Play all audios:
ABSTRACT Alzheimer’s disease (AD) is a chronic pathological condition that leads to neurodegeneration, loss of intellectual abilities, including cognition and memory, and ultimately to
death. It is widely recognized that AD is a multifactorial disease, where different pathological cascades (mainly amyloid and tau) contribute to neural death and to the clinical outcome
related to the disease. The currently available drugs for AD were developed according to the one-target, one-drug paradigm. In recent times, multi-target strategies have begun to play an
increasingly central role in the discovery of more efficacious candidates for complex neurological conditions, including AD. In this study, we report on the _in vivo_ pharmacological
characterization of ARN14140, a new chemical entity, which was obtained through a multi-target structure-activity relationship campaign, and which showed a balanced inhibiting profile
against the acetylcholinesterase enzyme and the NMDA receptor. Based on the initial promising biochemical data, ARN14140 is here studied in mice treated with the amyloidogenic fragment 25–35
of the amyloid-β peptide, a consolidated non-transgenic AD model. Sub-chronically treating animals with ARN14140 leads to a prevention of the cognitive impairment and of biomarker levels
connected to neurodegeneration, demonstrating its neuroprotective potential as new AD agent. SIMILAR CONTENT BEING VIEWED BY OTHERS NEW THERAPEUTICS BEYOND AMYLOID-Β AND TAU FOR THE
TREATMENT OF ALZHEIMER’S DISEASE Article 02 December 2020 PYROGLUTAMATE AΒ CASCADE AS DRUG TARGET IN ALZHEIMER’S DISEASE Article Open access 08 December 2021 INHIBITION OF ASPARAGINE
ENDOPEPTIDASE (AEP) EFFECTIVELY TREATS SPORADIC ALZHEIMER’S DISEASE IN MICE Article 29 November 2023 INTRODUCTION Alzheimer’s disease (AD) is a chronic neurodegenerative disease
characterized by a progressive decline in memory and cognition, leading to loss of body functions and ultimately to death. AD’s etiopathology is largely unknown, although it is widely
accepted that the disease is multifactorial, involving parallel and sequential pathological cascades1,2. In recent years, two major pathways have been reported to be highly involved in
disease development: i) the extracellular aggregation of the amyloid beta peptide in protofibrils, fibrils, and plaques, and ii) the intracellular hyperphosphorylation of the tau protein,
which is subsequently detached from microtubules with consequent neuronal death3,4. Oxidative stress and neuroinflammation, with subsequent activation of glial cells, have also been reported
to play a role, likely downstream, in AD-associated neurodegeneration5,6. Because of its complexity, AD is the source of a major unmet medical need in neurology7,8. In response to this
pluralism of causes and effects, one possible research strategy is to develop a multi-target approach, leading to a single molecule acting in concert on different targets of relevance for
the disease. This should allow to gain a superior therapeutic profile, relative to single-target molecules alone, and to overcome the intrinsic conflict of combination therapies, where
positive outcomes deriving from combating the disease on multiple fronts coexist with drug-drug interaction concerns9. We recently developed a novel class of multi-target compounds, obtained
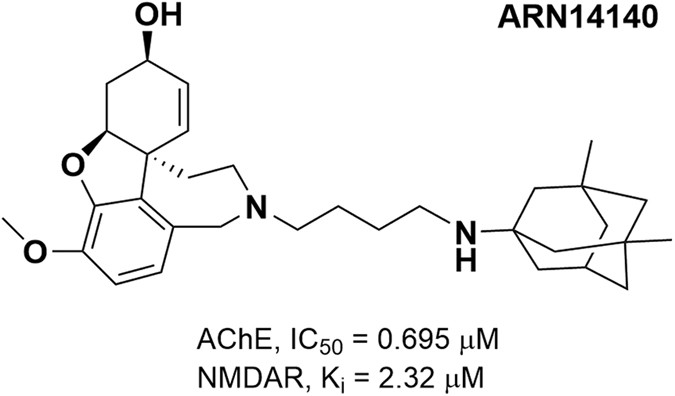
by linking together two commercially available drugs for AD, galantamine and memantine. These drugs modulate the cholinergic and glutamatergic pathways, respectively10,11. ARN14140 was the
endpoint of a mid-sized campaign of dual-target structure-activity relationship (SARs) studies. ARN14140 was the best compromise between pharmacological potency, molecular weight, and
calculated logP. When tested _in vitro_, ARN14140 showed a fairly balanced profile against both targets. It was almost equipotent for acetylcholinesterase (AChE) and the NMDA receptor
(NMDAR, Fig. 1). To investigate the effects of ARN14140 in a functional context, we used the intracerebroventricular (i.c.v.) injection of oligomeric amyloid beta peptide 25–35 (Aβ25-35) in
mice as a rapid, standardized pharmacological model of AD toxicity, which mimics both the cognitive impairment and the associated cellular neurodegeneration12,13,14,15,16,17. Preliminary
pharmacokinetic and brain penetration data showed that the compound has a suboptimal profile possibly due to a preferred compound accumulation in the liver (data not shown). To allow brain
penetration ARN14140 was given by i.c.v. delivery through osmotic mini pumps providing a continuous flow to interact with the targets. After Aβ25-35 intoxication, ARN14140 was delivered for
