Play all audios:
ABSTRACT Obesity is a significant public health challenge, yet the link between BMI and mortality in critical illness remains unclear. This study analyzed 19,311 patients from the MIMIC-III
database, categorized into underweight, normal weight, overweight, and obese groups. Using Cox models and restricted cubic splines, we explored the complex association between BMI and
mortality. Finally, multiple sensitivity analyses were performed to test the robustness of the results. The proportion of underweight patients (2.3%) was the lowest, while overweight (34.8%)
and obese (34.5%) patients constituted a large proportion. Being underweight portended a greater risk, while being overweight or obese was associated with a lower risk of mortality, which
is consistent with the sensitivity analysis. Moreover, we observed a typical L-shaped association between BMI and the risk of mortality with and without adjustment, with the lowest mortality
occurring at approximately 32 kg/m2. The overall pattern of the nonlinear association between BMI and mortality was similar for most subgroup analyses. Underweight was associated with a
greater risk of mortality, while obesity and overweight were both associated with a lower risk of mortality in critically ill patients. BMI had a typical L-shaped association with the risk
of mortality. SIMILAR CONTENT BEING VIEWED BY OTHERS EVALUATING THE OBESITY PARADOX IN PATIENTS WITH SEPSIS AND CANCER Article Open access 12 May 2025 THE OBESITY PARADOX IN YOUNGER ADULT
PATIENTS WITH SEPSIS: ANALYSIS OF THE MIMIC-IV DATABASE Article 26 April 2024 ASSOCIATION BETWEEN LOW BODY MASS INDEX AND INCREASED 28-DAY MORTALITY OF SEVERE SEPSIS IN JAPANESE COHORTS
Article Open access 15 January 2021 INTRODUCTION According to a report published by the World Health Organization (WHO), excess or abnormal fat accumulation has emerged as a rapidly growing
threat to the health of humans in an increasing number of countries. The latest data show that a high body mass index (BMI) caused approximately 4 million deaths globally in 20151. Many
health problems, such as sleep apnea, type 2 diabetes, hypertension, cardiovascular diseases, dyslipidemia, and physical disabilities, are a direct consequence of increased fat mass.
Moreover, the number of obese adults continues to increase from 100 million in 1975 to 671 million in 2016 and is projected to increase to 1.12 billion by 20302,3. BMI [weight (kg)/height2
(m)], which forms the basis for the WHO classification, is commonly used to estimate the amount of body fat. Multiple large observational studies have suggested that BMI is closely related
to all-cause mortality, and those studies revealed a U-shaped association with minimum mortality in the range from 20 to 25 kg/m24,5,6,7. Increasing evidence suggests that patients with
similar BMIs may have different obesity-related complications depending on the distribution of excess fat, including visceral and ectopic versus subcutaneous fat8,9. The phenomenon that
obesity is a risk factor for mortality in the general population but a protective factor for mortality in patients with chronic diseases, such as chronic kidney disease, heart failure,
cancer, and diabetes mellitus, is called the “obesity paradox”, which indicates a more complex and variable association between BMI and mortality10,11,12. In addition, BMI is a poor marker
of excess body fat in patients with either increased or low muscle mass. As the prevalence of obesity continues to increase, it has become one of the greatest health issues affecting all age
groups and is also prevalent in the intensive care unit (ICU) population13,14. Some studies have shown that BMI may be associated with morbidity13 and increased resource utilization15, but
the impact of obesity on ICU mortality is still debated. In this study, we aimed to retrospectively examine the association between BMI and mortality in ICU patients using the MIMIC-III
database. The robustness of our primary outcome was tested by a series of sensitivity analyses. We performed a series of subgroup analyses, including age (≤ 60 and > 60), sex,
hypertension status, diabetes status, liver disease status, CHF status and ethnicity. Our study could help ICU physicians better understand the association between BMI and outcomes in ICU
patients, aiding in the management of this vulnerable population. METHODS This study aimed to evaluate the association between Body Mass Index (BMI) and mortality in critically ill patients.
