatants with DirectRNAZol MagBead RNA (Zymo research). RNA was reverse transcribed to cDNA with Maxima reverse transcriptase
primed using random hexamers and following the manufacturer’s protocol. Total RNA isolated from 0.15 mL progeny virus was subjected to cDNA synthesis followed by targeted amplification of a
fragment containing nsP2-nsP3-nsP4 (5.9 kb) with Phusion High-Fidelity DNA polymerase and 9nt unique barcoded primers. The barcode sequences were generated by using an R package, DNA barcode
(https://bioconductor.org/packages/release/bioc/vignettes/DNABarcodes/inst/doc/DNABarcodes.html) using an argument of mySeqlevSet <- create.dnabarcodes(9, metric="seqlev”,
heuristic="ashlock”, cores = 12). A total of 612 barcodes sequences were obtained and unique sequences were added to the 5′ end of the sequences for nsP2-fwd and nsP4 rev. Barcoded
primers were purchased from IDT DNA. The primer sequences are listed in Supplementary data (Sequences of the barcoded_primers.xlsx). PCR amplicons were purified with KAPA Pure magnetic beads
(Roche) at a 0.5 X bead-to-sample volume ratio and eluted in nuclease-free water. Pooled barcoded PCR amplicons were prepared into SMRTbell template libraries as recommended by the
manufacturer and subjected to single molecule, real time (SMRT) sequencing on the Sequel IIe system (Pacific Biosciences) using v2.0 chemistry and 30 h movies. Following data collection,
highly accurate (Q43, > 99.99%) circular consensus sequences (“HiFi reads”) were generated on the system. These HiFi data were used for all downstream analyses. HiFi read sequences were
de-multiplexed by known barcode sequences and mutational analyses performed. To generate the consensus sequence of the seeding population, RNA isolated from a culture infected with 100 pfu
of virus was used. SINGLE INFECTIOUS UNIT SEQUENCING USING NANOPORE SEQUENCING RNA was isolated from each well of infected cells cultured in a 96-well plate. Following cDNA synthesis, a 5.9
kb amplicon, encoding the nsP2-nsP3-nsP4 regions, was generated by PCR for each sample using 9nt-barcoded nsP2-forward and nsP4-reverse primers described above (See Supplementary data,
Sequences of the barcoded_primers.xlsx). Following amplicon generation, 2 µL from each PCR reaction were pooled together, purified with KAPA Pure magnetic beads (Roche) at a 0.5 X
bead-to-sample volume ratio, and eluted in nuclease-free water. From the purified PCR sample, 1 µg was used as input into the Nanopore ligation sequencing library preparation kit for
amplicons (Oxford Nanopore Technologies). If more than one 96-well plate worth of samples was to be sequenced together then the library preparation was done in conjunction with Nanopore
native barcoding of each 96-well plate sample pool (Oxford Nanopore Technologies). Each sequencing run was performed using a MinION Mk1c sequencer with R9.4.1 flow cell for 6 h with high
accuracy basecalling following the sequencing run. After obtaining the raw fastq files, read quality check was performed using Fastqc. Read length distribution was examined to confirm the
majority of reads fully cover the 5.9 kb amplicon. Sequencing data were de-multiplexed depending on the barcode sequences used for samples (see Supportive information, Sequences of the
barcoded_primers.xlsx) with an in-house script using 9-nt long barcode sequence plus 10-nt long primer sequence for the de-multiplexing process. SEQUENCE ANALYSIS WITH BIOINFORMATICS Each
demultiplexed sample fastq file was aligned to the reference genome sequence (VEEV GenBank: L01443.1) using Minimap243, which is efficient for aligning long sequencing reads. To identify
mutated sequences, we used mpileup from samtools (now bcftools)44. From each mapped bam file, the reference and alternative nucleotide sequences for each position of the target region were
counted and saved in VCF format. The alternate allele frequency is used as the mutation frequency. The significance of the identified mutations was assessed with the Fisher’s exact test to
calculate the p-value and Benjamini–Hochberg procedure to get false discovery rate (FDR). Occurrences of reference sequences and alternate sequences at each position of the target region
from the control samples were counted to set these values as the baseline sequencing error frequency. Similarly, these occurrences of reference and alternate sequences from the treated
