Play all audios:
ABSTRACT BACKGROUND Previous studies have reported inconsistent results regarding the association between poor dental health and pancreatic cancer risk. This study aimed to assess this
association using a well-functioning nationwide dental health registry in Sweden. METHODS Information of exposures (dental caries, root canal infection, mild inflammation, and periodontitis;
the number of teeth) was ascertained from the Swedish Dental Health Register, and occurrence of pancreatic cancer was identified from both cancer and cause of death registries. Hazard
ratios (HRs) were estimated using Cox models. RESULTS During a median of 7.2 years of follow-up, 10,081 pancreatic cancers were identified among 5,889,441 individuals. Compared with the
healthy status, a higher risk of pancreatic cancer was observed in individuals with root canal infection, mild inflammation, and periodontitis in the <50 age group (_P_ for trend
<0.001). In the 50–70 age group, only the subgroup with periodontitis had an excess risk (multivariable-adjusted HR = 1.20, 95% confidence interval [CI] 1.11–1.29). No positive
association with statistical significance was observed in the 70+ age group. Individuals with fewer teeth tended to have a higher risk in all age groups. CONCLUSIONS Our results confirmed
the association between poor dental health and pancreatic cancer risk, which warrants further studies on underlying mechanisms. SIMILAR CONTENT BEING VIEWED BY OTHERS IRANIAN EARLY CHILDHOOD
DENTAL CARIES: A COMPREHENSIVE SYSTEMATIC REVIEW AND META-ANALYSIS OF PREVALENCE AND ASSOCIATED RISK FACTORS Article 13 March 2025 ASSOCIATION BETWEEN ORAL HEALTH AND INCIDENCE OF
PNEUMONIA: A POPULATION-BASED COHORT STUDY FROM KOREA Article Open access 12 June 2020 INVESTIGATING THE LINK BETWEEN ORAL HEALTH CONDITIONS AND SYSTEMIC DISEASES: A CROSS-SECTIONAL ANALYSIS
Article Open access 26 March 2025 INTRODUCTION Pancreatic cancer is a lethal malignancy, with 5-year survival rate <9% [1]. Though the incidence is low, the number of new cases and of
deaths from pancreatic cancer are predicted to increase regionally and globally due to ageing populations [2]. Established risk factors include old age, male sex, chronic pancreatitis,
diabetes, obesity, tobacco smoking, and family history of pancreatic cancer [3, 4]. However, these risk factors explain only a fraction of pancreatic cancer cases, and other risk factors are
largely unknown yet. The oral cavity, as a gateway, including >700 species of bacteria, connects the gastrointestinal tract and the external environment [5]. Oral hygiene and lifestyle
factors have significant impact on the host microbiome [6]. Oral microbiome dysbiosis can augment progression of dental diseases and consequent tooth loss. Dental caries (dental plaque) is
initiated by the bacterial biofilm covering on the dental surface, without concurrent inflammation in surrounding tissues [7]. If left untreated, it can progress to pulpitis and apical
periodontitis that result in local inflammation [8]. Periodontal diseases (gum diseases), such as gingivitis, mild or advanced periodontitis, and periimplantitis, induce an inflammatory
response [9]. Gingivitis, the mildest form of periodontal disease, is caused by the bacterial biofilm that accumulates on teeth adjacent to the gums; it does not affect the underlying
supporting structures of the teeth and is reversible. Unlike gingivitis, periodontitis is the advanced stage of gum disease and involves loss of alveolar bone around the teeth, ultimately
leading to tooth loss if untreated [9]. Notably, emerging evidence indicates that myocardial infarction [10], diabetes [11], cancer risks [12,13,14], and cancer mortality [15] are related to
chronic microbial imbalance and systemic inflammation. To date, the evidence for the link between poor dental health and pancreatic cancer risk is not always consistent, partly due to
variations in study population, exposure measurement, and/or selection on adjusted confounding factors, and a lack of statistical power (Supplementary Table 1). Consequently, we aimed to
quantify the association between poor dental health, in particular inflammation related oral disorders, and the risk of pancreatic cancer based on the nationwide Dental Health Register in
Sweden. This registry provides continuous and good quality monitoring of dental health conditions of the vast majority of Swedish adult population [16]. METHODS STUDY DESIGN We included a
total of 5.9 million individuals older than 19 years with at least one dentist visit between 2009 and 2016. The unique personal identity numbers included in all Swedish registries were used
to follow all individuals in this dental health cohort through linkages to the Swedish Cancer Register, Cause of Death Register, and Total Population Register. Each individual was followed
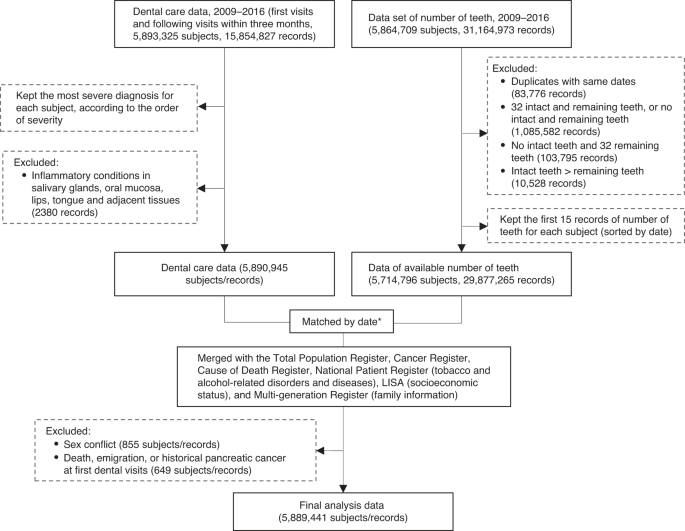