We conducted a retrospective cohort study using data from the MIMIC-III v1.4 database, which includes detailed clinical information from the Beth Israel Deaconess Medical Center collected
between 2001 and 2012. We analyzed demographic information, comorbidities, severity scores, vital signs, laboratory results, and treatments. The primary outcomes were 28-day and 60-day
mortality rates. To assess the impact of BMI on these outcomes, we used Cox proportional hazard models and restricted cubic spline analysis, adjusting for potential confounders. Sensitivity
analyses were conducted across various subgroups to validate the robustness of our results. This methodological approach aimed to provide insights into how BMI affects mortality in
critically ill patients, aiding in risk stratification and clinical decision-making in the ICU setting. DATA SOURCES All data in our study were extracted from the MIMIC-III v 1.4, a large,
single-center, open and free critical care database that contains comprehensive clinical data of patients admitted to the Beth Israel Deaconess Medical Center in Boston, Massachusetts
between June 2001 and October 201216. The database was released on 2nd September 2016, in which comprehensive and deidentified in-hospital information, including vital signs, medications,
laboratory measurements, observations and notes charted by care providers, fluid balance, procedure codes, diagnostic codes, imaging reports, hospital length of stay, and survival data of
53,423 distinct ICU admissions, was stored. The final diagnosis was recorded according to the International Classification of Disease 9th Edition code when patients were discharged. Ethical
clearance and informed consent were not required because the MIMIC-III is an anonymized database that is available to the public. The STrengthening the Reporting of OBservational studies in
Epidemiology (STROBE) Statement was applied in the present study. STUDY COHORT We included all individuals with BMI data and excluded those who met the following criteria: (1) age < 18
years OR > 85 years; (2) length of stay < 24 h; (3) pregnancy; and (4) missing body weight or height data. In the case of more than one hospital admission, each patient contributed
only their first admission to the analysis. Altogether, 19,311 ICU patients were included in the present study. The World Health Organization Consultation published a report on obesity that
defined BMI-based categories of underweight, normal weight, preobesity, and obesity in 199717. The same cutoff BMI values were adopted by the National Heart, Lung, and Blood Institute in
199818. In this study, all participants were divided into four groups, namely, underweight (BMI < 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2), and obese
(BMI ≥ 30 kg/m2), based on the WHO categories. This study was conducted in accordance with the Helsinki Declaration (WMA Declaration of Helsinki, 2013). COVARIATES AND OUTCOMES We utilized
Structured Query Language to extract a large amount of clinical information for each enrolled patient from MIMIC-III, including (1) demographic data (age, sex, BMI and ethnicity); (2)
etiology at admission; (3) comorbidities (the Elixhauser Comorbidity Index, hypertension, cardiac arrhythmias, congestive heart failure, peptic ulcer, liver disease, diabetes, chronic
obstructive pulmonary disease, coagulopathy, and solid tumor); (4) severity scores, including the Sequential Organ Failure Assessment (SOFA) score and the Simplified Acute Physiology Score
(SAPS II)); (5) mean value of vital signs within 24 h after ICU admission (heart rate, respiratory rate, temperature, mean arterial pressure, pO2, pCO2 and pH); (6) the poorest laboratory
test value during the first day after ICU admission (white blood cell count), platelet count, hemoglobin, glucose, creatinine, chloride, sodium, potassium, blood urea nitrogen (BUN), base
excess, international normalized ratio (INR), prothrombin time (PT), partial thromboplastin time (PTT), and bicarbonate); and (7) the treatment received (mechanical ventilation; renal
replacement therapy). The primary outcomes of the study were 28-day mortality and 60-day mortality. Patient mortality information for discharged patients was gathered from the US Social
Security Death Index. Secondary outcomes included the number of days of mechanical ventilation, renal replacement therapy, and length of stay. STATISTICAL ANALYSIS The raw data were
extracted from the MIMIC-III database using SQL (structure query language) with Navicat Premium version 15.0.26. Further statistical analyses were performed with the statistical software R
v4.2.0. We first divided all patients into four groups according to BMI. We used the Shapiro‒Wilk test to check for normality, and normally distributed continuous variables are presented as