7 days, releasing an estimated concentration of 12 μM during the treatment. Protection against Aβ25-35 neurotoxicity was assessed either behaviorally (spontaneous alternation and passive
avoidance) or biochemically (measures of key markers of inflammation and cell integrity). RESULTS Neurodegeneration was induced by i.c.v. injection of Aβ25-35. ARN14140 was introduced into
the lateral ventricle in mice for 7 days of chronic infusion through an Alzet mini pumps implant. To guarantee full coverage for the entire infusion period, compound doses (2.5 and 7.5
μg/day for 7 days) were selected based on the _in vitro_ potency of the molecule on both targets. Since the molecular weight of ARN14140 is 506.73, we estimated a constant concentration of
the compound of almost 12 μM. This value was about 6 fold higher than the Ki for the NMDA receptor (2.3 μM) and 17 fold higher than the IC50 for the AChE enzyme (0.7 μM). Measurements were
taken 7–9 days later. Behavioral readouts included two complementary procedures to assess memory functions. We measured the following biomarkers of neuronal function and integrity: i)
hippocampal lipid peroxidation as a cell integrity marker; ii) hippocampal TNFα as a neuroinflammation marker; iii) hippocampal Synaptophysin (Syn) as a synaptic integrity marker. We also
looked at Bax and Bcl-2, two proteins involved in apoptotic pathways. Finally, we examined brain tissue integrity to quantify the damage in hippocampal pyramidal cell layers CA1. We assessed
the cholinergic loss by immunolabeling of vesicular ACh transporter (VAChT) in cortex, nucleus basalis magnocellularis (Meynert), and hippocampal formation. BEHAVIORAL TESTS Figure 2
reports the effect of ARN14140 on Aβ25-35-induced spontaneous alternation deficits in mice during the 7 days. Treatment with Aβ25-35 induced significant spontaneous alternation deficits when
compared to Sc.Aβ (Fig. 2a). ARN14140 dose-dependently reduced the Aβ25-35-induced memory deficits with full effect at a dose of 7.5 μg/day. Conversely, treatments did not affect total arm
entries as reported in Fig. 2b. Figure 2 also reports the results of the passive avoidance test. Figure 2c shows that, with respect to untreated mice or those treated with Sc.Aβ, the Aβ25-35
treatment induced highly significant deficits in mice performance both as step-through latency and as escape latency during the retention session (Fig. 2c,d, respectively). Treatment with
ARN14140 before training dose-dependently reduced the Aβ25-35-induced deficits, with significant prevention at a dose of 7.5 μg/day on both parameters (Fig. 2c,d). The ARN14140 effect was
not associated with the typical NMDAR antagonist drawbacks such as increased step-through latency or lower shock sensitivity (data not shown). In summary, the present findings indicate that
chronic infusion of ARN14140 in the lateral ventricles fully protects mice from the development of short-term memory deficits after i.c.v. injection of Aβ25-35. Since the Y-maze performance
mimics spatial learning and is driven at the hippocampal level, it can be concluded that ARN14140 provides a functional neuroprotective effect for this type of memory. ARN14140 was also
effective in the passive avoidance test, which is a fear-motivated test classically used to assess short or long-term memory. Therefore, the data also suggest ARN14140 has an effect on this
type of short-term memory. Both memory types are typically affected in AD patients18. BIOCHEMICAL ANALYSES We then analyzed the effect of ARN14140 on specific markers related to
neurodegeneration to assess whether the functional neuroprotection seen behaviorally could be associated with a cellular neuroprotection. First, we studied lipid peroxidation, a well-known
marker of oxidative stress, which is associated with neurodegenerative diseases19,20. As shown in Fig. 3a, treatment with Aβ25-35 induced a highly significant increase in lipid peroxidation
in mouse hippocampus compared to Sc.Aβ/V-injected mice. ARN14140 infusion significantly prevented the Aβ25-35-induced increase of lipid peroxidation. The effect of ARN14140 was complete at
7.5 μg/day, suggesting that, at this dose, the compound fully reverses the Aβ25-35-induced neuronal oxidative damage. AD has been associated with activation of inflammatory pathways
including the hyper secretion of pro-inflammatory, neurotoxic cytokines such as TNFα by reactive microglia and monocytes21. As shown in Fig. 3b, after treatment with Aβ25-35, the hippocampal
content of TNFα increased compared to ScAβ-injected mice (+89% increase, p < 0.05 using a two-column test, red bar vs. empty bar). As reported in the same figure, continuous i.c.v.
infusion of ARN14140 for 7 days tended to prevent the increase in TNFα levels, although the ANOVA failed to reach significance, a similar attenuation was noted with both regimens, 2.5 and
7.5 μg/day. Since TNFα is thought to be part of the initiation mechanism of immune-mediated neurotoxic inflammation22, the data suggest that ARN14140 can possibly provide protection against
AD-related inflammatory events. We then investigated the Synaptophysin expression in hippocampus. Syn is a 38 kDa protein, present in virtually all neurons, which participates in synaptic
transmission. Reduction of Syn is an index of synaptic function and many reports suggest that Syn levels are lowered by neurodegeneration23,24. In our study, treatment with Aβ25-35 induced a
highly significant decrease of hippocampal Synaptophysin content (−34%) as compared to Sc.Aβ-injected mice (cfr white bar with red bar in Fig. 3c). At a dose of 7.5 μg/day, ARN14140
significantly prevented the Aβ25-35-induced decrease in Syn in hippocampus, indicating that, at the top dose, ARN14140 can fully protect synaptic function. Lastly, we focused on the Bcl-2
protein family. An increase of apoptotic cell death has been reported in the brain tissue of AD patients25,26. This event has been associated with a dysregulation of the Bcl-2 proteins
balance. The Bcl-2 proteins are a family of evolutionarily related proteins mainly involved in regulating programmed cell death (apoptosis). Bax is the most studied member of the family and
has pro-apoptotic activity, while Bcl-2 itself is the most investigated family member with anti-apoptotic activity. As reported in Fig. 4a, Aβ25-35 administration induced a highly
significant increase (+90%) in hippocampal Bax content compared to Sc.Aβ-injected mice. This translates into a highly significant increase (+85%) of Bax/Bcl-2 ratio relative to
Sc.Aβ-injected mice (Fig. 4b). The continuous infusion of ARN14140 for 7 days dose-dependently reduced the increase in Bax content in mouse hippocampus and rebalanced the altered Bax/Bcl-2
ratio (see Fig. 4a,b). In this study, both doses led to a significant effect although the max was observed with the top dose. In summary, it has been reported that Aβ peptide affect Bax and
Bcl-2 expression levels in AD human neurons27. Our findings indicate that ARN14140 can rebalance these mechanisms through which can possibly reduce AD-associated apoptosis. MORPHOLOGICAL
ALTERATIONS We studied the neuroprotective potential of ARN14140 at a cellular level by evaluating its effect on Aβ25-35 induced CA1 mouse hippocampus cell loss. Cresyl violet was used as a
vital stain and a significant decrease in cell count was observed in Aβ25-35 treated mice 9 days after i.c.v. injection of the peptides (Fig. 5a,b). The continuous infusion of ARN14140
treatment dose-dependently prevented the effect in viable cells, with a significant difference when compared to the Aβ25-35/V-treated group at a dose of 7.5 μg/day (Fig. 5c). We then
analyzed the acetylcholine marker in different samples. VAChT was stained. VAChT is responsible for loading into neuronal endings ready for secretion. A decrease in VAChT indicates less
acetylcholine, most likely due to loss of cholinergic neurons. The qualitative analysis of immunolabeling of VAChT showed large immunoreactive fibers in the hippocampus especially in the CA3
area (see Fig. 6a) and a more punctae labeling in the different cortex layers of Sc.Aβ/V-treated animals (Fig. 6b). In Aβ25-35-treated mice, a net decrease in immunolabeling was observed
(Fig. 6c,d), which could be attributed to the small loss of neurons measured in the hippocampus. Poor brain integrity due to the chronic implantation of the pump meant that drug analysis
could only be done on qualitative bases (marked glial injury, with high variability among mice). Nonetheless a clear trend of increased density of cholinergic terminals was observed in those
mice receiving ARN14140. The effect was detectable at the high dose with an intense labeling of cholinergic terminals in the hippocampus and cortex, as pointed out in Fig. 6g,h. Our
morphological findings confirm at a cellular level that ARN14140 infusion had a beneficial effect on development of neurotoxicity. The effect on CA1 hippocampal cell loss was clear and
quantitative, allowing in turn a quantitative analysis of the trend of cholinergic markers. DISCUSSION AD is a complex and multifactorial disease whose causes are still partially unknown. It
is widely accepted that AD is associated with a series of concomitant biochemical events that contribute to the pathophysiology of the disease. In the search for more effective therapeutic
approaches to AD, an emerging option is to design multi-target molecules. The concept is that multi-target molecules can act at several levels of the AD-related neurodegenerative cascade/s28
at the same time. This should provide a profile with greater therapeutic benefits and reduced side effects, compared to single-target compounds. Pursuing this line of research, we recently
designed a novel class of multi-target molecule: dual NMDAR/AChE inhibitors. As starting scaffolds, we used two well-known currently available drugs, galantamine and memantine. We “linked”
them into a single compound to form a new class of molecules acting on both targets at the same time. Galantamine was chosen because of its intrinsic dual mechanism of action as an
anticholinesterase inhibitor (potentiation of endogenous ACh content) and allosteric modulator of neuronal nicotinic receptors (increase of glutamate levels)29,30. Memantine was chosen
because of its reduced NMDA-related side effects, which may be due to its selective interaction with extrasynaptic NMDAR (selective blockade of extrasynaptic NMDAR does not affect the
postsynaptic NMDAR, which is believed to mediate the beneficial glutamate effects in the CNS)31. ARN14140 was the best representative of this new chemical class, which has been the subject