from entry at the first dental visit until outcome occurrence, death, migration out of Sweden, or end of follow-up (December 31, 2016), whichever came first. After excluding subjects with
pancreatic cancer, death and emigration at or before baseline, and conflicting information of sex between Total Population Register and Dental Health Register, we included 5,889,441
individuals with both information of dental diagnoses and the number of teeth in the final analysis cohort. The workflow for cohort assembly is shown in Fig. 1. ASSESSMENT OF EXPOSURES Based
on dental care data, we classified oral health conditions in teeth and their supporting tissues caused by dental biofilm (layers of microorganisms attached to the supragingival or
subgingival surface of a tooth) according to the severity of oral health damage and inflammation (Supplementary Table 2) [17] as healthy, caries, root canal infection, mild inflammation
(including gingivitis, pericoronitis, stomatitis, mucositis, and other unspecific inflammatory conditions), and periodontitis (including mild to advanced periodontitis, and periimplantitis
[18, 19]). Information on the number of teeth was also collected, and subjects were grouped according to the number of teeth at the first visit into categories (28–32, 25–27, 21–24, 15–20,
and 1–14 teeth); patients in whom this information was missing were categorised as “unknown” (Supplementary Methods). ASSESSMENT OF OUTCOME Reporting any diagnosis of cancer has been
mandatory for clinicians, cytologists, and/or pathologists in Sweden since 1958, and the overall completeness of the Swedish Cancer Register has been estimated at >98% [20]. However,
cancers without histopathological confirmation are less likely to be reported but may be reported to the Swedish Cause of Death Register, based on obligatory death certificates. Therefore,
we ascertained pancreatic cancer cases not only from the Cancer Register through the International Classification of Diseases version 7 (ICD-7: 157), but also from the Cause of Death
Register (underlying cause, ICD-7/8/9:157, ICD-10: C25), to compensate for underreporting of pancreatic cancer in the Cancer Register [21]. OTHER COVARIATES Individuals’ socioeconomic
background may serve as a potential confounder for the studied association, thus we obtained information about education level and family income from the Longitudinal Integration Database
for Health Insurance and Labour Market Studies (LISA). Education level was classified as (a) low, if the highest schooling was primary education 9 years and below, (b) medium, if 2 or 3
years of secondary schooling, (c) high, if postsecondary education and above, and (d) unknown information. Family income at baseline was categorised into three levels: low, medium, and high
among subjects aged 20–65 years and older than 65 years (retired) separately, using age-specific tertiles from the Swedish general population (Supplementary Table 3). Diagnoses of tobacco
abuse, and chronic obstructive pulmonary disease (as a proxy for smoking, Supplementary Table 4), and alcohol-related disorders and diseases (as a proxy for alcohol drinking, Supplementary
Table 4) were obtained from the National Patient Register by using ICD codes. With regard to family history of pancreatic cancer, all first-degree family members of individuals in this
cohort were linked to the Swedish Multi-generation Register by personal identity numbers, and then linked to the Swedish Cancer Register and Cause of Death Register to capture all pancreatic
cancer events. A Directed Acyclic Graph (DAG) for the list of potential confounders is shown in Supplementary Figure. STATISTICAL ANALYSIS We reported the baseline characteristics and
dental health-related factors (dental health status and number of teeth categories) of all individuals by age at entry into cohort (>19 and <50, ≥50 and <70, and ≥70 years). Cox
proportional hazards models were fitted to calculate hazard ratios (HRs) with 95% confidence intervals (CIs), to examine the association between poor dental health and the risk of pancreatic
cancer. We stratified age at baseline into the same three groups and fitted Cox models with attained age as the underlying time scale in each stratum. We selected healthy dental status and
≥28 teeth as the reference group, with adjustment for sex, calendar year of first visit, education, family income, family history of pancreatic cancer, smoking-related diseases, and
alcohol-related disorders and diseases. Furthermore, each model included both dental health status and number of teeth, so that our main exposures were always adjusted for each other. The
proportional hazards assumption was assessed by a Schoenfeld residual-based test, and no violation was observed. The Cochran–Armitage trend test was used to evaluate a possible trend of the
risk of pancreatic cancer across decreasing levels of dental health status (inflammation), and the number of teeth. We estimated interactions between age at baseline and poor dental health,