the mean ± standard deviation, nonnormally distributed continuous variables as the median (interquartile range), and categorical variables as frequencies (percentages). Continuous variables
were compared by ANOVA (analysis of variance), and categorical variables were compared by the chi-square test or Fisher’s exact test, with Bonferroni correction for multiple pairwise
comparisons. Then, we used two main methods to analyze the association between BMI and mortality in critically ill patients. First, five Cox proportional hazards regression models were used
to evaluate the independent associations of BMI with survival. Model 1 was adjusted for demographic variables (age and ethnicity). Model 2 was adjusted for variables included in model 1 plus
vital signs and arterial blood gas results (PCO2, pH, heart rate and temperature). Model 3 was adjusted for variables included in model 2 plus biochemical markers (glucose, hemoglobin, WBC,
platelet count, and creatinine). Model 4 was adjusted for all covariates except for severity scores (SOFA score and SAPS score). Model 5 was adjusted for all covariates. Second, to evaluate
the possible nonlinear impact of BMI as a continuous variable on survival, a multivariable Cox model with restricted cubic splines (RCSs) was built. Kaplan-Meier survival curves were
generated to compare survival rates among BMI groups. Log-rank tests were conducted to assess statistical differences between these survival curves. Finally, we conducted several sensitivity
analyses to test the robustness of our primary findings and how our conclusions can be affected in different situations. First, we used Cox proportional hazards models to determine the
impact of various subgroups on our findings. Second, we utilized restricted cubic spline analysis to examine the association between BMI and mortality risk within these subgroups. Missing
values were handled by multiple imputation methods based on the “Mice” package of R. However, these variables were omitted when more than 25% of the values were missing. A two-tailed P value
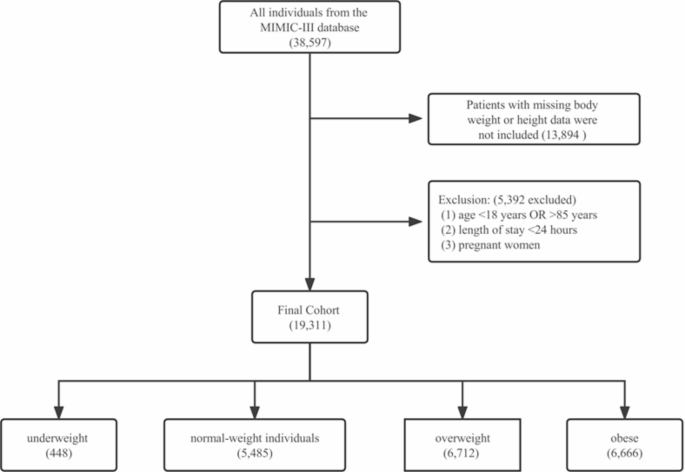
of < 0.05 was considered to indicate statistical significance. RESULTS BASELINE CHARACTERISTICS OF THE PARTICIPANTS Of the 38,597 individuals from the MIMIC-III database, 19,311 were
included in the study. The flow diagram of patient selection is presented in Fig. 1. Among them, 5,485 were normal-weight individuals, 448 were underweight individuals, 6,712 were overweight
individuals, and 6,666 were obese individuals (Table 1). More males than females were included in this study (male: 61.3%; female: 38.7%). Females (55.8%) composed the majority of the
underweight group, while males made up the majority of the other groups. A positive association was observed between glucose and BMI (median glucose of 123 mg/dl in underweight individuals,
125 mg/dl in normal-weight individuals, 128 mg/dl in overweight individuals, and 134 mg/dl in obese individuals), consistent with expected trends19. The greater the BMI is, the greater the
proportion of patients with hypertension. Normal-weight patients had the highest PO2 and pH. The lowest proportion of underweight patients had hypertension. A negative association was
observed between mortality and BMI as well as between the SAPS II score and BMI. No significant differences were observed in the mean blood pressure, PTT, INR, or prevalence of liver disease
or peptic ulcers among the different groups. ASSOCIATION BETWEEN BMI AND OUTCOMES We applied Cox proportional hazards models to evaluate the association between BMI and mortality in
critical patients. Univariate Cox regression analysis for the hazard ratio of survival indicated that a lower BMI was associated with a greater risk of 28-day mortality (underweight: HR,
1.44; overweight: HR, 0.75; obese: HR, 0.74) and 60-day mortality (underweight: HR, 1.56; overweight: HR, 0.74; obese: HR, 0.71). After further adjustment for a series of covariates in the
other four models, the association between BMI and mortality was largely consistent (Table 2). Patients with a higher BMI had a greater likelihood of receiving mechanical ventilation therapy
and RRT (Table 1). K‒M survival curves indicated that underweight patients had the worst survival among all groups, while obese patients and overweight patients had better survival than
normal-weight patients did (Fig. 2). The differences in survival curves were statistically significant, as determined by the log-rank test, with all p-values being < 0.001. NONLINEAR
ASSOCIATION BETWEEN BMI AND MORTALITY Restricted cubic spline models were used to visualize the shape of the association between BMI and outcomes in critical patients. With this analysis, we
observed a typical L-shaped association between BMI and the outcomes of critical patients with and without adjustment, with the lowest mortality occurring at approximately 32 kg/m2 (Fig.
3). The results from the cubic spline model suggested that critical patients had a marked increase in risk at low BMIs but only a minimal elevation in risk at higher BMIs. The nadir for both
28-day mortality and 60-day mortality risk among critically ill patients was estimated to be at a BMI of 32 kg/m2 from the RCS curve. Higher BMIs were likely protective factors for critical
patients compared with normal-weight patients under the influence of covariates (Fig. 4). SENSITIVITY ANALYSIS To further verify the robustness of the reported findings, sensitivity
analyses were conducted. Primary covariates of interest, which included age, sex, hypertension status, CHF status, liver disease status, diabetes status, and ethnicity, were included in the
sensitivity analyses. Compared with those of normal-weight patients, the risk of 28-day mortality and 60-day mortality was lower for both overweight and obese patients in the following
subgroups: those with hypertension, without diabetes, those with and without CHF, those with liver disease, those who were male, and those aged older than 60 years (Fig. 5). The overall
pattern of the nonlinear association between BMI and mortality was similar for most subgroup analyses (Fig. 6). All of the sensitivity analyses confirmed our main analyses. DISCUSSION In
this retrospective cohort study, 19,311 critically ill patients were included from the MIMIC-III database and then classified into four BMI-based categories: underweight, normal weight,
overweight, and obese. Notably, the proportion of underweight patients (2.3%) was the lowest, while overweight (34.8%) and obese (34.5%) patients constituted a much larger proportion of
critically ill patients. The prevalence of obesity in our study was much greater than that in recent reports, in which the proportion was approximately 20%14. A positive association was
observed between glucose and BMI as well as between the frequency of hypertension and BMI, which is consistent with previous studies20,21,22. Briefly, we found that underweight was
associated with a significantly greater risk for 28-day mortality and 60-day mortality, while overweight was associated with a lower risk for 28-day mortality and 60-day mortality than
normal weight in critically ill patients. Additionally, we observed a typical L-shaped association between BMI and mortality, with the lowest mortality occurring at approximately 32 kg/m2.
Moreover, patients with a higher BMI had a greater likelihood of receiving mechanical ventilation therapy and RRT. A large amount of research has shown that BMI has J-shaped associations
with overall mortality and most specific causes of death23. However, a small amount of research has estimated a lower risk among overweight patients than among normal-weight patients24. The
discrepant results between different studies might be explained by reverse causality and residual confounding. Most studies have shown clear heterogeneity in the associations between BMI and
different causes of death, which means that the association of all-cause mortality with BMI will be affected by cause-of-death distributions in the source population. Currently, the impact
of obesity on ICU mortality is still debated. Although obesity seems to be associated with morbidity, the association between the two is not yet clear13,14. Thus, this study provides
evidence for the possibility of using BMI to predict the prognosis of critically ill patients, highlighting the possibility of employing BMI as a novel, easily obtained risk marker. The
prevalence of obesity has tripled worldwide and has been increasing since 1975. It has become a nonnegligible health issue that affects all age groups, populations, and countries of all
income levels. Identifying the complex association between BMI and mortality is challenging. This challenge becomes increasingly difficult in complex, dynamic environments such as the ICU.
In general, innovations that have been found to be beneficial in specific disease populations may be applied to other populations in which those findings have not been adequately analyzed,
potentially exposing patients to harm without commensurate benefit25. Large cohort studies in the general population demonstrated that BMI had J-shaped associations with overall mortality
and most specific causes of death, except for mental and behavioral, neurological, and external causes, which means that a high BMI was associated with an elevated risk of mortality for most
patients23,26. More recent data in hospitalized patients or patients with chronic illnesses have shown that overweight and moderate obesity are associated with lower mortality than a normal
BMI or more severe obesity14,18. Such a scenario has been observed not only in multiple chronic diseases, such as heart failure27, end-stage kidney disease28 and coronary artery disease29
but also in acute conditions, such as pneumonia30, acute respiratory distress syndrome31, sepsis32 or critical illness in general33. In addition, increasing BMI was not associated with
increased mortality in patients with COVID-19 admitted to intensive care34. The phenomenon known as the “obesity paradox” is that obesity increases the risk of obesity-related disease but is
paradoxically associated with increased survival in patients with these conditions. Our results are derived from an analysis of a real-world database and provide additional evidence for
understanding the association between BMI and mortality in critically ill patients. Although a large number of studies have revealed the obesity survival paradox, the actual protective
effect of adipose tissue has been challenged. The reason might be that the protective effect of adipose tissue could be influenced by factors that are difficult to control. First, some young
and healthy obese patients may be admitted to the ICU at a low threshold to avoid complications, thereby leading to selection bias. Second, the obesity survival paradox may be affected by
therapeutic factors. Obese patients prefer to receive a lower weight-based dosage of fluids and vasopressors, which potentially reduces the side effects of these therapies35. Finally, there
are increasing criticisms of the use of BMI as a measure of obesity. In this study, we systematically analyzed the association between outcomes and BMI based on data from a large sample size
extracted from a real-world database. We employed a novel methodology to address continuous covariates and reverse causality and conducted a wide range of sensitivity analyses. However, our
research has several limitations. First, approximately 21.8% of individuals who were otherwise eligible were excluded, according to the exclusion criteria. This may induce selection bias,
which is difficult to avoid. Second, the lack of relevant information about therapy may limit the generalizability of these results. However, sensitivity analyses for subgroups with diabetes
or liver disease who might receive a nutritional approach reached similar conclusions. Third, the MIMIC-III population is predominantly white, so these findings may not be generalizable to
other populations. CONCLUSIONS Compared with normal weight, underweight was associated with a significantly greater risk of mortality, while obesity and overweight were both associated with
a significantly lower risk of mortality in critically ill patients. BMI had a typical L-shaped association with the risk of mortality, and a BMI above the normal range was associated with an
elevated risk of mechanical ventilation, RRT, and prolonged length of stay. Based on our results, we recommend BMI as an easily obtained prognostic marker for critically ill patients. More
research is needed to determine the optimal BMI and potential role in risk stratification to more precisely guide therapeutic decisions. DATA AVAILABILITY Both original data and any
secondary data presented in this study are available upon request from the corresponding author. REFERENCES * Collaborators, G. B. D. O. et al. Health effects of overweight and obesity in
195 countries over 25 years. _N. Engl. J. Med._ 377, 13–27. https://doi.org/10.1056/NEJMoa1614362 (2017). Article MATH Google Scholar * Kelly, T., Yang, W., Chen, C. S., Reynolds, K.
& He, J. Global burden of obesity in 2005 and projections to 2030. _Int. J. Obes. (Lond.)_. 32, 1431–1437. https://doi.org/10.1038/ijo.2008.102 (2008). Article CAS PubMed MATH Google
Scholar * Collaboration, N. C. D. R. F. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement
studies in 128.9 million children, adolescents, and adults. _Lancet_ 390, 2627–2642. https://doi.org/10.1016/S0140-6736(17)32129-3 (2017). Article MATH Google Scholar * Aune, D. et al.
BMI and all cause mortality: Systematic review and non-linear dose-response meta-analysis of 230 cohort studies with 3.74 million deaths among 30.3 million participants. _BMJ_ 353, i2156.
https://doi.org/10.1136/bmj.i2156 (2016). Article PubMed PubMed Central Google Scholar * de Berrington, A. et al. Body-mass index and mortality among 1.46 million white adults. _N Engl.
J. Med._ 363, 2211–2219. https://doi.org/10.1056/NEJMoa1000367 (2010). Article MATH Google Scholar * Global, B. M. I. M. C. et al. Body-mass index and all-cause mortality:
individual-participant-data meta-analysis of 239 prospective studies in four continents. _Lancet_ 388, 776–786. https://doi.org/10.1016/S0140-6736(16)30175-1 (2016). Article Google Scholar
* Prospective Studies, C. et al. Body-mass index and cause-specific mortality in 900 000 adults: Collaborative analyses of 57 prospective studies. _Lancet_ 373, 1083–1096.
https://doi.org/10.1016/S0140-6736(09)60318-4 (2009). Article MATH Google Scholar * Piche, M. E., Poirier, P., Lemieux, I. & Despres, J. P. Overview of epidemiology and contribution
of obesity and body fat distribution to cardiovascular disease: An update. _Prog Cardiovasc. Dis._ 61, 103–113. https://doi.org/10.1016/j.pcad.2018.06.004 (2018). Article PubMed MATH
Google Scholar * Neeland, I. J., Poirier, P. & Despres, J. P. Cardiovascular and metabolic heterogeneity of obesity: Clinical challenges and implications for management. _Circulation_
137, 1391–1406. https://doi.org/10.1161/CIRCULATIONAHA.117.029617 (2018). Article PubMed PubMed Central Google Scholar * Tsang, N. M. et al. Overweight and obesity predict better overall
survival rates in cancer patients with distant metastases. _Cancer Med._ 5, 665–675. https://doi.org/10.1002/cam4.634 (2016). Article PubMed PubMed Central MATH Google Scholar * Zhao,
Y. et al. Body mass index and risk of all-cause mortality with normoglycemia, impaired fasting glucose and prevalent diabetes: Results from the rural Chinese cohort study. _J. Epidemiol.
Community Health_. 72, 1052–1058. https://doi.org/10.1136/jech-2017-210277 (2018). Article PubMed MATH Google Scholar * Uretsky, S. et al. Obesity paradox in patients with hypertension
and coronary artery disease. _Am. J. Med._ 120, 863–870. https://doi.org/10.1016/j.amjmed.2007.05.011 (2007). Article PubMed MATH Google Scholar * Sakr, Y. et al. Being overweight is
associated with greater survival in ICU patients: Results from the intensive care over nations audit. _Crit. Care Med._ 43, 2623–2632. https://doi.org/10.1097/CCM.0000000000001310 (2015).
Article PubMed MATH Google Scholar * De Jong, A. et al. Medical versus surgical ICU obese patient outcome: A propensity-matched analysis to resolve clinical trial controversies. _Crit.
Care Med._ 46, e294–e301. https://doi.org/10.1097/CCM.0000000000002954 (2018). Article PubMed MATH Google Scholar * Rosvall, B. R. et al. Impact of obesity on intensive care unit
resource utilization after cardiac operations. _Ann. Thorac. Surg._ 104, 2009–2015. https://doi.org/10.1016/j.athoracsur.2017.05.047 (2017). Article PubMed MATH Google Scholar * Johnson,
A. E. et al. MIMIC-III, a freely accessible critical care database. _Sci. Data_. 3, 160035. https://doi.org/10.1038/sdata.2016.35 (2016). Article CAS PubMed PubMed Central Google
Scholar * Obesity: preventing and managing the global epidemic. Report of a WHO consultation. In _World Health Organ Tech Rep Ser_ 894, i-xii, 1–253 (2000). * Clinical guidelines on the
identification, evaluation, and treatment of overweight and obesity in adults. _WMJ_ 97 (24–25), 20–21 (1998). * Haddow, J. E. et al. Peripheral deiodinase activity, and plasma glucose:
Relationships between white women in the HAPO study. _J. Clin. Endocrinol. Metab._ 104, 2593–2600. https://doi.org/10.1210/jc.2018-02328 (2019). Maternal BMI. Article PubMed PubMed Central
MATH Google Scholar * You, Y. et al. Hypertension and physical activity in middle-aged and older adults in China. _Sci. Rep._ 8, 16098. https://doi.org/10.1038/s41598-018-34617-y (2018).
Article ADS CAS PubMed PubMed Central Google Scholar * Svensson, M. K. et al. The risk for diabetic nephropathy is low in young adults in a 17-year follow-up from the diabetes
incidence study in Sweden (DISS). Older age and higher BMI at diabetes onset can be important risk factors. _Diabetes Metab. Res. Rev._ 31, 138–146. https://doi.org/10.1002/dmrr.2574 (2015).
Article CAS PubMed MATH Google Scholar * Looker, H. C., Knowler, W. C. & Hanson, R. L. Changes in BMI and weight before and after the development of type 2 diabetes. _Diabetes
Care_. 24, 1917–1922. https://doi.org/10.2337/diacare.24.11.1917 (2001). Article CAS PubMed MATH Google Scholar * Bhaskaran, K., Dos-Santos-Silva, I., Leon, D. A., Douglas, I. J. &
Smeeth, L. Association of BMI with overall and cause-specific mortality: A population-based cohort study of 3.6 million adults in the UK. _Lancet Diabetes Endocrinol._ 6, 944–953.
https://doi.org/10.1016/S2213-8587(18)30288-2 (2018). Article PubMed PubMed Central Google Scholar * Davey Smith, G. et al. The association between BMI and mortality using offspring BMI
as an indicator of own BMI: Large intergenerational mortality study. _BMJ_ 339, b5043. https://doi.org/10.1136/bmj.b5043 (2009). Article PubMed PubMed Central Google Scholar * Moss, M.,
Good, V. S., Gozal, D., Kleinpell, R. & Sessler, C. N. An official critical care societies collaborative statement-burnout syndrome in critical care health-care professionals: A call for
action. _Chest_ 150, 17–26. https://doi.org/10.1016/j.chest.2016.02.649 (2016). Article PubMed Google Scholar * Heymsfield, S. B., Wadden, T. A. & Mechanisms pathophysiology, and
management of obesity. _N Engl. J. Med._ 376, 254–266. https://doi.org/10.1056/NEJMra1514009 (2017). Article CAS PubMed MATH Google Scholar * Sharma, A. et al. Meta-analysis of the
relation of body mass index to all-cause and cardiovascular mortality and hospitalization in patients with chronic heart failure. _Am. J. Cardiol._ 115, 1428–1434.
https://doi.org/10.1016/j.amjcard.2015.02.024 (2015). Article PubMed MATH Google Scholar * Naderi, N. et al. Obesity paradox in advanced kidney disease: From bedside to the bench. _Prog
Cardiovasc. Dis._ 61, 168–181. https://doi.org/10.1016/j.pcad.2018.07.001 (2018). Article MathSciNet PubMed PubMed Central MATH Google Scholar * Romero-Corral, A. et al. Association of
bodyweight with total mortality and with cardiovascular events in coronary artery disease: A systematic review of cohort studies. _Lancet_ 368, 666–678.
https://doi.org/10.1016/S0140-6736(06)69251-9 (2006). Article PubMed MATH Google Scholar * Nie, W. et al. Obesity survival paradox in pneumonia: A meta-analysis. _BMC Med._ 12, 61.
https://doi.org/10.1186/1741-7015-12-61 (2014). Article PubMed PubMed Central MATH Google Scholar * Ni, Y. N. et al. Can body mass index predict clinical outcomes for patients with
acute lung injury/acute respiratory distress syndrome? A meta-analysis. _Crit. Care_. 21, 36. https://doi.org/10.1186/s13054-017-1615-3 (2017). Article PubMed PubMed Central MATH Google
Scholar * Pepper, D. J. et al. Increased body mass index and adjusted mortality in ICU patients with sepsis or septic shock: A systematic review and meta-analysis. _Crit. Care_. 20, 181.
https://doi.org/10.1186/s13054-016-1360-z (2016). Article PubMed PubMed Central MATH Google Scholar * Hogue, C. W. Jr. et al. The impact of obesity on outcomes after critical illness: A
meta-analysis. _Intensive Care Med._ 35, 1152–1170. https://doi.org/10.1007/s00134-009-1424-5 (2009). Article PubMed MATH Google Scholar * Taylor, E. H. et al. Factors associated with
mortality in patients with COVID-19 admitted to intensive care: A systematic review and meta-analysis. _Anaesthesia_ 76, 1224–1232. https://doi.org/10.1111/anae.15532 (2021). Article CAS
PubMed PubMed Central MATH Google Scholar * Wacharasint, P., Boyd, J. H., Russell, J. A. & Walley, K. R. One size does not fit all in severe infection: Obesity alters outcome,
susceptibility, treatment, and inflammatory response. _Crit. Care_. 17, R122. https://doi.org/10.1186/cc12794 (2013). Article PubMed PubMed Central Google Scholar Download references
ACKNOWLEDGEMENTS This work was supported by the Innovative Research Team of High-Level Local University in Shanghai. We thank all patients and authors involved in this study. FUNDING This
research received no external funding. AUTHOR INFORMATION Author notes * Wenbo Yu, Weiwei Jiang, and Jihong Yuan contributed equally to this work. AUTHORS AND AFFILIATIONS * Department of
Emergency Medicine, PLA Marine Corps Hospital, No. 1 Xinyang Road, Chaozhou, 521021, China Wenbo Yu, Tao Fan & Huiyan Xiao * Department of Emergency and Critical Care Medicine,
Changzheng Hospital, Naval Medical University, No. 415 Fengyang Road, Shanghai, 200003, China Weiwei Jiang, Yan Zhu & Wenfang Li * Seventh People’s Hospital of Shanghai University of
Traditional Chinese Medicine, No. 358 Datong Road, Shanghai, 200137, China Jihong Yuan * Department of Critical Care Medicine, PLA 96603 Unit Hospital, No. 65 Huaidong Road, Huaihua, 418000,
China Lizhu Sun * Department of Neurosurgery, Minhang Hospital, Fudan University, No. 39 Xinling Road, Shanghai, 201100, China Shaoshuai Wu Authors * Wenbo Yu View author publications You
can also search for this author inPubMed Google Scholar * Weiwei Jiang View author publications You can also search for this author inPubMed Google Scholar * Jihong Yuan View author
publications You can also search for this author inPubMed Google Scholar * Tao Fan View author publications You can also search for this author inPubMed Google Scholar * Huiyan Xiao View
author publications You can also search for this author inPubMed Google Scholar * Lizhu Sun View author publications You can also search for this author inPubMed Google Scholar * Yan Zhu
View author publications You can also search for this author inPubMed Google Scholar * Wenfang Li View author publications You can also search for this author inPubMed Google Scholar *
Shaoshuai Wu View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS WY, WJ and JY were responsible for the methodology and writing of the
manuscript and contrib-uted equally. TF, HX and LS were responsible for medical information collection, data extraction and verification. YZ, WL and SW designed and guided this study. WY, WJ
and JY contributed equally and share first authorship. All authors read and approved the final manuscript. CORRESPONDING AUTHORS Correspondence to Yan Zhu, Wenfang Li or Shaoshuai Wu.
ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing interests. ETHICAL APPROVAL This study used the Medical Information Mart for Intensive Care (MIMIC) database, which
is a freely accessible critical care database. The use of the MIMIC database is approved by the Institutional Review Boards (IRB) of the Massachusetts Institute of Technology (MIT) and Beth
Israel Deaconess Medical Center (BIDMC). The principal investigator, Wenbo Yu, has completed the necessary ethics training and obtained certification for using the MIMIC database. The
database does not contain protected health information, and all patient data are de-identified to ensure patient privacy and confidentiality. This study was approved by the Institutional
Ethics Committee of PLA Marine Corps Hospital, and the requirement for informed consent was waived due to the retrospective nature of the study and the use of anonymized data. The approval
number is YW[2023]01. ADDITIONAL INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. RIGHTS
AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use,
sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons
licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or
other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in
the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the
copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Yu, W., Jiang, W.,
Yuan, J. _et al._ Association between BMI and outcomes in critically ill patients: an analysis of the MIMIC-III database. _Sci Rep_ 14, 31127 (2024).
https://doi.org/10.1038/s41598-024-82424-5 Download citation * Received: 21 August 2024 * Accepted: 05 December 2024 * Published: 28 December 2024 * DOI:
https://doi.org/10.1038/s41598-024-82424-5 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link Sorry, a shareable link is not
currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative KEYWORDS * BMI * ICU * Critically ill * Mortality * Risk factor *
Obesity