of an international PCT patent application (WO2013160728A1). Based on the initial biochemical characterization, which has already been published10, ARN14140 was chosen because it is a fairly
balanced molecule. It interacts equally with the AChE enzyme and the NMDA receptor. In this study, the molecule was tested for its ability to prevent the biochemical and behavioral
detrimental effects of the i.c.v. injection of Aβ25-35. The model is thought to mimic some key phenotypes of AD (mainly cognitive/memory impairment and neurodegeneration), and has already
been used to determine neuroprotective effect of galantamine and memantine alone32,33. In the present study, ARN14140 was given i.c.v. to minimize all possible issues of brain penetration,
since preliminary data showed a suboptimal pharmacokinetic (PK) profile. To maintain a constant inhibition of the AChE and NMDA targets for the required length of time, the compound was
given by chronic infusion with osmotic mini-pumps, providing a continuous flow to interact with the targets. For these reasons, ARN14140 is a prototype suitable to explore a concept but
insufficient for becoming a medicine. We are now seeking to chemically optimize the PK profile and to explore new delivery strategies, such as transdermal patches, which could minimize the
unfavorable plasma profile and maximize ARN14140 therapeutic efficacy. The Aβ25-35-treated animals show a statistically relevant cognitive impairment as well as alteration of the major
markers of neurodegeneration and cell death. ARN14140 was able to rescue the behavioral impairment in two different tasks and to balance the levels of biomarkers of neurodegeneration,
synaptic plasticity, and apoptosis, which were modified by treatment with Aβ25-35. We should recall here that ARN14140 was simultaneously administered to Aβ25-35, showing that the molecule
could be able to tackle neurodegeneration in the very early stages of the disease. However, based on our data, we could not argue whether ARN14140 is also able to reverse the neuronal damage
already present in the brain of AD patients quite in advance of the symptom onset. When administered to mice for 7 days at a dose of 7.5 μg/day, ARN14140 completely reverted the
Aβ25-35-induced neurotoxicity in terms of behavioral tasks and biomarkers. We believe this highly positive feature was due to the synergistic potentiation arising from the simultaneous
engagement of NMDAR and AChE. To support this hypothesis is the increasing evidence that the glutamatergic and cholinergic neuronal systems influence each other, and that their joint
dysfunction is crucial to the effects produced by AD34. In particular, based on our recent findings on memantine and galantamine in combination35, we may hypothesize that the galantamine
moiety could determine AChE inhibition, tackling memory loss and cognitive impairment. In addition, the galantamine function is expected to contrast NMDA-mediated neurotoxicity through the
allosteric modulation of nicotinic receptors, thus potentiating memantine’s efficacy in promoting neuronal survival. This interpretation is, however, rather speculative and cannot rule out
the involvement of additional, as yet unknown, mechanisms. Our data suggests that ARN14140 could serve as the initial prototype for a pharmacological advancement with respect to the current
AD therapies, since it merges complementary activities that could otherwise only be achieved by administering a cocktail of molecules36. Overall, the present study further confirms that
multi-target compounds can play an important role in the treatment of complex neurological disorders, and may represent a novel paradigm in anti-AD drug discovery research. METHODS ANIMALS
AND TREATMENT GROUPS All experiments were carried out in Amylgen facility (Montpellier, France). Animal procedures were carried out in strict adherence to the European Community Council
Directive of September 22, 2010 (2010/63/UE). All experiments and protocols were authorised and approved by the French Ministry of Research, as well as by the Regional Animal Welfare
Committee. All efforts were made to minimise the number of animals used. A total of 72 male Swiss mice (RjOrl:SWISS, Janvier, Saint Berthevin, France) aged 6 weeks old and weighing 30–35 g,
were used for Aβ25-35 intoxications. Animals were housed in the regulated animal facility of Amylgen (agreement #A 34-169-002 from May 02, 2014), in plastic cages with free access to food
and water, except during behavioural experiments. They were kept in a regulated environment under a 12 h light/dark cycle (lights off at 07:00 pm). EXPERIMENTAL PROTOCOL Four experimental
groups were used, with n = 18 per group: scrambled Aβ25-35 (Sc.Aβ) (9 nmol injected intracerebroventricularly (i.c.v.) once) + vehicle solution (infused i.c.v. during 7 days), Aβ25-35 (9
nmol injected i.c.v. once) + vehicle solution (infused i.c.v. during 7 days), Aβ25-35 (9 nmol injected i.c.v. once) + ARN1410 (infused i.c.v. at 2.5 μg/day during 7 days), and Aβ25-35 (9
nmol injected i.c.v. once) + ARN1410 (infused i.c.v. at 7.5 μg/day during 7 days). Animals were kept with n = 8 individuals per cage, the treatment being coded and blind to the experimenter.
On day 0, mice were anesthetized using isoflurane 2.5% inhalation. They were injected i.c.v. with Aβ25-35 or Sc.Aβ peptide. An Alzet micro-osmotic pump delivering ARN14140 or vehicle
solution was placed subcutaneously with the brain cannula into the lateral ventricle. On day 7, the spontaneous alternation performance was tested for n = 12 animals in the Y-maze test, an
index of spatial working memory. On days 8 and 9, the contextual long-term memory was assessed using the step-through type passive avoidance procedure for the same animals, with training
session on day 8 and retention session on day 9. On day 9, all animals were sacrificed. For half of the animals (n = 6 per group), the hippocampi and frontal cortex were dissected out and
frozen in liquid nitrogen before being stored at −80 °C before analyses. One hippocampus was used to measure lipid peroxidation levels in tissue extracts. One cortex was used for ELISA
assays. A second set of animals, with n = 6 animal per experimental group, were administered as described and transcardially perfused at day 9 with paraformaldehyde to allow brain slicing
and histology/immunohistochemistry. These animals were not tested behaviorally. DRUGS AND ADMINISTRATION PROCEDURES The Aβ25-35 peptide (SC489) and its control scrambled peptide, containing
the 11 amino-acids of Aβ25-35 but in a random order, Sc.Aβ (SC492) were purchased from Polypeptides (France). Peptides were solubilized in sterile distilled water at a concentration of 3 mM
and the homogeneous oligomeric preparation of Aβ25-35 peptides was performed according to Amylgen’s own procedure, leading to a > 98% pure soluble oligomers solution similar as described
by Zussy _et al_.12,13. A quality control analysis for Aβ25-35 aggregation was systematically performed by analyzing Sc.Aβ and Aβ25-35 solutions using a light scattering assay before each
injection of Aβ25-35 peptides. The Sc.Aβ solution (3 mM) does not aggregate and must show an OD320 nm < 0.2 while the Aβ25-35 solution at the same concentration must show an OD320 nm >
0.8. Each mouse was anesthetized with isoflurane 2.5% and injected i.c.v. with Aβ25-35 or Sc.Aβ peptides (9 nmol/mouse) in a final volume of 3 μL per mouse. The injection was performed
using the hand-free method described by Haley & McCormick37, with the injection coordinates from Bregma: AP −0.4 mm, L 1.0 mm, V −2.5 mm (Paxinos and Franklin, 2012), as previously
described14,32,38,39,40,41. ARN14140 was solubilized in PBS/0.5% acetic acid, pH = 6, at a concentration of 13.3 mg/mL and then diluted to the appropriate concentrations. It was infused
using Alzet micro-osmotic pumps 1007D delivering 0.5 μL/h over 7 days (total volume 100 μL, solution concentrations of 0.21 g/L and 0.63 g/L). Each pump was connected to a brain infusion kit
III (Charles River, L’Arbresles, France). Behavioral studies were carried out blind to the experimenter. SPONTANEOUS ALTERNATION PERFORMANCES The spatial working memory was examined by
measuring the spontaneous alternation behaviour of the mice in the Y-maze14,32,38,39,40,41. The Y-maze is made of grey polyvinylchloride. Each arm is 40 cm long, 13 cm high, 3 cm wide at the
bottom, 10 cm wide at the top, and converging at an equal angle. Seven days after Aβ25-35 or Sc.Aβ peptide injection, each mouse was placed at the end of one arm and allowed to move freely
through the maze during an 8 min session. The series of arm entries, including possible returns into the same arm, was recorded visually. An alternation was defined as entries into all three
arms on consecutive occasions. The number of maximum alternations was the total number of arm entries minus two and the percentage of alternation was calculated as actual
alternations/maximum alternations × 100. Measured parameters included the percentage of alternation (memory index) and total number of arm entries (exploration index). PASSIVE AVOIDANCE TEST
The contextual long-term memory of the animals was assessed using a two-session step-through passive avoidance procedure32,40,41. The apparatus consisted of two compartments (15 × 20 × 15
cm high), one illuminated with white polyvinylchloride walls and the other darkened with black polyvinylchloride walls and a grid floor for electrical shocks. A guillotine door separated
each compartment. A 60 W lamp positioned 40 cm above the apparatus lights up the white compartment during the experiment. Scrambled foot shocks could be delivered to the grid floor using a
shock generator scrambler (Lafayette Instruments, Lafayette, USA). Training: 8 days after Aβ25-35 or Sc.Aβ peptide injection, each mouse was placed into the white compartment. After 5 s, the
door was raised. When the mouse entered the darkened compartment and placed all its paws on the grid floor, the door was closed and the foot shock (0.3 mA) delivered for 3 s. The latency
spent to enter the dark compartment and the number of vocalisations was recorded. None of the treatment affected the step-through latency (H = 0.31, p > 0.05) or vocalisations (H = 2.83,
p > 0.05) during training. Retention: 24 h after training (9 days after Aβ25-35 or Sc.Aβ peptide injection), each mouse was placed again into the white compartment. After 5 s, the door
was raised and the step-through latency (latency to enter the dark compartment) was recorded up to 300 s. LIPID PEROXIDATION The quantification of lipid peroxidation in tissue extracts is
based on Fe(III)xylenol orange complex formation according to Hermes-Lima _et al_.42. Six mice for each group were sacrificed by decapitation, without anesthesia nor sedation, 9 days after
Aβ25-35 or Sc.Aβ peptide injection. The brains were rapidly removed, weighed and kept in liquid nitrogen until assayed. After thawing, one hippocampus per mouse was homogenized in cold
methanol (1/10 w/v), centrifuged at 1,000 _g_ for 5 min and the supernatant placed in an Eppendorf tube. The reaction volume of each homogenate was added to FeSO4 1 mM, H2SO4 0.25 M, xylenol
orange 1 mM and incubated for 30 min at room temperature. After reading the absorbance at 580 nm (A5801), 10 μL of cumene hydroperoxide (CHP) 1 mM was added to the sample and incubated for
30 min at room temperature, to determine the maximal oxidation level. The absorbance was measured at 580 nm (A5802). The level of lipid peroxidation was determined as CHP equivalents
according to: CHPE = A5801/A5802 × [CHP (nmol)] and expressed as CHP equivalents per mg of tissue and as a percentage of the control group data (V-treated Sc.Aβ-administered mice).
BIOCHEMICAL ANALYSES Nine days after Aβ25-35 or Sc.Aβ injection, 6 animals were killed by decapitation, and hippocampi from 6 animals were dissected out, weighted and immediately frozen in
liquid nitrogen. 6 hippocampi were used per group for ELISA assays. For ELISA analysis, 6 hippocampi were homogenized in 50 mM Tris-150 mM NaCl buffer, pH 7.5 in eppendorf tubes, and
sonicated for 2 × 10 s at 4 °C (2 × 1,0 kJ, BANDELIN Sonopuls HD3200). After centrifugation (16100 g for 15 min, 4 °C), the supernatants were assayed immediately by ELISA assay for tumor
necrosis factor alpha (TNFα) (EMTNFA01, ThermoScientific), synaptophysin (Syn) (E90425M, USCN), Bax (E91343M, USCN), and Bcl-2 (E90778M, USCN) according to the manufacturer instructions. For
each assay, absorbance was read at 450 nm and sample concentration was calculated using the standard curve. Results are expressed in pg of marker per mg of tissue. Protein concentration was
determined in brain homogenates with the BCA protein assay kit (Pierce Perbio Science, France). HISTOLOGY/IMMUNOHISTOCHEMISTRY Nine days after Aβ25-35 or Sc.Aβ peptide injection, 6 mice
from each group were anesthetised by 200 μL intraperitoneal injection of a premix of ketamine (80 mg/kg) and xylazine (10 mg/kg), and quickly perfused transcardially with 100 mL of saline
solution (NaCl 0.9%) followed by 100 mL of paraformaldehyde 4%. Brains were removed and kept for 48 h in the fixative solution at 4 °C, then cut into 10 μm thickness coronal sections using a
cryostat. Sections were stained with 0.2% cresyl violet reagent (Sigma-Aldrich), dehydrated with graded ethanol, treated with toluene, and mounted with Mountex medium (BDH Laboratory
Supplies, Poole, Dorset, UK). Examination of the CA1 area was performed using digitalized slices using a Nanozoomer virtual microscopy system (Hamamatsu, Massy, France). CA1 measurement and
pyramidal cell counts were processed using a 40 × objective using ImageJ software (NIH). Data were expressed as mean number of viable cells per mm, from at least four slices × 3 CA1 fields ×
2 hemispheres for each group, according to the previously reported method12. For immunohistochemical labeling of the vesicular acetylcholine transporter (VAChT), sections were incubated
overnight at 4 °C with Rabbit monoclonal anti-VAChT (SOSV00002G, Thermofisher). Then, sections were incubated with Rabbit biotinylated secondary antibody (B8895, Sigma-Aldrich) and incubated
for 1 h in avidin-biotin complex (ABC Vector laboratory). Signal was detected with the diaminobenzidine kit (Vector, Laboratories). Examination of the stained area was performed using
digitalized slices using Optic microscope (Leica). STATISTICAL ANALYSES All values, except passive avoidance latencies, were expressed as mean ± S.E.M. Statistic analyses were performed on
the different conditions using one-way ANOVA (_F_ value), followed by the Dunnett’s post-hoc multiple comparison test. Passive avoidance latencies do not follow a Gaussian distribution,
since upper cut-off times are set. They were therefore analyzed using a Kruskal-Wallis non-parametric ANOVA (_H_ value), followed by a Dunn’s multiple comparison test. _p_ < 0.05 was
considered as statistically significant. ADDITIONAL INFORMATION HOW TO CITE THIS ARTICLE: Reggiani, A. M. _et al_. _In Vivo_ Characterization of ARN14140, a Memantine/Galantamine-Based
Multi-Target Compound for Alzheimer’s Disease. _Sci. Rep._ 6, 33172; doi: 10.1038/srep33172 (2016). REFERENCES * Querfurth, H. W. & LaFerla, F. M. Alzheimer’s disease. N Engl J Med 362,
329–344 (2010). CAS PubMed Google Scholar * Citron, M. Alzheimer’s disease: strategies for disease modification. Nat. Rev. Drug Discov. 9, 387–398 (2010). CAS PubMed Google Scholar *
Hardy, J. A. & Higgins, G. A. Alzheimer’s disease: the amyloid cascade hypothesis. Science 256, 184–185 (1992). ADS CAS PubMed Google Scholar * Grundke-Iqbal, I. et al.
Microtubule-associated protein tau. A component of Alzheimer paired helical filaments. J. Biol. Chem. 261, 6084–6089 (1986). CAS PubMed Google Scholar * von Bernhardi, R. & Eugenín,
J. Alzheimer’s disease: redox dysregulation as a common denominator for diverse pathogenic mechanisms. Antioxid. Redox Signal. 16, 974–1031 (2012). CAS PubMed Google Scholar * Rosini, M.,
Simoni, E., Milelli, A., Minarini, A. & Melchiorre, C. Oxidative stress in Alzheimer’s disease: are we connecting the dots? J. Med. Chem. 57, 2821–2831 (2014). CAS PubMed Google
Scholar * Association, A. s. 2013 Alzheimer’s disease facts and figures. Alzheimers Dement 9, 208–245 (2013). Google Scholar * Ballard, C. et al. Alzheimer’s disease. Lancet 377, 1019–1031
(2011). PubMed Google Scholar * Rosini, M. Polypharmacology: the rise of multitarget drugs over combination therapies. Future Med. Chem. 6, 485–487 (2014). ADS CAS PubMed Google
Scholar * Simoni, E. et al. Combining galantamine and memantine in multitargeted, new chemical entities potentially useful in Alzheimer’s disease. J. Med. Chem. 55, 9708–9721 (2012). CAS
PubMed Google Scholar * Rosini, M., Simoni, E., Minarini, A. & Melchiorre, C. Multi-target design strategies in the context of Alzheimer’s disease: acetylcholinesterase inhibition and
NMDA receptor antagonism as the driving forces. Neurochem. Res. 39, 1914–1923 (2014). CAS PubMed Google Scholar * Zussy, C. et al. Time-course and regional analyses of the
physiopathological changes induced after cerebral injection of an amyloid β fragment in rats. Am. J. Pathol. 179, 315–334 (2011). CAS PubMed PubMed Central Google Scholar * Zussy, C. et
al. Alzheimer’s disease related markers, cellular toxicity and behavioral deficits induced six weeks after oligomeric amyloid-β peptide injection in rats. PLoS One 8, e53117 (2013). ADS CAS
PubMed PubMed Central Google Scholar * Maurice, T., Lockhart, B. P. & Privat, A. Amnesia induced in mice by centrally administered beta-amyloid peptides involves cholinergic
dysfunction. Brain Res. 706, 181–193 (1996). CAS PubMed Google Scholar * Lahmy, V. et al. Blockade of Tau hyperphosphorylation and Aβ1;–42; generation by the aminotetrahydrofuran
derivative ANAVEX2-73, a mixed muscarinic and σ1 receptor agonist, in a nontransgenic mouse model of Alzheimer’s disease. Neuropsychopharmacology 38, 1706–1723 (2013). CAS PubMed PubMed
Central Google Scholar * Klementiev, B. et al. A neural cell adhesion molecule-derived peptide reduces neuropathological signs and cognitive impairment induced by Abeta25-35. Neuroscience
145, 209–224 (2007). CAS PubMed Google Scholar * Kaminsky, Y. G., Marlatt, M. W., Smith, M. A. & Kosenko, E. A. Subcellular and metabolic examination of amyloid-beta peptides in
Alzheimer disease pathogenesis: evidence for Abeta(25–35). Exp. Neurol. 221, 26–37 (2010). CAS PubMed Google Scholar * Morris, R. G. & Kopelman, M. D. The memory deficits in
Alzheimer-type dementia: a review. Q. J. Exp. Psychol. A 38, 575–602 (1986). CAS PubMed Google Scholar * Bradley-Whitman, M. A. & Lovell, M. A. Biomarkers of lipid peroxidation in
Alzheimer disease (AD): an update. Arch. Toxicol. 89, 1035–1044 (2015). CAS PubMed PubMed Central Google Scholar * Casado, A., Encarnación López-Fernández, M., Concepción Casado, M.
& de La Torre, R. Lipid peroxidation and antioxidant enzyme activities in vascular and Alzheimer dementias. Neurochem. Res. 33, 450–458 (2008). CAS PubMed Google Scholar * Rivest, S.
Regulation of innate immune responses in the brain. Nat. Rev. Immunol. 9, 429–439 (2009). CAS PubMed Google Scholar * Heneka, M. T. et al. Neuroinflammation in Alzheimer’s disease. Lancet
Neurol. 14, 388–405 (2015). CAS PubMed PubMed Central Google Scholar * Love, S. et al. Premorbid effects of APOE on synaptic proteins in human temporal neocortex. in Neurobiol. Aging
Vol. 27, 797–803 (United States, 2006). Google Scholar * Masliah, E. et al. Synaptic and neuritic alterations during the progression of Alzheimer’s disease. Neurosci. Lett. 174, 67–72
(1994). CAS PubMed Google Scholar * Shimohama, S. Apoptosis in Alzheimer’s disease–an update. Apoptosis 5, 9–16 (2000). CAS PubMed Google Scholar * Hugon, J., Terro, F., Esclaire, F.
& Yardin, C. Markers of apoptosis and models of programmed cell death in Alzheimer’s disease. J. Neural. Transm. Suppl. 59, 125–131 (2000). CAS PubMed Google Scholar * Paradis, E.,
Douillard, H., Koutroumanis, M., Goodyer, C. & LeBlanc, A. Amyloid beta peptide of Alzheimer’s disease downregulates Bcl-2 and upregulates bax expression in human neurons. J. Neurosci.
16, 7533–7539 (1996). CAS PubMed PubMed Central Google Scholar * Cavalli, A. et al. Multi-target-directed ligands to combat neurodegenerative diseases. J. Med. Chem. 51, 347–372 (2008).
CAS PubMed Google Scholar * Samochocki, M. et al. Galantamine is an allosterically potentiating ligand of neuronal nicotinic but not of muscarinic acetylcholine receptors. J. Pharmacol.
Exp. Ther. 305, 1024–1036 (2003). CAS PubMed Google Scholar * Takada-Takatori, Y. et al. Neuroprotective effects of galanthamine and tacrine against glutamate neurotoxicity. Eur. J.
Pharmacol. 549, 19–26 (2006). CAS PubMed Google Scholar * Xia, P., Chen, H. S., Zhang, D. & Lipton, S. A. Memantine preferentially blocks extrasynaptic over synaptic NMDA receptor
currents in hippocampal autapses. J. Neurosci. 30, 11246–11250 (2010). CAS PubMed PubMed Central Google Scholar * Meunier, J., Ieni, J. & Maurice, T. The anti-amnesic and
neuroprotective effects of donepezil against amyloid beta25-35 peptide-induced toxicity in mice involve an interaction with the sigma1 receptor. Br. J. Pharmacol. 149, 998–1012 (2006). CAS
PubMed PubMed Central Google Scholar * Maurice, T. Protection by sigma-1 receptor agonists is synergic with donepezil, but not with memantine, in a mouse model of amyloid-induced memory
impairments. Behav. Brain Res. 296, 270–278 (2016). CAS PubMed Google Scholar * Parsons, C. G., Danysz, W., Dekundy, A. & Pulte, I. Memantine and cholinesterase inhibitors:
complementary mechanisms in the treatment of Alzheimer’s disease. Neurotox. Res. 24, 358–369 (2013). CAS PubMed PubMed Central Google Scholar * Lopes, J. P., Tarozzo, G., Reggiani, A.,
Piomelli, D. & Cavalli, A. Galantamine potentiates the neuroprotective effect of memantine against NMDA-induced excitotoxicity. Brain Behav. 3, 67–74 (2013). PubMed PubMed Central
Google Scholar * Busquet, P. et al. Synergistic effects of galantamine and memantine in attenuating scopolamine-induced amnesia in mice. J. Pharmacol. Sci. 120, 305–309 (2012). CAS PubMed
Google Scholar * Haley, T. J. & Mccormick, W. G. Pharmacological effects produced by intracerebral injection of drugs in the conscious mouse. Br. J. Pharmacol. Chemother. 12, 12–15
(1957). CAS PubMed PubMed Central Google Scholar * Maurice, T., Su, T. P. & Privat, A. Sigma1 (sigma 1) receptor agonists and neurosteroids attenuate B25-35-amyloid peptide-induced
amnesia in mice through a common mechanism. Neuroscience 83, 413–428 (1998). CAS PubMed Google Scholar * Meunier, J., Villard, V., Givalois, L. & Maurice, T. The γ-secretase inhibitor
2-[(1R)-1-[(4-chlorophenyl)sulfonyl](2,5-difluorophenyl) amino]ethyl-5-fluorobenzenebutanoic acid (BMS-299897) alleviates Aβ1-42 seeding and short-term memory deficits in the Aβ25-35 mouse
model of Alzheimer’s disease. Eur. J. Pharmacol. 698, 193–199 (2013). CAS PubMed Google Scholar * Villard, V. et al. Antiamnesic and neuroprotective effects of the aminotetrahydrofuran
derivative ANAVEX1-41 against amyloid beta(25-35)-induced toxicity in mice. Neuropsychopharmacology 34, 1552–1566 (2009). CAS PubMed Google Scholar * Villard, V., Espallergues, J.,
Keller, E., Vamvakides, A. & Maurice, T. Anti-amnesic and neuroprotective potentials of the mixed muscarinic receptor/sigma 1 (σ1) ligand ANAVEX2-73, a novel aminotetrahydrofuran
derivative. J. Psychopharmacol. 25, 1101–1117 (2011). CAS PubMed Google Scholar * Hermes-Lima, M., Willmore, W. G. & Storey, K. B. Quantification of lipid peroxidation in tissue
extracts based on Fe(III)xylenol orange complex formation. Free Radic. Biol. Med. 19, 271–280 (1995). CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS This work was
supported by the Italian Institute of Technology and the University of Bologna. We thank Amylgen (Montferrier-sur-Lez, France) for the technical support. We thank Prof. Daniele Piomelli and
Dr. Giuseppe Giardina for the useful discussions. We thank Grace Fox for editing and proofreading the manuscript. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Drug Discovery and
Development, Istituto Italiano di Tecnologia, Genova, Italy Angelo M. Reggiani & Andrea Cavalli * Department of Pharmacy and Biotechnology, University of Bologna, Bologna, Italy Elena
Simoni, Roberta Caporaso, Anna Minarini, Michela Rosini & Andrea Cavalli * Amylgen, Montferrier-sur-Lez, France Johann Meunier, Emeline Keller & Tangui Maurice * INSERM U1198,
Montpellier, France Tangui Maurice * University of Montpellier, Montpellier, France Tangui Maurice * EPHE, Paris, France Tangui Maurice Authors * Angelo M. Reggiani View author publications
You can also search for this author inPubMed Google Scholar * Elena Simoni View author publications You can also search for this author inPubMed Google Scholar * Roberta Caporaso View author
publications You can also search for this author inPubMed Google Scholar * Johann Meunier View author publications You can also search for this author inPubMed Google Scholar * Emeline
Keller View author publications You can also search for this author inPubMed Google Scholar * Tangui Maurice View author publications You can also search for this author inPubMed Google
Scholar * Anna Minarini View author publications You can also search for this author inPubMed Google Scholar * Michela Rosini View author publications You can also search for this author
inPubMed Google Scholar * Andrea Cavalli View author publications You can also search for this author inPubMed Google Scholar CONTRIBUTIONS A.M.R. provided expertise of behavioural and
biochemical analyses, analysed the data and wrote the paper; E.S. performed the synthesis of ARN14140 and wrote the paper; R.C. performed the synthesis of ARN14140; A.M. discussed
prepublication results, contributed to the interpretation of the data and reviewed the manuscript; J.M., E.K. and T.M. performed the biological studies; M.R. contributed to the analysis and
interpretation of the results, and wrote the paper; A.C. designed the research study, analysed and interpreted results, and wrote the paper. All authors have given approval to the final
version of the paper. ETHICS DECLARATIONS COMPETING INTERESTS The authors declare no competing financial interests. RIGHTS AND PERMISSIONS This work is licensed under a Creative Commons
Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the
credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of
this license, visit http://creativecommons.org/licenses/by/4.0/ Reprints and permissions ABOUT THIS ARTICLE CITE THIS ARTICLE Reggiani, A., Simoni, E., Caporaso, R. _et al._ _In Vivo_
Characterization of ARN14140, a Memantine/Galantamine-Based Multi-Target Compound for Alzheimer’s Disease. _Sci Rep_ 6, 33172 (2016). https://doi.org/10.1038/srep33172 Download citation *
Received: 07 June 2016 * Accepted: 17 August 2016 * Published: 09 September 2016 * DOI: https://doi.org/10.1038/srep33172 SHARE THIS ARTICLE Anyone you share the following link with will be
able to read this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing
initiative