Play all audios:
CHANGES IN OTHER FLEXIBILITIES Beyond vaccines, tests and treatments, the emergency declarations have granted a range of flexibilities within the health care system that will end. For
example: The three-day hospitalization requirement that Medicare patients had to meet before continued care at a skilled nursing facility would be covered was waived during the pandemic.
That rule goes back into effect. Also, throughout the pandemic, Medicare Advantage plans have been required to charge in-network prices for care provided at out-of-network facilities. This
flexibility was part of the national emergency that ended April 10. A bigger change has to do with Medicaid coverage. People who have been on Medicaid these last few years could soon be
without it due to a continuous enrollment provision that ended on March 31. (This benefit, which barred states from removing people from Medicaid during the pandemic, was previously tied to
the public health emergency but ended earlier.) In fact, KFF estimates that between 5 million and 14 million people could lose their Medicaid insurance. It’s important for people with
Medicaid to pay attention to their plan in the coming months, said Salama Freed, an assistant professor in the Department of Health Policy and Management at George Washington University’s
Milken Institute School of Public Health. And if they get disenrolled, they’ll need to have another option and prepare for any extra costs. “I don’t want anyone to be caught off guard
losing their insurance coverage and have to scramble and find something else,” Freed said. “I just want people to have their ducks in a row, so that they’re not caught flat-footed.” Some
people who get disenrolled from Medicaid may be eligible for Medicare. Sharfstein said it’s going to be important for states to identify these people and to help them enroll in new coverage
plans. For people not yet eligible for Medicare, there will be a temporary special enrollment period for plans on HealthCare.gov. One change brought on by the pandemic that’s sticking
around, at least for now, is expanded telehealth. More than 28 million Medicare beneficiaries dialed into doctors’ appointments during the first year of the pandemic, a report from HHS
shows. New legislation extends telehealth benefits for Medicare beneficiaries through 2024. States already have “significant flexibility with respect to covering and paying for Medicaid
services delivered via telehealth,” HHS says. These flexibilities will remain in place. END OF EMERGENCIES DOESN’T MEAN END OF COVID-19 One thing that doesn’t end when the declarations do
is COVID-19, Sharfstein points out. Cases, deaths and hospitalizations have plummeted since the peak of the omicron surge last winter. Still, more than 1,100 Americans are dying each week
from COVID-19, federal data shows. People should “continue paying attention to the virus,” Sharfstein said. Stay up to date on your vaccines, he advises, watch out for symptoms, and test
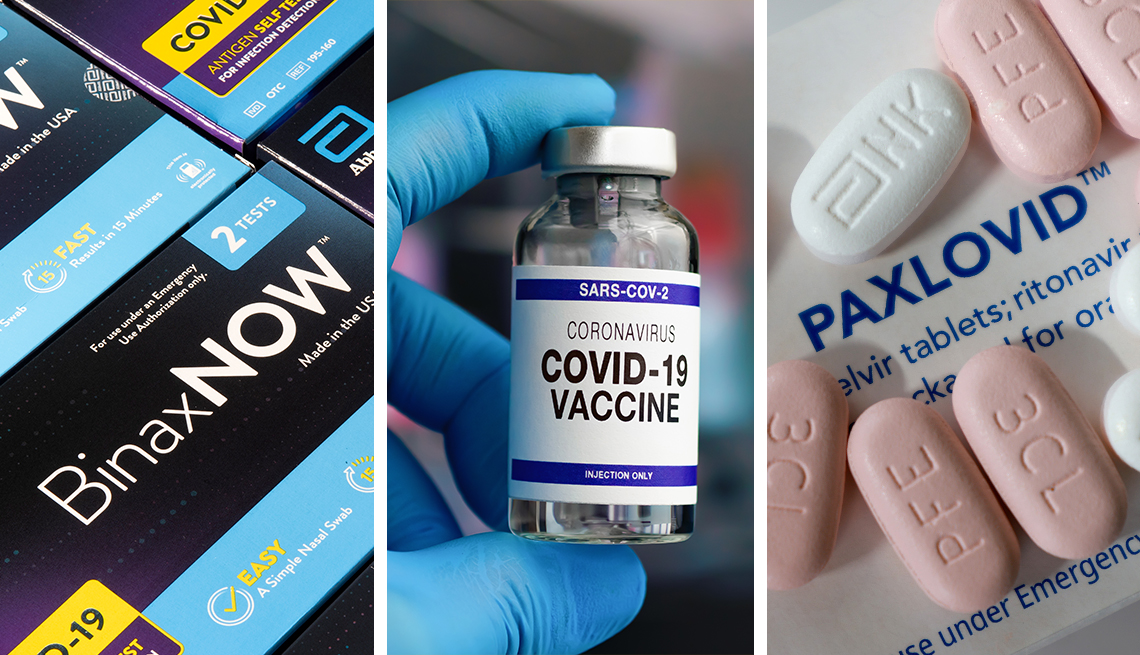
yourself if you’re going to be around vulnerable people. “The virus doesn’t care whether there’s a public health emergency declaration or not,” Sharfstein said. WHAT ABOUT EUAS? The FDA
confirmed on Jan. 31 that the ending of the public health emergency will not affect the agency’s ability to authorize devices (including tests), treatments or vaccines for emergency use.
“Existing emergency use authorizations (EUAs) for products will remain in effect and the agency may continue to issue new EUAs going forward when criteria for issuance are met,” the FDA said
in a tweet.