and between age at baseline and the number of teeth fit to the whole data (Supplementary Methods). These preliminary models suggested strong effect modification for both main exposures by
age at baseline, and this was no longer the case after stratifying the data by age at baseline. Therefore, we continued with the separate Cox models across this study. In a separate
analysis, we included an interaction term between dental inflammation (inflammation group includes mild inflammation and periodontitis; no inflammation group includes healthy, caries, and
root canal infection) and number of teeth in all three age-specific Cox models. This interaction was estimated by including a cross-product term between the binary dental inflammatory
condition (having inflammation or not) and the indicator variables for categories of number of teeth, and the null hypothesis of no interaction was assessed using a likelihood ratio test. In
sensitivity analyses, we explored the effects of multiple measurements during follow-up (time-varying exposures): for each participant, the most severe diagnosis of dental health status in
each calendar year was identified after baseline, and treated as a time-varying exposure. The follow-up period was split at progressive dates. Similarly, we identified any reduction in the
number of teeth during follow-up, and also included it as a time-varying exposure with split-follow-up time in the three age-stratified Cox models. We also included a one-year lag in the Cox
models as a sensitivity analysis, i.e. starting follow-up one year after the first visit, to minimise selection bias. Additionally, models were re-fitted while limiting the outcome to
incident cases from the Cancer Register only, i.e. excluding cases from the Cause of Death Register, to assess the possible effect of selective reporting of pancreatic cancer. Statistical
analyses were performed using Stata (Version 14; Stata Corp, College Station, TX, USA), and data visualisation was performed using R (Version 3.6.1; R Foundation for Statistical Computing,
Vienna, Austria). Two-sided _P_ < 0.05 was considered statistically significant. RESULTS In the main analyses, 5,889,441 individuals with median follow-up of 7.2 years were included. The
mean age at baseline was 53.7 years (Table 1). About 30% of all individuals had dental inflammatory conditions (mild dental inflammation or periodontitis), among whom more than one-third had
periodontitis. Individuals with periodontitis at baseline were older, more likely to be smokers, and had fewer teeth. Similarly, individuals with fewer teeth (1–14) at baseline were older,
had lower education level, family income, and more likely to be smokers and alcohol drinkers (Supplementary Tables 5 and 6). A total of 10,081 pancreatic cancer cases were identified during
follow-up. In our multivariable-adjusted model (Table 2), individuals <50 years with root canal infection had a 58% increased risk of pancreatic cancer than those with healthy dental
status at baseline (multivariable-adjusted HR = 1.58, 95% CI 1.10–2.28), while individuals with mild dental inflammation and periodontitis had a 35% (95% CI 6–72%) and 56% (95% CI 17–108%)
higher risk of pancreatic cancer, respectively, compared with the healthy reference (_P_ for trend <0.001). In the 50–70 age group, only individuals with periodontitis had a 20% increased
risk of pancreatic cancer (multivariable-adjusted HR = 1.20, 95% CI 1.11–1.29). Among individuals aged 70 years and older, HRs were around one (with CIs across one). We found that
individuals with fewer teeth tended to have an increased risk of pancreatic cancer in all three age groups (Table 3). Additionally, individuals in the 50–70 age group with unknown number of
teeth had a 33% increased risk of pancreatic cancer (multivariable-adjusted HR = 1.33, 95% CI 1.19–1.48) compared with those with full dentition. When number of teeth was treated as a
time-varying exposure, the results remain similar as in the baseline models (Supplementary Table 7). There were no interaction effects between dental inflammatory conditions and the number
of teeth in all age groups with statistical significance (Fig. 2). In the sensitivity analyses, when dental health status was treated as a time-varying exposure, an 8% increased cancer risk
(crude HR = 1.08, 95% CI 1.01–1.17) in the ≥70 age group was observed in individuals with periodontitis than the healthy reference (Supplementary Table 7). After adding a one-year lag since
baseline, the HRs were similar for both dental health status and the number of teeth (data not shown). When the outcome was limited to incident pancreatic cancer cases only, the results
changed marginally compared with the main analyses (data not shown). DISCUSSION In this nationwide Swedish registry-based cohort study in Sweden, we confirm that periodontitis increases the
risk of pancreatic cancer by 20–56% in adults under 70 years as compared with the dentally healthy individuals. Our results also provide new evidence that root canal infection appears to
increase the risk of pancreatic cancer, with risk in individuals younger than 50 years increased by up to 58%, similar to periodontitis. To our knowledge, this fact has not been reported
previously. Similarly, individuals with fewer teeth tended to have an excess risk of pancreatic cancer. Accumulating evidence supports periodontal pathogens are strongly linked to pancreatic
cancer. As previously shown by Michaud and colleagues [22], individuals with a high level of antibodies against _Porphyromonas gingivalis_ (>200 ng/ml) had a twofold higher risk of
pancreatic cancer than individuals with a low level of the antibodies (≤200 ng/ml). Fan et al. [23] also found that _Aggregatibacter actinomycetemcomitans_ was associated with a higher risk
of pancreatic cancer (odds ratio [OR] = 2.20, 95% CI 1.16–4.18); in contrast, phylum _Fusobacteria_ seemed to be associated with a decreased pancreatic cancer risk (OR = 0.94, 95% CI
0.89–0.99). The keystone pathogen hypothesis suggests that _Aggregatibacter actinomycetemcomitans_ and _Porphyromonas gingivalis_, may affect the inflammatory disease by proliferating,
remodelling and controlling commensal microbiome [19]. Oral commensals, on the other hand, do cause root canal infection, with cell necrosis and tissue destruction involving the supportive
tissues through the root canal that leads to apical periodontitis which in fact demonstrates a very similar periodontal pathogen profile [24]. Besides triggering systemic inflammation, the
pathogenic species may promote the production of nitrosamines, which are potential carcinogens [25], and the release of enzymes and other carcinogenic metabolites [26]. Notably, the
dissemination of these products can take place by several routes: (a) by entering the circulatory system via the perturbed periodontal tissues (oral–blood axis), (b) through the oral–gut
axis via saliva, or (c) via the lymphatic draining system, possibly also attributing to immune modulations in distant organs [27,28,29]. We observed a positive association between root canal
infection and pancreatic cancer risk among younger adults. Although this finding is new, it is not completely surprising: root canal infection often involves the apical periodontal tissues
around the root—clinically, the infection can persist for multiple years without any symptoms [8]. Notably, oral bacteria have been found in cystic precursors to pancreatic cancer [30], but
such precursor lesions could take up to ten years to become invasive. Although less explored, studies report that chronic apical periodontitis is associated with diabetes or cardiovascular
diseases [31, 32]. Translocated root canal microbiomes, either microbial DNA or live bacteria, are found in distant organs including thrombus aspirates of subjects with myocardial infarction
[33]. Future studies are warranted to confirm our findings. We performed stratified analysis by age, since the effects of periodontal diseases accumulate with age. Compared with younger
patients, uncontrolled lifetime periodontal diseases may have a greater impact on older patients [18]. However, an increased risk was observed between periodontitis and pancreatic cancer
risk among individuals aged younger than 70 years, but not in 70 years and older. Some studies have previously reported that for dental pathology, many older adult patients may often be left
untreated [18] due to overall health status. Therefore, it is possible that we grouped some older patients, who had compromised dental health but with no diagnosis/treatment records of
periodontal diseases, into the dentally “healthy” subgroup. This misclassification is likely to be limited to younger individuals. Tooth loss is a robust indicator of oral health, reflecting
lifetime accumulation of oral inflammation. In this study, we demonstrated that individuals with fewer teeth had an excess risk of pancreatic cancer. Several studies reported null or
non-statistically significant positive results about the association between the number of teeth and pancreatic cancer risk [6, 34, 35], and only one study in Finland reported a 63%
increased risk in male smokers with complete edentulism (lack of teeth) with statistical significance (HR = 1.63, 95% CI 1.09–2.46) [36]. Inconsistent results are partly due to heterogeneity
of the study populations, exposure ascertainment, confounding adjustment, and follow-up time. Compared with prior studies, the strengths of this study are the large unselected population,
and the detailed clinical information about exposures, although some subjects with financial distress may not seek dental health care when needed, due to partial out-of-pocket payment [16].
The study population consisted of subjects aged >19 years with at least one dental visit and data on oral health diagnoses and dental procedures in Sweden. The exposures of compromised
dental health used in this study were defined by diagnostic codes from the Dental Health Register (uniquely used in Sweden) [17], which indicates that the probability of false positives is
low. Another exposure, the number of teeth, which was captured from clinical examinations, is more accurate than self-reported data. In addition, the linkage to Swedish national registries
[37, 38] allowed us to control for confounding factors, such as socioeconomic status and some diseases. With regard to diabetes, longitudinal studies indicate a bidirectional relationship
between periodontitis and diabetes—that is, periodontitis worsens diabetes by increasing the inflammatory burden and enhancing insulin resistance, and vice versa [9, 11]. Diabetes is a risk
factor as well as a consequence of a tumour in the pancreas. Therefore, we did not adjust for diabetes in the Cox models. Moreover, we added a lag time (one year) after the start of
follow-up to minimise the potential risk of reverse causality or surveillance bias. It turned out that HRs were only marginally changed when excluding the first year of follow-up, which
indicates a minimal impact from such bias. Furthermore, when compared with general health care that addresses broad health conditions, dental care is limited to a much narrower field of
health care: oral diseases and concerns. Therefore, the surveillance bias is likely to be limited. The current study has some limitations. First, the longest follow-up period in this cohort
is eight years, thus we probably could not capture all potential cancer cases, as carcinogenesis from initiation to metastasis can last more than ten years [39]. However, the number of teeth
reflects the accumulation of oral inflammation over a lifetime, so we may be able to study late-occurring outcomes without an extended follow-up period. Another caveat to consider is the
definition of dental health conditions: since most oral-related diseases and concerns were dealt with in public and private dental clinics, and were assessed by many different dentists,
inter- and intra-observer variation is a reality. In addition, the registries did not contain data on lifestyle factors and medications, such as smoking, alcohol drinking, antibiotic or
anti-inflammatory treatment, thus we could not adjust for these variables directly; though we used proxies for smoking and alcohol drinking during analyses, residual confounding cannot be
ruled out. Having fewer teeth reduces masticatory ability, which may result in a less healthy diet [40, 41]; a diet with fewer vegetables and fibres and more cholesterol and calories,
increases the general risk of cancer [41]. In the current study, information about dietary habits was not available from any registry and was thus not included in the models. Nevertheless,
other studies have adjusted for covariates related to diet when conducting multivariable models, but the results changed little [34, 42, 43]. At last, this is a Swedish population-based
cohort and has limitations for generalisation. Other potential biases with minimal impact on risk are described in the Supplementary Discussion. In conclusion, this study offers supporting
evidence that periodontal disease and tooth loss are associated with increased risks of pancreatic cancer. The positive association between root canal infection and pancreatic cancer risk
among individuals younger than 50 years is a new finding. Further prospective studies that identify specific oral pathogenic bacteria which precede carcinoma development are warranted, and
these findings may also provide clues for non-invasive biomarkers that can be used to identify tumours at an early stage in high-risk populations. DATA AVAILABILITY The data that support the
findings of this study are not publicly available due to privacy and ethical restrictions. The data are available from the corresponding author WY on reasonable request. CODE AVAILABILITY
Scripts used to generate the results presented in this study are available from the corresponding author JY on reasonable request. REFERENCES * Siegel RL, Miller KD, Jemal A. Cancer
statistics, 2019. CA Cancer J Clin. 2019;69:7–34. Article PubMed Google Scholar * Foreman KJ, Marquez N, Dolgert A, Fukutaki K, Fullman N, McGaughey M, et al. Forecasting life expectancy,
years of life lost, and all-cause and cause-specific mortality for 250 causes of death: reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet.
2018;392:2052–90. Article PubMed PubMed Central Google Scholar * Rawla P, Sunkara T, Gaduputi V. Epidemiology of pancreatic cancer: global trends, etiology and risk factors. World J
Oncol. 2019;10:10–27. Article PubMed PubMed Central Google Scholar * Kleeff J, Korc M, Apte M, La Vecchia C, Johnson CD, Biankin AV, et al. Pancreatic cancer. Nat Rev Dis Prim.
2016;2:16022. Article PubMed Google Scholar * Escapa IF, Chen T, Huang Y, Gajare P, Dewhirst FE, Lemon KP. New insights into human nostril microbiome from the Expanded Human Oral
Microbiome Database (eHOMD): a resource for the microbiome of the human aerodigestive tract. mSystems. 2018;3:e00187-00118. Article Google Scholar * Huang J, Roosaar A, Axell T, Ye W. A
prospective cohort study on poor oral hygiene and pancreatic cancer risk. Int J Cancer. 2016;138:340–7. Article CAS PubMed Google Scholar * Verna L, Whysner J, Williams GM.
N-nitrosodiethylamine mechanistic data and risk assessment: bioactivation, DNA-adduct formation, mutagenicity, and tumor initiation. Pharm Ther. 1996;71:57–81. Article CAS Google Scholar
* Nair PN. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med. 2004;15:348–81. Article CAS PubMed Google Scholar * Kinane DF, Stathopoulou
PG, Papapanou PN. Periodontal diseases. Nat Rev Dis Prim. 2017;3:17038. Article PubMed Google Scholar * Wilson K, Liu Z, Huang J, Roosaar A, Axéll T, Ye W. Poor oral health and risk of
incident myocardial infarction: a prospective cohort study of Swedish adults, 1973-2012. Sci Rep. 2018;8:11479. Article PubMed PubMed Central Google Scholar * Lalla E, Papapanou PN.
Diabetes mellitus and periodontitis: a tale of two common interrelated diseases. Nat Rev Endocrinol. 2011;7:738–48. Article CAS PubMed Google Scholar * Shi J, Leng W, Zhao L, Deng C, Xu
C, Wang J, et al. Tooth loss and cancer risk: a dose-response meta analysis of prospective cohort studies. Oncotarget. 2018;9:15090–15100. Article PubMed Google Scholar * Maisonneuve P,
Amar S, Lowenfels AB. Periodontal disease, edentulism, and pancreatic cancer: a meta-analysis. Ann Oncol. 2017;28:985–95. Article CAS PubMed Google Scholar * Ndegwa N, Ploner A, Liu Z,
Roosaar A, Axéll T, Ye W. Association between poor oral health and gastric cancer: a prospective cohort study. Int J Cancer. 2018;143:2281–8. Article CAS PubMed Google Scholar * Heikkilä
P, But A, Sorsa T, Haukka J. Periodontitis and cancer mortality: Register-based cohort study of 68,273 adults in 10-year follow-up. Int J Cancer. 2018;142:2244–53. Article PubMed Google
Scholar * Ljung R, Lundgren F, Appelquist M, Cederlund A. The Swedish dental health register - validation study of remaining and intact teeth. BMC Oral Health. 2019;19:116. Article PubMed
PubMed Central Google Scholar * Yu, J. Etiology and early detection of pancreatic cancer. Stockholm: Karolinska Institutet; 2021. * The Dental and Pharmaceutical Benefits Agency.
Föreskrifter om ändring i Tandvårds- och läkemedelsförmånsverkets föreskrifter och allmänna råd (TLVFS 2008:1) om statligt tandvårdsstöd. 2020.
https://www.tlv.se/download/18.1c9ccc53176e89932171fccd/1610445393307/hslf_fs2020_28.pdf. Accessed 16 Apr 2022. * Scannapieco FA, Cantos A. Oral inflammation and infection, and chronic
medical diseases: implications for the elderly. Periodontol 2000. 2016;72:153–75. Article PubMed Google Scholar * Lamont RJ, Koo H, Hajishengallis G. The oral microbiota: dynamic
communities and host interactions. Nat Rev Microbiol. 2018;16:745–59. Article CAS PubMed PubMed Central Google Scholar * Barlow L, Westergren K, Holmberg L, Talback M. The completeness
of the Swedish Cancer Register: a sample survey for year 1998. Acta Oncol. 2009;48:27–33. Article PubMed Google Scholar * Kilander C, Mattsson F, Ljung R, Lagergren J, Sadr-Azodi O.
Systematic underreporting of the population-based incidence of pancreatic and biliary tract cancers. Acta Oncol. 2014;53:822–9. Article PubMed Google Scholar * Michaud DS, Izard J,
Wilhelm-Benartzi CS, You DH, Grote VA, Tjonneland A, et al. Plasma antibodies to oral bacteria and risk of pancreatic cancer in a large European prospective cohort study. Gut.
2013;62:1764–70. Article PubMed Google Scholar * Fan X, Alekseyenko AV, Wu J, Peters BA, Jacobs EJ, Gapstur SM, et al. Human oral microbiome and prospective risk for pancreatic cancer: a
population-based nested case-control study. Gut. 2018;67:120–7. Article CAS PubMed Google Scholar * Davanian H, Gaiser RA, Silfverberg M, Hugerth LW, Sobkowiak MJ, Lu L, et al.
Mucosal-associated invariant T cells and oral microbiome in persistent apical periodontitis. Int J Oral Sci. 2019;11:16. Article PubMed PubMed Central Google Scholar * Risch HA. Etiology
of pancreatic cancer, with a hypothesis concerning the role of N-nitroso compounds and excess gastric acidity. J Natl Cancer Inst. 2003;95:948–60. Article CAS PubMed Google Scholar *
Pushalkar S, Hundeyin M, Daley D, Zambirinis CP, Kurz E, Mishra A, et al. The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer
Discov. 2018;8:403–16. Article CAS PubMed PubMed Central Google Scholar * Schmidt TS, Hayward MR, Coelho LP, Li SS, Costea PI, Voigt AY, et al. Extensive transmission of microbes along
the gastrointestinal tract. Elife. 2019;8:e42693. Article PubMed PubMed Central Google Scholar * Konkel JE, O’Boyle C, Krishnan S. Distal consequences of oral inflammation. Front
Immunol. 2019;10:1403. Article CAS PubMed PubMed Central Google Scholar * Thomas RM, Jobin C. Microbiota in pancreatic health and disease: the next frontier in microbiome research. Nat
Rev Gastroenterol Hepatol. 2020;17:53–64. Article PubMed Google Scholar * Gaiser RA, Halimi A, Alkharaan H, Lu L, Davanian H, Healy K, et al. Enrichment of oral microbiota in early cystic
precursors to invasive pancreatic cancer. Gut. 2019;68:2186–94. Article CAS PubMed Google Scholar * Pérez-Losada FL, Estrugo-Devesa A, Castellanos-Cosano L, Segura-Egea JJ, López-López
J, Velasco-Ortega E. Apical periodontitis and diabetes mellitus type 2: a systematic review and meta-analysis. J Clin Med. 2020;9:540. Article PubMed PubMed Central Google Scholar *
Hernández-Ríos P, Pussinen PJ, Vernal R, Hernández M. Oxidative stress in the local and systemic events of apical periodontitis. Front Physiol. 2017;8:869. Article PubMed PubMed Central
Google Scholar * Pessi T, Karhunen V, Karjalainen PP, Ylitalo A, Airaksinen JK, Niemi M, et al. Bacterial signatures in thrombus aspirates of patients with myocardial infarction.
Circulation. 2013;127:1219–28,e1-6. Article CAS PubMed Google Scholar * Hiraki A, Matsuo K, Suzuki T, Kawase T, Tajima K. Teeth loss and risk of cancer at 14 common sites in Japanese.
Cancer Epidemiol Biomark Prev. 2008;17:1222–7. Article Google Scholar * Lee K, Lee JS, Kim J, Lee H, Chang Y, Woo HG, et al. Oral health and gastrointestinal cancer: a nationwide cohort
study. J Clin Periodontol. 2020;47:796–808. Article CAS PubMed Google Scholar * Stolzenberg-Solomon RZ, Dodd KW, Blaser MJ, Virtamo J, Taylor PR, Albanes D. Tooth loss, pancreatic
cancer, and _Helicobacter pylori_. Am J Clin Nutr. 2003;78:176–81. Article CAS PubMed Google Scholar * Ludvigsson JF, Svedberg P, Olén O, Bruze G, Neovius M. The longitudinal integrated
database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol. 2019;34:423–37. Article PubMed PubMed Central Google Scholar *
Socialstyrelsen. The National Patient Register. 2022. https://www.socialstyrelsen.se/en/statistics-and-data/registers/register-information/the-national-patient-register/. Accessed 25 May
2022. * Yachida S, Iacobuzio-Donahue CA. Evolution and dynamics of pancreatic cancer progression. Oncogene. 2013;32:5253–60. Article CAS PubMed Google Scholar * Joshipura KJ, Willett WC,
Douglass CW. The impact of edentulousness on food and nutrient intake. J Am Dent Assoc. 1996;127:459–67. Article CAS PubMed Google Scholar * Sheiham A, Steele JG, Marcenes W, Lowe C,
Finch S, Bates CJ, et al. The relationship among dental status, nutrient intake, and nutritional status in older people. J Dent Res. 2001;80:408–13. Article CAS PubMed Google Scholar *
Michaud DS, Joshipura K, Giovannucci E, Fuchs CS. A prospective study of periodontal disease and pancreatic cancer in US male health professionals. J Natl Cancer Inst. 2007;99:171–5. Article
PubMed Google Scholar Download references ACKNOWLEDGEMENTS We thank Pouran Almstedt for data management and all individuals who contributed data to our research. This project was
supported by a grant from the Swedish Cancer Society (grant number 2019-0264). JY is partly supported by a scholarship from the China Scholarship Council. The funding sources had no role in
the study design, execution, analyses, interpretation of the data, writing of the report, or decision to submit the manuscript. FUNDING Open access funding provided by Karolinska Institute.
AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, 171 77, Stockholm, Sweden Jingru Yu, Alexander Ploner, Ji Zhang
& Weimin Ye * Department of Dental Medicine, Karolinska Institutet, 171 77, Stockholm, Sweden Margaret Sällberg Chen & Gunilla Sandborgh-Englund * Tenth People’s Hospital, Tongji
University, 200 072, Shanghai, China Margaret Sällberg Chen * Academic Center for Geriatric Dentistry, Karolinska Institutet, 171 77, Stockholm, Sweden Gunilla Sandborgh-Englund * Department
of Epidemiology and Health Statistics & Key Laboratory of Ministry of Education for Gastrointestinal Cancer, Fujian Medical University, 350 122, Fuzhou, China Weimin Ye Authors * Jingru
Yu View author publications You can also search for this author inPubMed Google Scholar * Alexander Ploner View author publications You can also search for this author inPubMed Google
Scholar * Margaret Sällberg Chen View author publications You can also search for this author inPubMed Google Scholar * Ji Zhang View author publications You can also search for this author
inPubMed Google Scholar * Gunilla Sandborgh-Englund View author publications You can also search for this author inPubMed Google Scholar * Weimin Ye View author publications You can also
search for this author inPubMed Google Scholar CONTRIBUTIONS Study concept and design: JY, GS-E, and WY; obtained funding: WY; acquisition of data: JY, and WY; analysis of data: JY, AP, and
JZ; interpretation of data: JY, AP, GS-E, MSC, and WY; drafting of the manuscript: JY; critical revision of the manuscript: JY, AP, GS-E, MSC, and WY; study supervision: WY. All authors gave
their final approval and agree to be accountable for all aspects of the work. CORRESPONDING AUTHORS Correspondence to Jingru Yu or Weimin Ye. ETHICS DECLARATIONS COMPETING INTERESTS The
authors declare no competing interests. ETHICS APPROVAL AND CONSENT TO PARTICIPATE This study was approved by the Swedish Ethical Review Authority (approval number 2021-02491) and was
performed in accordance with the Declaration of Helsinki. CONSENT FOR PUBLICATION Since this was a strictly registry-based study, individual informed consent was not required. ADDITIONAL
INFORMATION PUBLISHER’S NOTE Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations. SUPPLEMENTARY INFORMATION SUPPLEMENTARY
MATERIAL RIGHTS AND PERMISSIONS OPEN ACCESS This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and
reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes
were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If
material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain
permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. Reprints and permissions ABOUT THIS ARTICLE CITE THIS
ARTICLE Yu, J., Ploner, A., Chen, M.S. _et al._ Poor dental health and risk of pancreatic cancer: a nationwide registry-based cohort study in Sweden, 2009–2016. _Br J Cancer_ 127, 2133–2140
(2022). https://doi.org/10.1038/s41416-022-02018-8 Download citation * Received: 14 April 2022 * Revised: 05 October 2022 * Accepted: 06 October 2022 * Published: 22 October 2022 * Issue
Date: 07 December 2022 * DOI: https://doi.org/10.1038/s41416-022-02018-8 SHARE THIS ARTICLE Anyone you share the following link with will be able to read this content: Get shareable link
Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative