Play all audios:
Discusses the level of understanding of words used in clinical discussion by patients.
Considers the impact of education and language on level of understanding.
Emphasises the importance of good communication with patients.
Introduction Communication within the doctor-patient relationship is complex due to a variety of reasons; a patient's understanding may not correspond with the clinician's vocabulary,
resulting in misunderstanding, anxiety and ill-informed decision making. We investigated the understanding of terminology commonly used in oral and maxillofacial surgery and oral medicine
clinics.
Methods We investigated patients' understanding using a questionnaire-based study in the out-patient setting. Age, gender, first language and highest educational level were recorded. The
questionnaire included multiple choice questions regarding patients' understanding of words as well as asking patients to define certain terms. Vocabulary included 'ulcer', 'blister',
'cancer', 'malignant' and 'benign'.
Results and conclusions Many patients have difficulty in understanding and explaining commonly used terminology. 'Blister' was the most commonly understood term, while 'benign' and 'lesion'
were the least well understood. 'Tumour' was mistakenly thought of as synonymous with 'malignancy' by over a third of patients. Understanding was better among those for whom English was
their first language. It is essential that all clinicians modify their language appropriately during consultations in order to deliver information in a comprehensive manner, to educate
patients on their condition thus enabling informed decision making by patients.
Communication within the doctor-patient relationship is complex for a variety of reasons; a clinician's vocabulary may not correspond with a patient's understanding of a given term,
resulting in difficulty in establishing the diagnosis for the physician, as well as confusion and potential for ill-informed decision making on the part of the patient. As a result of
patients wishing to be increasingly involved in the decision making process1,2 and receive as much information as possible,2 medicine is moving away from a paternalistic model and
patient-doctor communication therefore becomes paramount. Furthermore, effective communication has been shown to be related to improved health outcomes.3 We investigated the understanding of
terminology commonly used in oral and maxillofacial surgery and oral medicine clinics. Previous studies regarding the use of medical terminology in other settings, such as the emergency
department4 and anaesthetics5 have shown a correlation between level of understanding and educational level. In addition, studies have shown generally lower than expected levels of
understanding; O'Connell et al.6 showed that in the breast clinic setting only 65% of patients could define the word malignant. However, there are no previous studies examining understanding
of oral medicine terminology which is frequently used in both primary care dentistry as well as secondary care.
Patients attending the out-patient clinics at a London teaching hospital were recruited over two separate three day periods. Patients were asked to complete a short paper-based questionnaire
while waiting for their appointment. Participation was voluntary and anonymous, clinicians were not aware of whether patients had completed the questionnaire. For patients with physical
disability or low literacy levels, an assistant was permitted to transcribe the answers.
Section one of the questionnaire asked for demographic information including age, gender, first language, level of English spoken, and the highest level of education completed (school (up to
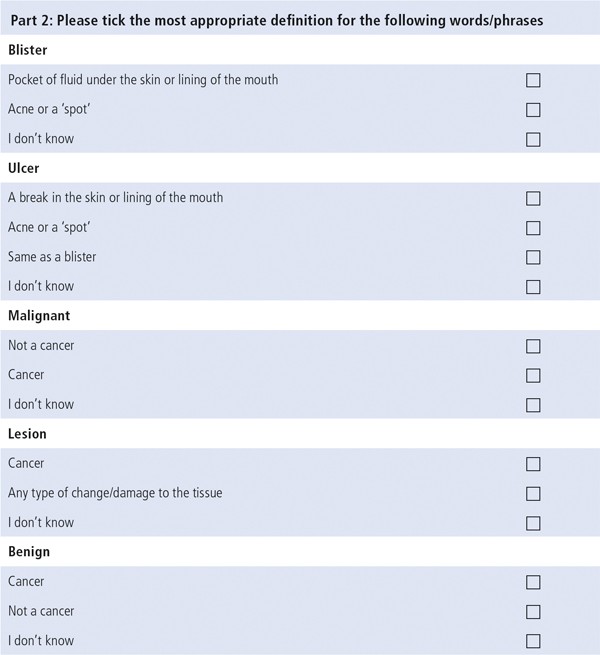
GCSE or equivalent), college (up to Alevel or equivalent), university or postgraduate education). The second section, shown in Figure 1, consisted of multiple choice questions asking
patients to select the most appropriate definition for the terms 'ulcer', 'blister', 'malignant', 'lesion', and 'benign' from three or four choices, including the option 'Do not know'. The
final section asked patients to define various terms ('biopsy', 'metastasis', 'pre-malignant', 'lymph node', and 'tumour'). The terms were selected for inclusion in the questionnaire as they
are either frequently used in both verbal and written communication to patients (such as 'ulcer', 'blister', 'biopsy'), or because it was considered vital to establish whether patients
understood them despite their less frequent use ('malignant', 'benign', 'metastasis').
Data analyses were performed using IBM SPSS Statistics, version 24; Chi-squared test was used for larger data sets, and Fisher's exact test for smaller samples. A total of 123 questionnaires
were completed. Of these, 49.6% were completed by males; overall age ranged from 15–87 years, with a mean of 44 years and two months. English was selected as their first language by 90
(73%) respondents. In addition to English, there were 22 other languages listed as the first language, the most common of which was Polish, followed by Portuguese (12%). University was the
most frequent level of education selected (29%), with 27.6% leaving education after school. College level education was selected by 24.4% of patients, with 11.1% selecting postgraduate
education and nine respondents not stating their educational level. University and post-graduate education was seen in a higher proportion of patients with English as their first language (P
= 0.498).
For the multiple choice question, 'blister' was the most commonly understood word, with 91% of those who answered selecting the correct answer; 'benign' was the least well understood, with
64% selecting the correct answer, as shown in Table 1.
In total 120 patients answered the question regarding the definition of 'blister', with 109 (90.8%) answering correctly. Of the 113 who answered and gave a level of education, there was a
significant difference (p