samples were counted to set the observed allele frequency at each position. Using these values, we constructed a 2 × 2 table to compute p-value per each position. The FDR values were
complied with the Benjamini-Hochberg procedure with the p-values of all loci45. The overall mutation detection pipeline is depicted in Supportive Method Fig. 1. SINGLE INFECTION UNIT VIRAL
GROWTH KINETIC ASSAY Vero 76 cells were seeded in an imaging culture media (1X MEM-E with 2% FBS and 25 mM of HEPES without phenol red) in a 384-well plate at 5,000 cells/well and cultured
overnight in a CO2 incubator. The cell plate was infected with virus at approximately 0.5 TCID50/well and incubated at 37 ℃ in the Cytation 5 (BioTek) supplemented with 5% CO2. The amount of
virus per well was validated by a back titration of the diluted samples. The expression of EGFP was monitored every 20 min for 72 hrs. The growth analysis was performed using the fit
function of AMiGA program46 with additional arguments of ‘ --interval 1200 --do-not-log-transform -sfn 30’. Kinetic parameters were calculated with EGFP readouts (RFU) and the data were
normalized based on the control group with the normalize function of AMiGA with an argument of --normalize-by. Wells at the two outermost positions (i.e., columns of 1,2,23, and 24, and rows
of A, B, O, and P) were omitted for analysis for potential edge effects. Wells with the maximum growth rate (gr) > 200/hr and k-error threshold < 20% were defined as positive in viral
replication and selected for further analyses. VIRAL GROWTH KINETIC ASSAY OF MUTANT VIRUS Vero 76 cells were seeded in a virus culture media (1X MEM-E with 2% FBS and 25 mM of HEPES) in a
96-well plate at 24,000 cells/well and cultured overnight in a CO2 incubator. The cell plate was infected with virus at MOI of 10 or 0.1 (_n_ = 8) in a volume of 25 µL. After a 1-hour
incubation at 37 ℃, 75 µL of culture media was added for each well and the expression of EGFP was monitored every 20 min for 28 h at 37 ℃ in Cytation 5 (BioTek) provided with 5% CO2. The
growth analysis was performed as described above with the AMiGA program46. DATA AVAILABILITY Sequence data that support the findings of this study have been deposited in the NCBI GEO site
with an GEO accession ID of GSE207136 (https://www.ncbi.nlm.nih.gov/geo/query/acc.cgi? acc=GSE207136)Token: kzmtoseqnveplof. REFERENCES * Graci, J. D. & Cameron, C. E. Therapeutically
targeting RNA viruses via lethal mutagenesis. _Future Virol._ 3, 553–566 (2008). Article CAS PubMed PubMed Central Google Scholar * Perales, C. et al. The increasing impact of lethal
mutagenesis of viruses. _Future Med. Chem._ 11, 1645–1657 (2019). Article CAS PubMed Google Scholar * Perales, C. & Domingo, E. Antiviral strategies based on lethal mutagenesis and
error threshold. In _Quasispecies: from Theory to Experimental Systems_ vol. 392 (eds Domingo, E. & Schuster, P.) 323–339 (Springer International Publishing, Cham, 2015). * Crotty, S.,
Cameron, C. E. & Andino, R. RNA virus error catastrophe: Direct molecular test by using ribavirin. _Proc. Natl. Acad. Sci._ 98, 6895–6900 (2001). * Chung, D. H. et al. Ribavirin reveals
a lethal threshold of allowable mutation frequency for Hantaan virus. _J. Virol._ 81, 11722–11729 (2007). Article CAS PubMed PubMed Central Google Scholar * Chung, D. H. et al. The
murine model for Hantaan virus-induced lethal disease shows two distinct paths in viral evolutionary trajectory with and without Ribavirin treatment. _J. Virol._ 10997–11007.
https://doi.org/10.1128/JVI.01394-13 (2013). * Jordan, I., Briese, T., Fischer, N., Lau, J. Y. N. & Lipkin, W. I. Ribavirin inhibits west nile virus replication and cytopathic effect in
neural cells. _J. Infect. Dis._ 182, 1214–1217 (2000). Article CAS PubMed Google Scholar * Furuta, Y., Komeno, T. & Nakamura, T. Favipiravir (T-705), a broad spectrum inhibitor of
viral RNA polymerase. _Proc. Jpn. Acad. Ser. B: Phys. Biol. Sci._ 93, 449–463 (2017). Article ADS CAS PubMed Google Scholar * Baranovich, T. et al. T-705 (favipiravir) induces lethal
mutagenesis in influenza A H1N1 viruses in vitro. _J. Virol._ 87, 3741–3751 (2013). Article CAS PubMed PubMed Central Google Scholar * Day, C. W. et al. Error-prone replication of West
Nile virus caused by Ribavirin. _Antiviral Res._ 67, 38–45 (2005). Article CAS PubMed Google Scholar * Loeb, L. A. et al. Lethal mutagenesis of HIV with mutagenic nucleoside analogs.
_Proc. Natl. Acad. Sci. U S A_. 96, 1492–1497 (1999). Article ADS CAS PubMed PubMed Central Google Scholar * Pariente, N., Airaksinen, A. & Domingo, E. Mutagenesis versus
inhibition in the efficiency of extinction of Foot-and-Mouth Disease Virus. _J. Virol._ 77, 7131–7138 (2003). Article CAS PubMed PubMed Central Google Scholar * Ruiz-Jarabo, C. M., Ly,
C., Domingo, E. & de Torre, J. C. la. Lethal mutagenesis of the prototypic arenavirus lymphocytic choriomeningitis virus (LCMV). _Virology_ 308, 37–47 (2003). * Heck, J. A., Lam, A. M.
I., Narayanan, N. & Frick, D. N. Effects of mutagenic and chain-terminating nucleotide analogs on enzymes isolated from hepatitis C virus strains of various genotypes. _Antimicrob.
Agents Chemother._ 52, 1901–1911 (2008). Article CAS PubMed PubMed Central Google Scholar * Contreras, A. M. et al. Viral RNA mutations are region specific and increased by Ribavirin in
a full-length hepatitis C virus replication system. _J. Virol._ 76, 8505–8517 (2002). Article CAS PubMed PubMed Central Google Scholar * Delang, L. et al. Mutations in the Chikungunya
virus non-structural proteins cause resistance to favipiravir (T-705), a broad-spectrum antiviral. _J. Antimicrob. Chemother._ 69, 2770–2784 (2014). Article CAS PubMed Google Scholar *
Julander, J. G., Smee, D. F., Morrey, J. D. & Furuta, Y. Effect of T-705 treatment on western equine encephalitis in a mouse model. _Antiviral Res._ 82, 169–171 (2009). Article CAS
PubMed PubMed Central Google Scholar * Rabah, N. et al. Mutations on VEEV nsP1 relate RNA capping efficiency to Ribavirin susceptibility. _Antiviral Res._ 182, 104883 (2020). Article
PubMed Google Scholar * Beaucourt, S. & Vignuzzi, M. Ribavirin: a drug active against many viruses with multiple effects on virus replication and propagation. Molecular basis of
Ribavirin resistance. _Curr. Opin. Virol._ 8, 10–15 (2014). Article CAS PubMed PubMed Central Google Scholar * Bougie, I. & Bisaillon, M. The Broad Spectrum Antiviral Nucleoside
Ribavirin as a substrate for a viral RNA capping enzyme. _J. Biol. Chem._ 279, 22124–22130 (2004). Article CAS PubMed Google Scholar * Urakova, N. et al. β-D- _N_4 -Hydroxycytidine is a
potent anti-alphavirus compound that induces a high level of mutations in the viral genome. _J. Virol._ 92, e01965–e01917 (2017). /jvi/92/3/e01965-17.atom * Malone, B. & Campbell, E. A.
Molnupiravir: coding for catastrophe. _Nat. Struct. Mol. Biol._ 28, 706–708 (2021). Article PubMed Google Scholar * Kabinger, F. et al. Mechanism of molnupiravir-induced SARS-CoV-2
mutagenesis. _Nat. Struct. Mol. Biol._ 28, 740–746 (2021). Article CAS PubMed PubMed Central Google Scholar * Sheahan, T. P. et al. An orally bioavailable broad-spectrum antiviral
inhibits SARS-CoV-2 in human airway epithelial cell cultures and multiple coronaviruses in mice. _Sci. Transl Med._ 12, eabb5883 (2020). Article CAS PubMed Google Scholar * Zhou, S. et
al. β- d - _N_ 4-hydroxycytidine inhibits SARS-CoV-2 through Lethal Mutagenesis but is also mutagenic to mammalian cells. _J. Infect. Dis._ 224, 415–419 (2021). Article CAS PubMed PubMed
Central Google Scholar * Yoon, J. J. et al. Orally efficacious broad-spectrum Ribonucleoside Analog inhibitor of Influenza and respiratory syncytial viruses. _Antimicrob. Agents
Chemother._ 62, e00766–e00718 (2018). Article CAS PubMed PubMed Central Google Scholar * Sun, C. et al. High-level expression of reporter proteins from Improved Alphavirus expression
vectors to track replication and dissemination during Encephalitic and Arthritogenic Disease. _J. Virol._ 88, 2035–2046 (2014). Article PubMed PubMed Central Google Scholar * Markland,
W., McQuaid, T. J., Jain, J. & Kwong, A. D. Broad-spectrum antiviral activity of the IMP dehydrogenase inhibitor VX-497: a comparison with Ribavirin and demonstration of antiviral
additivity with alpha interferon. _Antimicrob. Agents Chemother._ 44, 859–866 (2000). Article CAS PubMed PubMed Central Google Scholar * Chung, D. H. et al. Discovery of a
broad-spectrum antiviral compound that inhibits pyrimidine biosynthesis and establishes a type 1 Interferon-Independent Antiviral State. _Antimicrob. Agents Chemother._ 60, 4552–4562 (2016).
Article CAS PubMed PubMed Central Google Scholar * Skidmore, A. M., Adcock, R. S., Jonsson, C. B., Golden, J. E. & Chung, D.-H. Benzamidine ML336 inhibits plus and minus strand RNA
synthesis of Venezuelan equine encephalitis virus without affecting host RNA production. _Antivir. Res._ 104674. https://doi.org/10.1016/j.antiviral.2019.104674 (2019). * Agostini, M. L. et
al. Small-molecule antiviral β- d - _N_4 -Hydroxycytidine inhibits a proofreading-intact coronavirus with a high genetic barrier to resistance. _J. Virol._ 93, e01348–e01319 (2019). Article
CAS PubMed PubMed Central Google Scholar * FischerII, W. A. et al. A phase 2a clinical trial of Molnupiravir in patients with COVID-19 shows accelerated SARS-CoV-2 RNA clearance and
elimination of infectious virus. _Sci. Transl. Med._ https://doi.org/10.1126/scitranslmed.abl7430 (2021). * Stuyver, L. J. et al. Ribonucleoside Analogue that blocks replication of Bovine
Viral Diarrhea and Hepatitis C Viruses in Culture. _Antimicrob. Agents Chemother._ 47, 244–254 (2003). Article CAS PubMed PubMed Central Google Scholar * Coffey, L. L., Beeharry, Y.,
Bordería, A. V., Blanc, H. & Vignuzzi, M. Arbovirus high fidelity variant loses fitness in mosquitoes and mice. _Proc. Natl. Acad. Sci. U S A_. 108, 16038–16043 (2011). Article ADS CAS
PubMed PubMed Central Google Scholar * Pollard, M. O., Gurdasani, D., Mentzer, A. J., Porter, T. & Sandhu, M. S. Long reads: their purpose and place. _Hum. Mol. Genet._ 27,
R234–R241 (2018). Article CAS PubMed PubMed Central Google Scholar * Burgess, D. J. Next regeneration sequencing for reference genomes. _Nat. Rev. Genet._ 19, 125–125 (2018). Article
CAS PubMed Google Scholar * Amarasinghe, S. L. et al. Opportunities and challenges in long-read sequencing data analysis. _Genome Biol._ 21, 30 (2020). Article PubMed PubMed Central
Google Scholar * Sanjuán, R. Mutational fitness effects in RNA and single-stranded DNA viruses: common patterns revealed by site-directed mutagenesis studies. _Phil Trans. R Soc. B_. 365,
1975–1982 (2010). Article PubMed PubMed Central Google Scholar * Domingo-Calap, P., Cuevas, J. M. & Sanjuán, R. The Fitness effects of Random mutations in single-stranded DNA and RNA
bacteriophages. _PLoS Genet._ 5, e1000742 (2009). Article PubMed PubMed Central Google Scholar * Danhier, P. et al. Combining Optical Reporter proteins with different half-lives to
detect temporal evolution of Hypoxia and Reoxygenation in Tumors. _Neoplasia_. 17, 871–881 (2015). Article CAS PubMed PubMed Central Google Scholar * Ojha, D. et al. _N_4
-Hydroxycytidine/Molnupiravir Inhibits RNA-Virus Induced Encephalitis by Producing Mutated Viruses with Reduced Fitness. Preprint at (2023). https://doi.org/10.1101/2023.08.22.554316 *
Bernard, K. A., Klimstra, W. B. & Johnston, R. E. Mutations in the E2 glycoprotein of Venezuelan equine Encephalitis Virus Confer Heparan Sulfate Interaction, Low Morbidity, and Rapid
Clearance from blood of mice. _Virology_ 276, 93–103 (2000). Article CAS PubMed Google Scholar * Li, H. Minimap2: pairwise alignment for nucleotide sequences. _Bioinformatics_. 34,
3094–3100 (2018). Article CAS PubMed PubMed Central Google Scholar * Li, H. et al. The sequence Alignment/Map format and SAMtools. _Bioinformatics_. 25, 2078–2079 (2009). Article
PubMed PubMed Central Google Scholar * Benjamini, Y. & Hochberg, Y. Controlling the false Discovery rate: a practical and powerful Approach to multiple testing. _J. Royal Stat. Soc.
Ser. B (Methodological)_. 57, 289–300 (1995). Article MathSciNet Google Scholar * Midani, F. S., Collins, J. & Britton, R. A. AMiGA: Software for automated analysis of microbial
growth assays. _mSystems_ 6, e00508-21 (2021). Download references ACKNOWLEDGEMENTS We thank Firas Midani for helping with the growth analysis using AMiGA. The present work has benefited
from University of Louisville Sequencing Technology Center. FUNDING This work was supported by National Health Institutes funding 1U19AI142762 (NIAID) to D.C., P20GM103436 (NIGMS) to J.P.,
and P30ES030283 (NIEHS) to J.P. and by institutional support from the University of Louisville to D.C. The funders had no role in study design, data collection and analysis, decision to
publish or preparation of the manuscript. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Center for Predictive Medicine, University of Louisville, Louisville, KY, USA Brian Alejandro, Eun
Jung Kim & Donghoon Chung * Department of Microbiology and Immunology, School of Medicine, University of Louisville, Louisville, KY, USA Donghoon Chung * Department of Medicine,
University of Louisville, Louisville, KY, USA Jae Yeon Hwang & Juw Won Park * Brown Cancer Center Bioinformatics Core, University of Louisville, Louisville, KY, USA Jae Yeon Hwang &
Juw Won Park * Department of Biochemistry and Molecular Genetics, School of Medicine, University of Louisville, Louisville, KY, USA Melissa Smith Authors * Brian Alejandro View author
publications You can also search for this author inPubMed Google Scholar * Eun Jung Kim View author publications You can also search for this author inPubMed Google Scholar * Jae Yeon Hwang
View author publications You can also search for this author inPubMed Google Scholar * Juw Won Park View author publications You can also search for this author inPubMed Google Scholar *
Melissa Smith View author publications You can also search for this author inPubMed Google Scholar * Donghoon Chung View author publications You can also search for this author inPubMed
Google Scholar CONTRIBUTIONS B.A., and D.C wrote the main manuscript text and figures. B.A., E.K., and D.C. conducted experiments for Figures 1, 2, 3, 4 and 5. J.H., J.W., and M.S.,
contributed to analysis for Figures 3 and 4. D.C. conceived the idea. All authors reviewed the manuscript. CORRESPONDING AUTHOR Correspondence to Donghoon Chung. ETHICS DECLARATIONS
COMPETING INTERESTS The authors declare no competing interests. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps
and institutional affiliations. SUPPLEMENTARY INFORMATION Below is the link to the electronic supplementary material. SUPPLEMENTARY MATERIAL 1 SUPPLEMENTARY MATERIAL 2 RIGHTS AND
PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing,
distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and
indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third
party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the
article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright
holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Alejandro, B., Kim, E.J.,
Hwang, J.Y. _et al._ Genetic and phenotypic changes to Venezuelan equine encephalitis virus following treatment with β-D-N4-hydroxycytidine, an RNA mutagen. _Sci Rep_ 14, 25265 (2024).
https://doi.org/10.1038/s41598-024-76788-x Download citation * Received: 27 August 2024 * Accepted: 16 October 2024 * Published: 25 October 2024 * DOI:
https://doi.org/10.1038/s41598-024-76788-x SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative