Play all audios:
ABSTRACT STUDY DESIGN: Prospective study. OBJECTIVE: To evaluate the formation of venous gas bubbles following open-sea scuba dives in persons with chronic spinal cord injury (SCI) and in
able-bodied diving instructors (C) and to assess the risk for decompression sickness (DCS). SETTING: Field study at the Island of Krk, Croatia. METHODS: Gas bubbles were monitored with an
ultrasound scanner 40 min after surfacing. The probability of DCS (P(DCS)) was estimated from the recorded depth-time profile using a decompression model. RESULTS: Divers completed six dives
in 3 days using a modified Bühlmann decompression model, and none developed signs of DCS. Mean P(DCS) was similar in both groups, SCI (0.51±0.2%) and C (0.64±0.27%), and was seen to
increase with subsequent dives. Number of bubbles (bubbles per cm2) was low in both groups on all 3 days of diving. CONCLUSIONS: We have used the P(DCS) as a severity index of diving
exposure. Overall, the severity of exposure in SCI subjects was consistent with the range of typical recreational dives, suggesting that the diving profile used is very safe. SIMILAR CONTENT
BEING VIEWED BY OTHERS PHYSIOLOGICAL PARAMETERS AND THE USE OF COMPRESSION STOCKINGS IN INDIVIDUALS WITH SPINAL CORD INJURIES: A SCOPING REVIEW Article 11 January 2022 REHABILITATION
OUTCOME IN PEOPLE WITH SPINAL CORD INJURIES RESULTING FROM DIVING IN SOUTH KOREA Article 09 April 2022 RISK FACTORS OF VIDEO URODYNAMICS AND BLADDER MANAGEMENT FOR LONG-TERM COMPLICATIONS IN
PATIENTS WITH CHRONIC SPINAL CORD INJURY Article Open access 02 June 2024 INTRODUCTION Scuba diving started as a sport of the exceptionally adventurous and physically fit, but has become a
popular recreational activity that attracts both young and old, physically active, as well as sedentary people. All who participate expose themselves to the physical challenges and hazards
that are inherent to this activity. The health and fitness requirements required to become certified as a scuba diver vary, but in general appear to have become quite liberal. The annual
incidence of spinal cord injury (SCI) in the United States is approximately 40 cases per million population, or approximately 11 000 new cases each year. The number of people in the United
States in 2006 who have SCI has been estimated to be between 225 000 and 296 000 persons. Most injuries occur between the ages of 16 and 30 years. More than half of SCI individuals were
employed at the time of injury and many were actively involved in sports. In the post-injury period, many SCI individuals, mostly those with a lower level of injury,1 return to their jobs,
lead active lives and some even return to recreation and sports. However, the majority of persons with SCI are inactive and exhibit low levels of cardiovascular fitness,2 which is a major
independent risk factor for cardiovascular disease and premature mortality.3 It appears that the ordinary activities of daily living in SCI are not adequate to maintain cardiovascular
fitness.2 Historically, individuals with disabilities have been discouraged from pursuing scuba diving by physicians because of both real and perceived risks. Since the 1990 Americans with
Disabilities Act and the 1995 Disability Discrimination Act in Great Britain, dive opportunities for persons with disability have increased. According to a Survey of Scuba Diving for
Disabled Divers, over 50% of British dive clubs were involved in the training of disabled divers between 1998 and 2000. Of the 130 survey respondents who described themselves as disabled, 54
had SCI. One-third of them learned to dive before their injury and two-third learned post injury.4 There are concerns that diving may further damage the spinal cord, as there is a rare
spinal form of decompression sickness (DCS). Neurological abnormalities are presently the most serious decompression related problem in recreational divers requiring treatment. DCS is
purportedly due to gas bubbles that form in body tissues during or after decompression. The amount of inert gas taken up by tissues is influenced by dive depth and duration, as well on
regional blood perfusion. Two factors required for bubble formation are gas nuclei and supersaturation. The nature of nuclei is unknown, but they are most likely small, gas-filled bubbles
attached to the endothelium of blood vessels. These bubbles eventually lodge in the pulmonary circulation. Recently, several reports have indicated that a single dive to depths regularly
taken by recreational divers (∼30 meters of sea water) causes an asymptomatic reduction in cardiovascular function, brachial artery endothelial dysfunction and reduction in right and left
ventricle functional indices.5, 6, 7 Some of these changes were reversed by acute pre-dive administration of antioxidants.7 In addition to venous bubble formation during scuba diving,
persons with SCI are exposed to other stress factors, such as hypothermia, immersion induced shifts of the peripheral venous blood toward the central vascular compartment, hyperoxia,
hemoconcentration and psychological stress. To date, there is no evidence that the risk of DCS is increased in SCI. The purpose of this study was to compare the occurrence and degree of
post-dive venous gas bubbles in divers with disabilities and able-bodied controls. METHODS STUDY POPULATION A total of 13 divers participated, 6 with chronic SCI and 7 healthy male scuba
diving instructors (group C). Demographic and lung function data are shown in Table 1. The diving instructors composing group C had years of diving experience, with logged hours of diving
between 1000 and 3000. For SCI subjects to be included they had to be at least 5 years out from their SCI and should not have cardiovascular diseases or diabetes. Paraplegia was the result
of traffic injury in five subjects. These five became certified divers after becoming paraplegic. One SCI subject was paraplegic due to DCS, and had completed scuba training before injury.
Diving experience in the SCI group varied between 1 and 29 years and 5 and 70 h per year of diving. One of the SCI individuals was mild smoker (10–15 cigarettes a day). At the time of this
study, all subjects had a valid medical waiver for diving and were clear of any symptoms of acute illness. Both groups were moderately trained (personal observation). The study methods and
potential risks were explained in detail to participants who gave written informed consent before the experiment. SPIROMETRY Spirometry was performed in the seated position. In the group
with SCI, height was recorded by self recall, whereas weight was measured using a wheelchair scale with subjects sitting in their wheelchairs. Body fat index was calculated by the Jackson
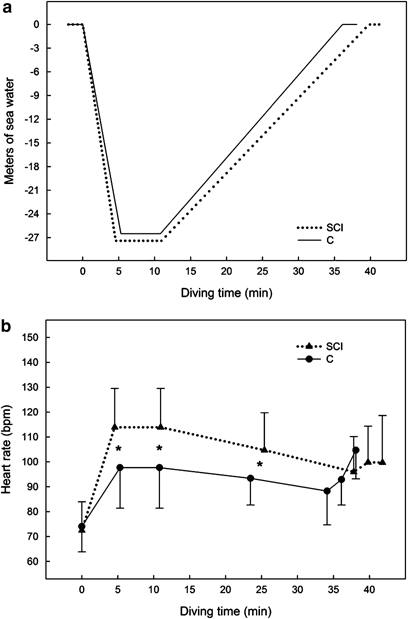
and Pollock three-site measurement method. DIVING PROTOCOL Divers were equipped with wet diving suits. All dives were performed according to the ZH-L8 ADT Bühlmann protocol, which is shown
in Figure 1. The study spanned over 3 days during which both groups performed two dives per day (six dives in total). Each SCI subject was accompanied during the dives by an assigned diving
instructor. One exception to this rule was a case where one diving instructor monitored two disabled individuals simultaneously, one being a very experienced, independent diver. The dive
pairs changed over 3 days. Dive depth was monitored with a dive computer (Galileo, Uwatec, Switzerland) interfaced with personal computer for later verification of the dive profile, sea
temperature, and heart rate (HR) of divers. Three divers in each group were equipped with a personal dive computer. During dives, no exercise was performed other than slow swimming. Bottom
sea temperatures were 15–17 °C for all dives, whereas air temperatures varied between 25 and 28 °C. POST-DIVE MONITORING AND BUBBLE ANALYSIS After completion of each dive, divers were
transported to an echocardiographic lab established on the beach 50 m from the shoreline. Beginning approximately 40 min after surfacing, with subjects in a supine position, venous gas
bubbles were monitored with a Logic Book XP scanner (GE, Milwaukee, WI, USA), using a phase array probe (1.5–3.3 MHz). Gas bubbles appeared in the right ventricle as high-intensity echoes
(Figure 2). Cardiac images were recorded to the computer's hard drive during 60 s of rest and after two coughs. Coughs were used because such a maneuver significantly increases the
number of bubbles detected.8 The quality of images obtained in all subjects was very good. We graded bubbles using the method described by Eftedal and Brubakk,9 which describes six grades:
0, no bubbles; 1, occasional bubbles; 2, at least one bubble every fourth heart cycle; 3, at least one bubble per cycle; 4, continuous bubbling, at least one bubble per cm2 in all frames and
5, ‘white-out’, individual bubbles cannot be seen (this grade has been observed in animals only). The grading system has been used extensively in several animal species, as well as in
human. After grading, the values were transferred to a linear scale (bubbles per cm2) as previously described.10 Bubbles were assessed twice after each dive and then integrated to give an
average bubble number per day. The risk of DCS was estimated from the recorded depth-time profile using a software application developed by W Gerth that implements the decompression model
LE1.11 The presence of patent foramen ovale in our subjects was checked by observing whether bubbles crossed the atrial septum following two coughs. STATISTICS The data are presented as
mean±standard deviation (s.d.). The comparison between groups was done using Student's _t_-test for paired and unpaired samples, using Statistica 7.0 software (Statsoft Inc., Tulsa, OK,
USA). The comparison of P(DCS) in repetitive diving was done using linear regression analysis (SAS by SAS Institute Inc., Cary, NC, USA). We certify that all applicable institutional and
governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. RESULTS SCI patients and able-bodied healthy males were matched for
age, but the SCI group was comprised of smaller and lighter individuals (Table 1). Body fat index was similar in SCI and C groups. All 13 divers successfully completed the protocol design
comprised of six dives in 3 consecutive days, and none developed any signs/symptoms of DCS. Average bottom depth and time during the dive was 26.9±2.9 m and 5.9±3.9 min, respectively (Figure
1a). Descent speed was ∼5.5 m min−1, whereas the ascent speed was ∼1.2 m min−1. On the surface there was no difference in HR between the groups. During the bottom phase and first half of
the ascent phase, SCI patients showed significantly higher HR (_P_=0.01, _P_=0.025, respectively; Figure 1b). Of 78 dives among 13 divers, bubbles were detected in all divers. The highest
grade detected was three in group C diver No. II, after his first day of diving. Average linearized bubble grade was similar for days 1 and 3 in both groups, whereas after day 2 diving
instructors showed a greater increase in gas bubbles formation (Table 2). Arterialization of bubbles (crossing of the atrial septum or passing through the lung) was not observed in any
diver. The estimated probability of DCS (P(DCS)) varied between 0.17 and 1.1%. Only two dives had a P(DCS) >1. The mean P(DCS) for SCI subjects (0.51±0.2%) was similar to mean P(DCS) for
able-bodied divers (0.64±0.27%; Figure 3). The P(DCS) was greater after repeat dives (Figure 4). DISCUSSION Peripheral circulation plays a major role in loading inert gases, generally
nitrogen, into body tissues during a dive and unloading them after a dive. When a diver is at rest under water, blood will redistribute to the central organs, whereas skeletal muscle will
receive little blood. As the visceral organs have a relatively high fat content, and nitrogen is more soluble in fat, more inert gas will be stored there. This process is also facilitated by
the immersion-induced centralization of peripheral blood.12 When a diver performs vigorous exercise underwater, as occurs during most recreational and professional dives, more blood will be
directed toward working skeletal muscles and theoretically more inert gas will accumulate in muscle.8 However, there is less fat in muscles than in the visceral organs, and therefore the
muscle stores less gas. If there are many bubble nuclei in exercising muscle, bubble growth will occur faster in this muscle despite the gas storage capacity being smaller. Circulation
changes in paraplegia may affect the risk of DCS. Due to paraplegia, the largest muscle group in the body, the leg, is inactive and takes up less inert gas during a dive. The upper
extremities have a higher gas uptake, as swimming is primarily performed by the arms. Based on measured HR changes during the bottom phase and during slow ascent, all subjects performed a
moderate level of exercise in this study (∼30–40% of the maximal oxygen uptake). Heart rate increased slightly more in SCI subjects, but this was expected, as these subjects have
significantly elevated HR values at every submaximal work stage in comparison to control subjects.13 In paraplegia, cold exposure during diving may trigger muscle spasticity and a general
reaction of autonomic nervous system with hypertension. In addition, SCI patients are at greater risk for disturbed heat balance during exercise in the cold than the able-bodied controls,14
and this may adversely affect the outcome of decompression post dive. On the other hand, immersion was shown to be beneficial in alleviating spastic attacks and it has been recommended as a
method to prevent spastic attacks.1 The present study is the first one known to monitor the occurrence of venous gas bubbles after scuba diving in SCI patients and able-bodied controls. We
found that the number of venous gas bubbles was rather low in both groups. The number of bubbles was quantified on a scale from 0 (no bubbles) to 5 bubbles per cm2 (‘white out’, individual
bubbles cannot be seen).9 The mean number of bubbles was ⩽0.1 in all six dives in both SCI and C groups. Although the number of venous bubbles is low, endothelial dysfunction of the brachial
artery may still occur,6 thus it is difficult to say definitively whether or not recreational diving is a safe sporting activity for SCI subjects. United States Navy divers with a higher
percentage of body fat were reported to have higher risk for DCS,15 although we could not confirm this finding.16 Furthermore, those who were aerobically more fit produced fewer bubbles
after diving.17 Body mass index (BMI) was not used in the present study as a marker of obesity in SCI subjects because it has been shown that BMI underestimates obesity. This underestimation
is due to potential measurement errors associated with measuring weight and height and because chronic SCI persons generally have greater fat mass and less fat-free mass per unit BMI than
age-matched able-bodied control subjects.18, 19 Greater fat mass may increase inert gas storage in the arms and legs of SCI subjects. Instead of BMI, we used a body fat index and
surprisingly found the body fat index was similar between the SCI and C groups. This finding was probably due to the high aerobic fitness level of our SCI subjects (personal observation).
Relatively low bubble grades found after scuba diving in SCI and C subjects in this study may be a result of the diving algorithm employed. The Bühlmann diving algorithm20 has been
considered safe for many years, and the duration of decompression with this procedure is considerably longer (up to 30–60%) than what is recommended both by the US Navy, the Norwegian
standard tables and the DCIM (Canadian) tables. For this study we used an adapted Bühlmann algorithm with a slower speed of descent (∼5 m min−1) and ascent (∼1 m min−1). This diving profile
is much more conservative than the usual recreational diving profile (descent rate 10 m min−1 and ascent rate 9 m min−1). With a slower compression phase, less inert gas will be accumulated
and with a prolonged decompression phase more gas will be eliminated, resulting in reduced DCS risk. In this study we used the P(DCS) as an index of diving exposure severity. There was no
difference in exposure severity between the two groups. The exposure was more severe on the second dive than on the first dive, suggesting a slightly higher risk. Overall, the severity of
exposure was in the range of most recreational dives. In conclusion, we suggest that chronic SCI subjects in good cardiovascular fitness may engage safely in recreational scuba diving if the
modified Bühlmann diving algorithm is used and if they dive in pair with diving instructors. Further studies are needed to investigate the acute and/or long-term effects of diving on
cardiovascular function in SCI subjects with lower cardiovascular fitness. REFERENCES * Steinbruck K, Paeslack V . Analysis of 139 spinal cord injuries due to accidents in water sports.
_Paraplegia_ 1980; 18: 86–93. CAS PubMed Google Scholar * Hoffman MD . Cardiorespiratory fitness and training in quadriplegics and paraplegics. _Sports Med_ 1986; 3: 312–330. Article CAS
PubMed Google Scholar * Blair SN, Brodney S . Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. _Med Sci Sports Exerc_ 1999;
31: S646–S662. Article CAS PubMed Google Scholar * Shelly S, Dowse ML, Bryson P . _The Report on the Data from the 1998–2000 Survey of Scuba Diving for Disable Divers_. Diving Disease
Research Center: Plymouth, 2002. Google Scholar * Dujic Z, Obad A, Palada I, Valic Z, Brubakk AO . A single open sea air dive increases pulmonary artery pressure and reduces right
ventricular function in professional divers. _Eur J Appl Physiol_ 2006; 97: 478–485. Article PubMed Google Scholar * Brubakk AO, Duplancic D, Valic Z, Palada I, Obad A, Bakovic D _et al_.
A single air dive reduces arterial endothelial function in man. _J Physiol_ 2005; 566: 901–906. Article CAS PubMed PubMed Central Google Scholar * Obad A, Palada I, Valic Z, Ivancev V,
Bakovic D, Wisloff U _et al_. The effects of acute oral antioxidants on diving-induced alterations in human cardiovascular function. _J Physiol_ 2007; 578: 859–870. Article CAS PubMed
Google Scholar * Flook V . The effect of exercise on decompression bubbles. A Theoretical Study. In: Mekjavic IB, Tipton MJ, Eiken O (eds). _Proceedings of the XXII Annual Scientific
Meeting of the European Underwater & Baromedical Society. Bled, Slovenia_, 1997, pp 55–61. * Eftedal O, Brubakk AO . Agreement between trained and untrained observers in grading
intravascular bubble signals in ultrasonic images. _Undersea Hyperb Med_ 1997; 24: 293–299. CAS PubMed Google Scholar * Nishi R, Brubakk AO, Eftedal O . Bubble detection. In: Brubakk AO,
Neumann TS (eds). _Bennet and Elliot's physiology and medicine of diving_, 5th edn. WB Saunders: London, 2003, pp 501–529. Google Scholar * Gerth WA, Vann RD . Comparison of bubble
dynamics and US Navy LE1 models as predictors of altitude decompression sickness. _Aviat Space Enviromen Med_ 1995; 66: A95. Google Scholar * Gabrielsen A, Johansen LB, Norsk P . Central
cardiovascular pressures during graded water immersion in humans. _J Appl Physiol_ 1993; 75: 581–585. Article CAS PubMed Google Scholar * Schneider DA, Sedlock DA, Gass E, Gass G .
VO2peak and the gas-exchange anaerobic threshold during incremental arm cranking in able-bodied and paraplegic men. _Eur J Appl Physiol Occup Physiol_ 1999; 80: 292–297. Article CAS PubMed
Google Scholar * Boot CR, Binkhorst RA, Hopman MT . Body temperature responses in spinal cord injured individuals during exercise in the cold and heat. _Int J Sports Med_ 2006; 27:
599–604. Article CAS PubMed Google Scholar * Dembert ML, Jekel JF, Mooney LW . Health risk factors for the development of decompression sickness among U.S. Navy divers. _Undersea Biomed
Res_ 1984; 11: 395–406. CAS PubMed Google Scholar * Dujic Z, Duplancic D, Marinovic-Terzic I, Bakovic D, Ivancev V, Valic Z _et al_. Aerobic exercise before diving reduces venous gas
bubble formation in humans. _J Physiol_ 2004; 555: 637–642. Article CAS PubMed PubMed Central Google Scholar * Carturan D, Boussuges A, Vanuxem P, Bar-Hen A, Burnet H, Gardette B .
Ascent rate, age, maximal oxygen uptake, adiposity, and circulating venous bubbles after diving. _J Appl Physiol_ 2002; 93: 1349–1356. Article CAS PubMed Google Scholar * Jones LM, Legge
M, Goulding A . Healthy body mass index values often underestimate body fat in men with spinal cord injury. _Arch Phys Med Rehabil_ 2003; 84: 1068–1071. Article PubMed Google Scholar *
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson Jr RN, Waters RL _et al_. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. _J Appl
Physiol_ 2003; 95: 2398–2407. Article PubMed Google Scholar * Buhlmann AA . Computation of low-risk compression. Computation model and results of experimental decompression research.
_Schweiz Med Wochenschr_ 1988; 118: 185–197. CAS PubMed Google Scholar Download references ACKNOWLEDGEMENTS We thank Dr JoAnn A Giaconi (University of California Los Angeles Jules Stein
Eye Institute Department of Ophtalmology, Los Angeles, CA, USA) for help with the preparation of the manuscript. We also thank Mr Branko Ravnak, president of IAHD Adriatic International and
International Societies Association IAHD Adriatic for their help and support. This study was supported by the Croatian Ministry of Science, Education and Sports, grant nos. 216-2160133-0130
and 216-2160133-0330. AUTHOR INFORMATION AUTHORS AND AFFILIATIONS * Department of Physiology, University of Split School of Medicine, Split, Croatia T Breskovic, I Palada, A Obad, Z Valic, D
Bakovic & Z Dujic * Department of Anesthesiology, Center for Hyperbaric Medicine and Environmental Physiology, Duke University Medical Center, Durham, NC, USA P Denoble * Department of
Internal Medicine, University Hospital Split, Split, Croatia D Glavas Authors * T Breskovic View author publications You can also search for this author inPubMed Google Scholar * P Denoble
View author publications You can also search for this author inPubMed Google Scholar * I Palada View author publications You can also search for this author inPubMed Google Scholar * A Obad
View author publications You can also search for this author inPubMed Google Scholar * Z Valic View author publications You can also search for this author inPubMed Google Scholar * D Glavas
View author publications You can also search for this author inPubMed Google Scholar * D Bakovic View author publications You can also search for this author inPubMed Google Scholar * Z
Dujic View author publications You can also search for this author inPubMed Google Scholar CORRESPONDING AUTHOR Correspondence to Z Dujic. RIGHTS AND PERMISSIONS Reprints and permissions
ABOUT THIS ARTICLE CITE THIS ARTICLE Breskovic, T., Denoble, P., Palada, I. _et al._ Venous gas bubble formation and decompression risk after scuba diving in persons with chronic spinal cord
injury and able-bodied controls. _Spinal Cord_ 46, 743–747 (2008). https://doi.org/10.1038/sc.2008.44 Download citation * Received: 30 November 2007 * Revised: 25 March 2008 * Accepted: 26
March 2008 * Published: 13 May 2008 * Issue Date: November 2008 * DOI: https://doi.org/10.1038/sc.2008.44 SHARE THIS ARTICLE Anyone you share the following link with will be able to read
this content: Get shareable link Sorry, a shareable link is not currently available for this article. Copy to clipboard Provided by the Springer Nature SharedIt content-sharing initiative
KEYWORDS * safe diving * decompression sickness * Doppler ultrasound