Play all audios:
Postural orthostatic tachycardia syndrome (POTS) was previously described after severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection; however, limited data are available on
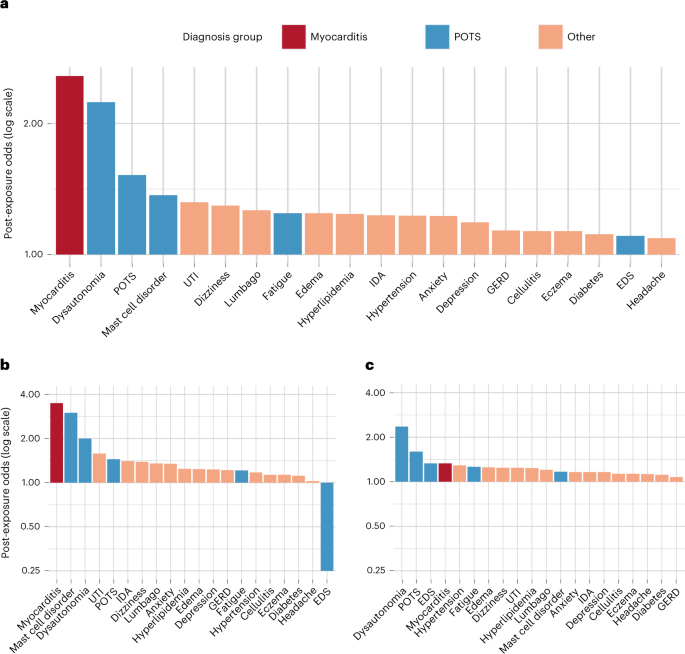
the relation of POTS with Coronavirus Disease 2019 (COVID-19) vaccination. Here we show, in a cohort of 284,592 COVID-19-vaccinated individuals, using a sequence–symmetry analysis, that the
odds of POTS are higher 90 days after vaccine exposure than 90 days before exposure; we also show that the odds for POTS are higher than referent conventional primary care diagnoses but
lower than the odds of new POTS diagnosis after SARS-CoV-2 infection. Our results identify a possible association between COVID-19 vaccination and incidence of POTS. Notwithstanding the
probable low incidence of POTS after COVID-19 vaccination, particularly when compared to SARS-Cov-2 post-infection odds, our results suggest that further studies are needed to investigate
the incidence and etiology of POTS occurring after COVID-19 vaccination.
Coronavirus Disease 2019 (COVID-19) vaccination has been shown to be safe and effective in multiple trials1,2,3,4. Vaccine pharmacovigilance has revealed diverse rare side effects in the
setting of population-wide administration5,6, including off-target cardiovascular effects, with the most well-characterized being myocarditis7,8. Reports have emerged regarding cases of
postural orthostatic tachycardic syndrome (POTS) after vaccination9. Recognized as a clinical syndrome that manifests with orthostatic intolerance and postural tachycardia, POTS is diagnosed
based on clinical features, such as orthostatic dizziness, palpitations and pre-syncope, and a 10-minute stand test or a tilt table test that demonstrate a heart rate elevation of at least
30 beats per minute from supine to standing position10,11,12. Given that POTS may be associated with small fiber or autonomic neuropathy, further diagnostic evaluation with autonomic
function tests and/or a skin biopsy for the assessment of small fiber neuropathy may be performed. POTS is now known as one of many possible features of post-acute COVID-19 syndromes that
can develop after SARS-CoV-2 infection13,14,15,16. Given that COVID-19 vaccination elicits an immunological response to the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) spike
protein, there is biological plausibility for a similar, even if attenuated, systemic response to vaccine when compared to that seen from viral exposure. Therefore, in this study, we
evaluated the relation between COVID-19 vaccination and new POTS-related diagnoses by assessing the odds of diagnosis in the baseline 90 days before first vaccine exposure versus the
subsequent 90 days after vaccine exposure in a sequence–symmetry analysis17. We first compared new POTS-related diagnosis odds to those for myocarditis and for common primary care (CPC)
diagnoses to provide benchmarks accounting for potential confounding from changes in patient engagement with the healthcare system during the pandemic as well as detection bias from the
provider standpoint. We then compared risks of new POTS diagnoses arising after vaccination compared to new POTS diagnoses arising after natural infection, to provide a broader context for
interpreting results.
For the post-vaccination analysis, we studied 284,592 patients (age 52 ± 20 years; 57% female; 63% White, 10% Asian, 8.9% African American and 12% Hispanic ethnicity). The types of
vaccinations received included: 62% Pfizer-BioNTech (BNT162b2); 31% Moderna (mRNA-1273); 6.9% Johnson & Johnson/Janssen (Ad26.COV2.S); and